Can I submit a claim to Medicare myself?
What is the first step in submitting Medicare claims?
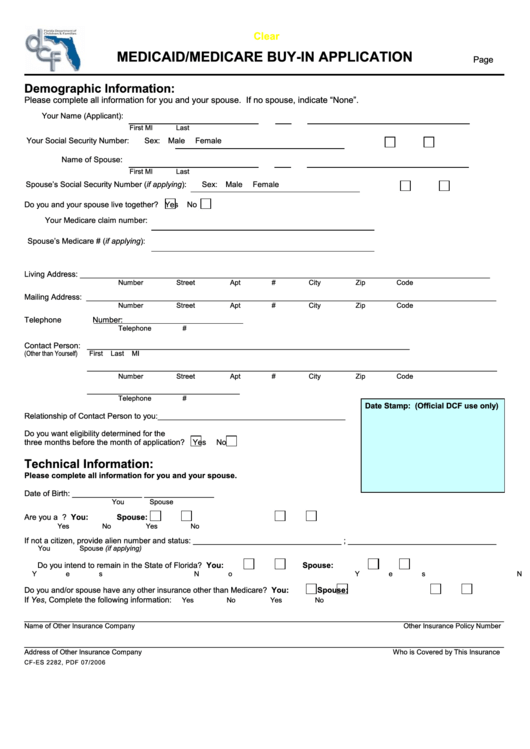
- The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ...
- The next step in filing your own claim is to get an itemized bill for your medical treatment.
What form is used to send claims to Medicare?
Do Medicare claims have to be submitted electronically?
How do I claim Medicare online?
How does Medicare reimbursement work?
What is the first step in submitting Medicare claims quizlet?
What is a 1500 form?
What is Medicare Part B claims address?
| Who to Write | Addresses and Additional Information |
|---|---|
| Appeals | |
| Claims | J15 — Part B/HHH Claims CGS Administrators, LLC PO Box 20019 Nashville, TN 37202 |
| Congressional Inquiries | CGS Administrators, LLC J15 Part A/B Correspondence PO Box 20018 Nashville, TN 37202 |
Does Medicare accept handwritten claims?
What is the difference between paper claims and electronic claims?
How long do you have to submit claims to Medicare?
How to file a claim for Medicare?
How to File a Medicare Claim Yourself. If you need to file your own Medicare claim, you’ll need to fill out a Patient Request for Medical Payment Form, the 1490S. Make sure it’s filed no later than 1 full calendar year after the date of service. Medicare can’t pay its share if the submission doesn’t happen within 12 months.
How to check Medicare claim status?
You can easily check the status of Medicare claims by visiting MyMedicare.gov; all you need to do is log into your account. Most claims are sent in within 24 hours of processing.
What to do if Medicare is denied?
If your Medicare claim is denied, you’ll want to file an appeal.
What is a claim number?
A claim number helps Medicare track your claim. This number is most likely your social security number with a letter after it.
How long does it take for Medicare to process a claim?
How Are Medicare Claims Processed? Your doctor will submit the claims. Then, Medicare will take about 30 days to process the claim. When it comes to Part A services, Medicare will pay the hospital directly. But, with Part B claims payment depends on whether or not the doctor accepts Medicare assignment.
Can a doctor submit a claim to Medicare?
But, in some instances, like foreign travel or doctors that don’t accept assignment, you’ll file the claim. If you receive an Advance Beneficiary Notice of Noncoverage and decide to proceed, it’s best to request your doctor submit the claim to Medicare before billing you.
Is Medicare always primary?
Medicare isn’t always primary. In this instance where Medicare is secondary, you’ll bill the primary insurance company before Medicare. Then, you can submit an Explanation of Benefits from the primary payor with the claim. The primary payer must process the claim first, and if they don’t, your doctor may bill Medicare.
How to file an original Medicare claim?
You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit. (Original Medicare providers have to give you an advance beneficiary notice ...
How long does it take to submit a claim to Medicare?
Original Medicare claims have to be submitted within 12 months of when you received care. Medicare Advantage plans have different time limits for when you have to submit claims, and these time limits are shorter than Original Medicare. Contact your Advantage plan to find out its time limit for submitting claims.
What is Medicare claim?
What is a Medicare claim? A claim asks Medicare or your insurer to pay for your medical care. Claims are submitted to Medicare after you see a doctor or are treated in a hospital. If you have a Medicare Advantage or Part D plan, your insurer will process claims on Medicare’s behalf.
How to file a complaint with Medicare?
You can file an Original Medicare claim by sending a Beneficiary Request for Medical Payment form and the provider’s bill or invoice to your regional Medicare Administrative Contractor (Here is a list of these broken down by state). Keep copies of everything you submit.
When to show Medicare card?
Show your health care provider your Medicare and Medicaid I.D. cards when you check in for your office visit. You should also show the provider your Medicaid managed care plan card (if you have one).
Do you have to bill your insurance if you have Medicare Advantage?
If you have Medicare Advantage, providers in the plan’s network have to bill your insurer for your care. As mentioned above, you may have to submit your own claims if you go out-of-network. If you decide to file a claim yourself, first contact your insurer for its claims mailing address and any forms to include with your claim.
Do you have to give advance beneficiary notice to Medicare?
