How do I find Medicare providers who have opted out?
Search this database by first name, last name, National Provider Identifier (NPI), specialty, or ZIP code to find providers who've opted out of Medicare. Enter at least one field to start your search. You can also download a national list of providers who’ve opted out of Medicare.
What are the out-of-pocket costs of Medicare?
Medicare includes a number of out-of-pocket costs such as deductibles, coinsurance and copayment. See a full breakdown and learn ways you could save. Nothing in life is completely free, and that’s true for Medicare.
What is the best way to pay for Medicare online?
However, paying online via the MyMedicare.gov website is one of the best options because it’s free and secure. It’s also fast, with payments usually processed in five business days.
How long does a doctor have to opt out of Medicare?
A doctor or other provider who chooses to opt out must do so for 2 years, which automatically renews every 2 years unless the provider requests not to renew their opt out status. When you get care from a provider who's opted out of Medicare:

Can I view my Medicare EOB online?
Your explanation of benefits, also called an EOB, is an important tool to help you keep track of your plan usage. Every time you get a new Medicare medical or Part D prescription coverage explanation of benefits, you can save time and paper by signing up to view them online.
Can I view my Medicare Summary Notice Online?
Yes, Medicare summary notices are available online — but you must sign up to receive them electronically. If you opt for electronic notices, you'll stop receiving printed copies of your MSNs in the mail. Instead, you'll get an email every month from your online My Medicare Account.
How do I get my yearly Medicare statement?
If you have lost your MSN or you need a duplicate copy, call 1-800-MEDICARE or go to your account on www.mymedicare.gov.
How do I get my Medicare summary online?
Log into (or create) your Medicare account. Select "Get your Medicare Summary Notices (MSNs) electronically" under the "My messages" section at the top of your account homepage. You'll come to the "My communication preferences" page where you can select "Yes" under "Change eMSN preference," then "Submit."
Where do I find my Medicare explanation of benefits?
claims:Check your Explanation of Benefits (EOB). Your Medicare drug plan will mail you an EOB each month you fill a prescription. ... Use Medicare's Blue Button by logging into your secure Medicare account to download and save your Part D claims information. ... For more up-to-date Part D claims information, contact your plan.
Are Medicare statements available online?
