If Medicare denies a claim, you can file an appeal. You can file an appeal by submitting a Redetermination Request form to the company on the last page of your MSN. You can also write a letter to appeal Medicare’s decision.
How do I ask for a fast appeal for Medicare non coverage?
Your provider will give you a notice called a Notice of Medicare Non Coverage before your services end, telling you how to ask for a fast appeal. You should read this notice carefully. If you don’t get this notice, ask your provider for it. With a fast appeal, an independent reviewer will decide if your covered services should continue.
How do I appeal a Medicare decision?
The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal. Write your Medicare Number on all documents you submit with your appeal request.
How do I request a fast appeal?
Follow the directions on the IM to request a fast appeal if you think your Medicare-covered hospital services are ending too soon. You must ask for a fast appeal no later than the day you're scheduled to be discharged from the hospital.
What is the appeal process for KanCare state fair hearing?
The appeal process is for KanCare members currently receiving services from a MCO. The KanCare state fair hearing is processed by the Office of Administrative Hearings (OAH).

What is an expedited appeal in Medicare?
An expedited appeal is a fast appeal of an Original Medicare, Medicare Advantage, or Medicare Part D plan's denial of coverage when a person's “life, health, or ability to regain maximum function” is in jeopardy.
When a Medicare beneficiary requests a fast appeal of their discharge a decision must be reached within?
If you miss the deadline for an expedited QIO review, you have up to 60 days to file a standard appeal with the QIO. If you are still receiving care, the QIO should make its decision as soon as possible after receiving your request. If you are no longer receiving care, the QIO must make a decision within 30 days.
Can we send appeal to Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
How long does it take Medicare to respond to an appeal?
about 60 daysHow Long Does a Medicare Appeal Take? You can expect a decision on your Medicare appeal within about 60 days. Officially known as a “Medicare Redetermination Notice,” the decision may come in a letter or an MSN. Medicare Advantage plans typically decide within 14 days.
How successful are Medicare appeals?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What are the five steps in the Medicare appeals process?
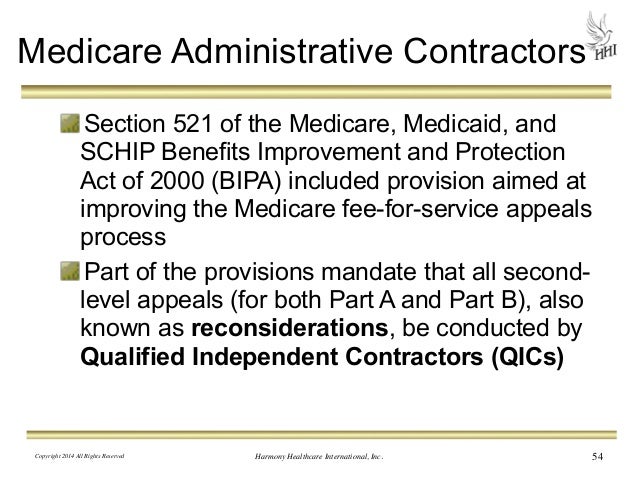
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
What is the timely filing limit for Medicare?
12 monthsMedicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share.
How long does Dwihn have to decide an expedited fast appeal request?
72 hours6. DWIHN has 72 hours from the receipt of the expedited MI Health Link first level request to review and make a determination and within 30 calendar days from receipt of the non-expedited MI Health Link first level internal/local appeal request to the enrollee.
How do I fight Medicare denial?
File your appeal within 120 days of receiving the Medicare Summary Notice (MSN) that lists the denied claim. Circle the item on your MSN that you are appealing and clearly explain why you think Medicare's decision is wrong. You can write on the MSN or attach a separate page.
Who pays if Medicare denies a claim?
The denial says they will not pay. If you think they should pay, you can challenge their decision not to pay. This is called “appealing a denial.” If you appeal a denial, Medicare may decide to pay some or all of the charge after all.
Who has the right to appeal denied Medicare claims?
You have the right to appeal any decision regarding your Medicare services. If Medicare does not pay for an item or service, or you do not receive an item or service you think you should, you can appeal. Ask your doctor or provider for a letter of support or related medical records that might help strengthen your case.
How do I appeal my Medicare Part B premium?
First, you must request a reconsideration of the initial determination from the Social Security Administration. A request for reconsideration can be done orally by calling the SSA 1-800 number (800.772. 1213) as well as by writing to SSA.