Keep copies of everything you submit. (Original Medicare providers have to give you an advance beneficiary notice (ABN), Home Health Advance Beneficiary Notice, or Skilled Nursing Advance Beneficiary Notice if they believe Medicare will not cover your care. Providers normally will not bill Medicare after they issue an ABN.
How long do you have to file a Medicare claim?
As a beneficiary, you have one calendar year after receiving medical services to file your Medicare claim. If you file your claim after 12 months has elapsed, it will probably be rejected.
What is the Medicare website?
The Medicare website contains information sheets detailing the specific requirements for these specialized claim types.
How often do you check your Medicare summary notice?
Check your Medicare Summary Notice issued every month to see whether you have outstanding claims. In most cases, your health provider will resolve these if you bring them to their attention. However, if they are unable to or simply refuse, you will need to file your own Medicare claim. 1.
Do you need to include supporting documents in Medicare?
This could be for any of the reasons discussed above. In addition, you should include any documents that can support your claim.
Is a diagnosis needed on an itemized bill?
Your specific diagnosis. This may not be necessary on the itemized bill if your Patient’s Request for Medical Payment form contains a thorough illness or injury description
How long do you have to file a Medicare claim?
You have 1 year to file your Medicare claim after receiving services covered by Medicare as a beneficiary. Your claim may be rejected if you wait longer. Contact a Medicare representative if you have other questions regarding your claim. You can log into your MyMedicare account to check the status of your claim.
How often do you get a Medicare summary notice?
People with original Medicare (parts A and B) may need to file their own claims if their healthcare provider: If you have original Medicare, you’ll receive a Medicare summary notice in the mail every 3 months. This notice will detail your Medicare plans and costs.
Do you have to file a claim with Medicare Advantage?
Medicare-approved providers usually send claims directly to Medicare so that you won’t need to. And people with Medicare Advantage (Part C) don’t need to file claims at all because the private insurance companies that offer these plans are paid by Medicare each month.
Do you need to add supporting documents to your claim?
You’ll need to add any supporting documents to your claim after getting an itemized bill for your treatment.
Can I file a Medicare claim online?
You must file your Medicare claim by mail. There isn’t an option to file your Medicare claim online. According to Medicare.gov, you may find the address for where to send your claim in two places: on the second page of the instructions for filing a claim, listed as “How do I file a claim?”.
How Do I File a Medicare Reimbursement Claim?
To file your claim, you’ll need to fill out a Patient’s Request for Medical Payment form. You then send both this form and the bill from your provider to your state’s Medicare contractor.
What To Submit With The Claim
When filling out the form, you must choose the service type then provide the following information:
Where to Send Your Medicare Claim
Each state has a different address to send your claim. There are two places where you can find the address. You can find the address on the claim form on page two, or on your quarterly Medicare Summary Notice.
What if My Healthcare Provider is Not Sending the Claims Promptly?
The first thing you should do is call the provider and ask them to send your claim. If they do not file the claim, call Medicare and find out how much time is left to file the claim. If it’s close to the end of the allowed time and your healthcare provider has not filed the claim, you should go ahead and file the claim.
FAQs
When a claim is submitted to Medicare, it should come straight from the doctor or other provider of services. If for some reason they don’t submit the claim on your behalf, then you can call Medicare and submit it yourself. You can also submit the claim online.
What Is a Medicare Claim?
Medicare claims ask Medicare or your insurer to pay for medical services or care you have received. In almost all cases, your doctor or a hospital where you received care will send the claim directly to Medicare if you are covered by Medicare Part A or Part B.
When Do You Need to File a Medicare Claim?
You generally shouldn’t have to worry about filing a Medicare claim yourself. But in some rare cases, you may have to file one on your own.
How to File a Medicare Claim
If you ever have to file a Medicare claim, you will need to fill out a special form and provide other detailed information to Medicare and/or your private insurer.
How to appeal Medicare summary notice?
If you have Original Medicare, start by looking at your " Medicare Summary Notice" (MSN). You must file your appeal by the date in the MSN. If you missed the deadline for appealing, you may still file an appeal and get a decision if you can show good cause for missing the deadline.
How long does it take to get a decision from Medicare?
Any other information that may help your case. You’ll generally get a decision from the Medicare Administrative Contractor within 60 days after they get your request. If Medicare will cover the item (s) or service (s), it will be listed on your next MSN. Learn more about appeals in Original Medicare.
What is an appeal in Medicare?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: • A request for a health care service, supply, item, or drug you think Medicare should cover. • A request for payment of a health care service, supply, item, ...
How long does Medicare take to respond to a request?
How long your plan has to respond to your request depends on the type of request: Expedited (fast) request—72 hours. Standard service request—30 calendar days. Payment request—60 calendar days. Learn more about appeals in a Medicare health plan.
How long does it take to appeal a Medicare denial?
You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination. If you miss the deadline, you must provide ...
How long does it take for a Medicare plan to make a decision?
The plan must give you its decision within 72 hours if it determines, or your doctor tells your plan, that waiting for a standard decision may seriously jeopardize your life, health, or ability to regain maximum function. Learn more about appeals in a Medicare health plan.
What to do if you decide to appeal a health insurance plan?
If you decide to appeal, ask your doctor, health care provider, or supplier for any information that may help your case. See your plan materials, or contact your plan for details about your appeal rights.