Get your “Medicare Summary Notices” electronically (also called “eMSNs”) For anyone with Original Medicare Part A or Part B, eMSNs contain the same information as paper MSNs. You can sign up for eMSNs by creating or logging into your Medicare account.
Do you get a 1095 form if you are on Medicare?
If you were enrolled in Medicare: For the entire year, your insurance provider will not send a 1095 form. Retirees that are age 65 and older, and who are on Medicare, may receive instructions from Medicare about how to report their health insurance coverage.
Does Medicare send a year end statement?
At the end of each year, Medicare sends a 1095-B statement. This statement shows the IRS a person had qualifying health insurance that year. An individual may receive more than one statement if they have a secondary insurance policy.
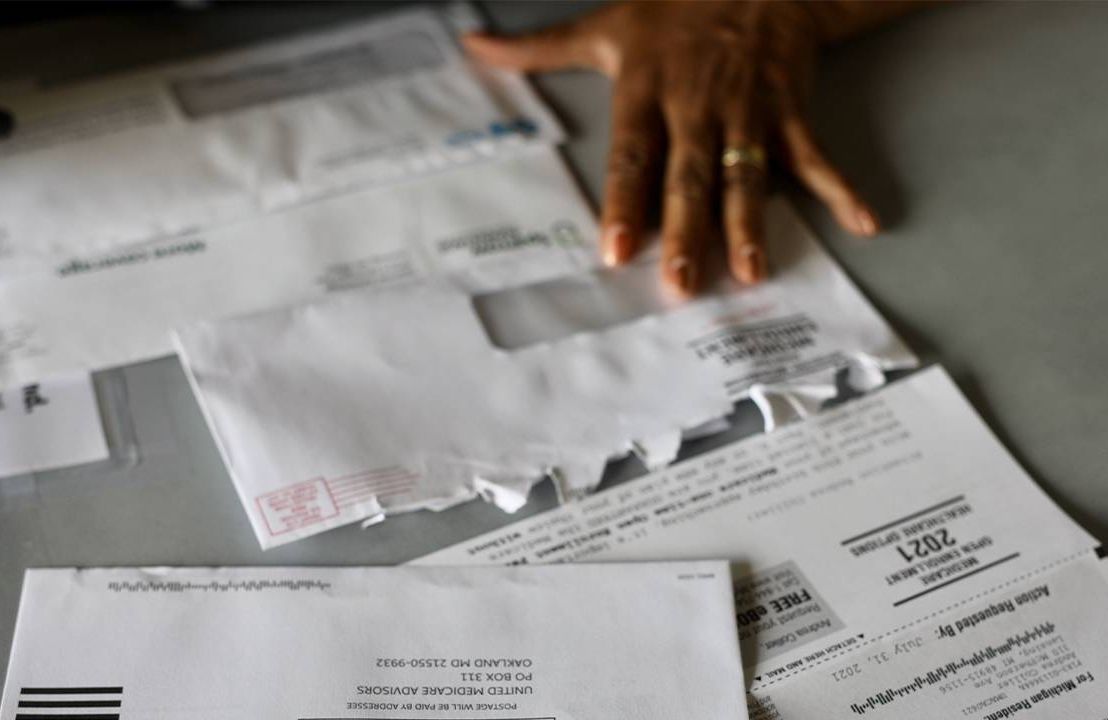
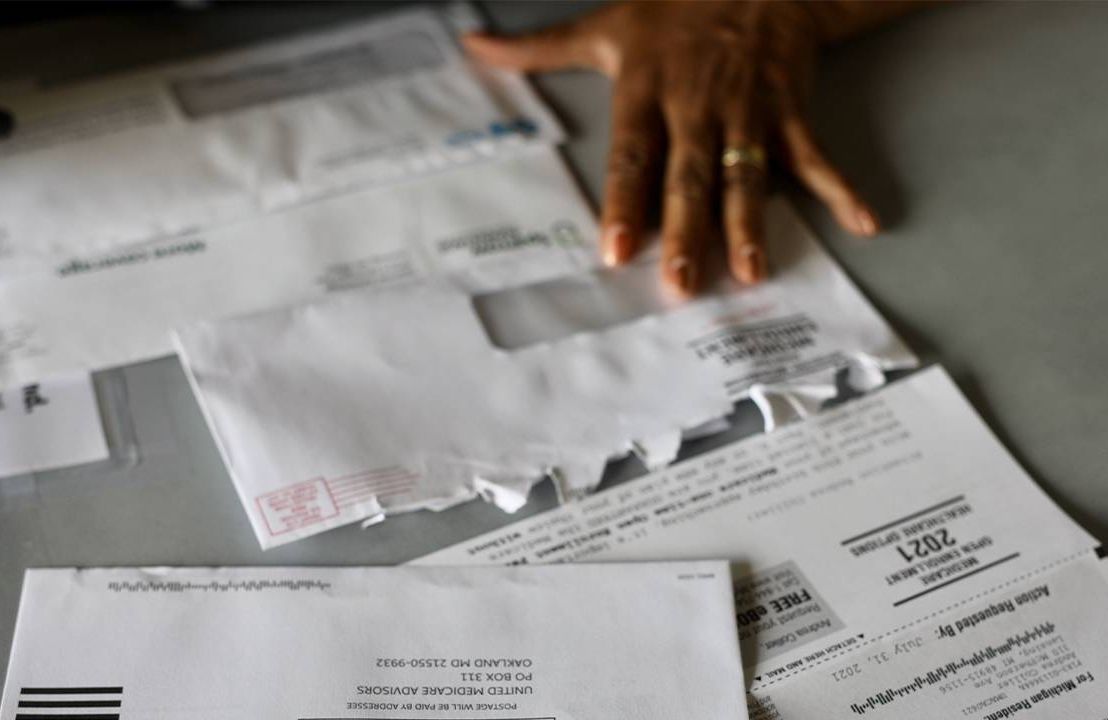
Does Medicare send statements?
It's a notice that people with Original Medicare get in the mail every 3 months for their Medicare Part A and Part B-covered services. The MSN shows: All your services or supplies that providers and suppliers billed to Medicare during the 3-month period.
What is Medicare summary?
The Medicare Summary Notice, also called an MSN, is a report of doctor visits, services or supplies billed to Medicare in your name. It is mailed every 3 months and is also available online.
How long keep Medicare summary notices?
1 to 3 yearsMedicare generally recommends that you keep notices for 1 to 3 years. It's extremely unusual that Medicare would follow up on anything older than that. In any case, Medicare ought to have copies of your records.
How much can you save if you don't accept Medicare?
If you are enrolled in Original Medicare, avoiding health care providers who do not accept Medicare assignment can help you save up to 15 percent on excess charges. Read additional medicare costs guides to learn more about Medicare costs and how they will affect you.
How much is Medicare Part B?
Part B. The standard Medicare Part B premium is $148.50 per month. However, the Part B premium is based on your reported taxable income from two years prior. The table below shows what Part B beneficiaries will pay for their premiums in 2021, based off their 2019 reported income. Medicare Part B IRMAA.
What is a Medigap plan?
These plans, also known as “ Medigap ,” provide coverage for some of Medicare’s out-of-pocket costs, such as deductibles, coinsurance and copayments. Some Medigap plans even include annual out-of-pocket spending limits. Sign up for a Medicare Advantage plan.
How much coinsurance is required for hospice?
A 5 percent coinsurance payment is also required for inpatient respite care. For durable medical equipment used for home health care, a 20 percent coinsurance payment is required.
What is Medicare Part D based on?
Part D premiums also come with an income-based tier system that uses your reported income from two years prior, similar to how Medicare Part B premiums are calculated. Part D premiums for 2021 will be based on reported taxable income from 2019, and the breakdown is as follows: Medicare Part D IRMAA. 2019 Individual tax return.
Do you have to pay coinsurance on Medicare?
Medicare coinsurance and copayments. Once you meet your deductible, you may have to pay coinsurance or copayments when you receive care. A coinsurance is a percentage of the total bill, while a copayment is a flat fee.
Does Medicare Advantage have a deductible?
Plans that offer prescription drug coverage may have a separate deductible for drug coverage and another deductible for the plan’s other benefits. Not all Medicare Advantage plans include a deductible.
Do you have to pay out of pocket for Medicare?
Whether you’re covered through Original Medicare or a Medicare Advantage Plan, there are some costs and expenses you’ll need to pay out-of-pocket, even after you pay your monthly premium. Your actual out-of-pocket costs depend on the exact Medicare coverage you have, your health care needs, your prescriptions, and how often you need health care ...
Can you compare out of pocket costs with Medicare?
You can compare estimated out-of-pocket costs side-by-side for various Medicare coverage combinations. For example, you can compare your costs with Original Medicare plus a Medigap policy plus a Medicare prescription drug plan, versus your costs with a Medicare Advantage Plan with drug coverage.
What to do if you don't receive Medicare?
If you don’t receive these benefits, you’ll need to decide how to pay your Medicare premium bill (in which case, you may need to use Form CMS-500 ). There are several payment options, including sending a check or money order, mailing your credit card information or using your bank’s payment service.
When is Medicare payment due?
You’ll have your payment due on the 25th of the month, so pay early to allow processing time. Whether you prefer making individual payments or enjoy the convenience of automated payment options, Medicare's online portal has you covered.
How often do you get Medicare premiums?
If you only have Medicare Part B and don’t get your Part B premiums deducted from your benefits, you’ll receive a premium bill every three months . If you have to buy Part A or owe Part D income-related monthly adjustment amounts (IRMAA), you’ll get a monthly premium bill.
Can you save on Medicare Supplement?
Learn How to Save on Medicare. Medicare Supplement Insurance plans (also called Medigap) can’t cover your Medicare premiums, but they can help make your Medicare spending more predictable by paying for some of your other out-of-pocket costs such as Medicare deductibles, copayments, coinsurance and more.
Does Medicare Easy Pay work?
Medicare Easy Pay is another payment option available to MyMedicare members. This program costs nothing to use, and it automatically deducts premiums from your checking or savings account when they’re due, ensuring you maintain continuous coverage. You’re also able to view your premium payment history online with Easy Pay.
What is Medicare out of pocket?
Original Medicare (Part A and Part B) is the federal health insurance program for people age 65 and older and individuals with certain disabilities. Although Original Medicare provides comprehensive coverage, it still leaves some out-of-pocket costs to recipients.
How much is Medicare Part A coinsurance for 2021?
In 2021, your Medicare Part A coinsurance for inpatient hospital care is as follows: Days 1-60: $0 coinsurance for each benefit period. Days 61-90: $371 coinsurance per day of each benefit period. Days 91 and beyond: $742 coinsurance per each lifetime reserve day after day 90 for each benefit period ...
What is coinsurance in Medicare?
Coinsurance is the percentage of costs you pay for health care expenses after your deductible is met. In most cases, your Medicare Part B coinsurance is 20 percent of the cost of Medicare-approved services. In 2021, your Medicare Part A coinsurance for inpatient hospital care is as follows:
What is the deductible for Medicare Part A in 2021?
In 2021, the deductible for Medicare Part A is $1,484 per benefit period , and the deductible for Medicare Part B is $203 per year.
How many Medigap plans are there?
Medicare Supplement Insurance provides full or partial coverage for some of the out-of-pocket expenses listed above. There are currently 10 standardized Medigap plans available in most states, and each includes a unique blend of basic benefits.
How much is the deductible for Medicare 2021?
If you became eligible for Medicare. + Read more. 1 Plans F and G offer high-deductible plans that each have an annual deductible of $2,370 in 2021. Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year.
Is Plan F available for Medicare?
Important: Plan F and Plan C are not available to beneficiaries who became eligible for Medicare on or after January 1, 2020. All 10 standardized Medigap plans provide at least partial coverage for: Medicare Part A coinsurance and hospital costs. Medicare Part B coinsurance or copayment. First three pints of blood.
How much does Medicare pay for 91 days?
For 91 days or more, $682 per day or full cost of stay. Medicare also provides 60 “lifetime reserve days” that beneficiaries can use if they need to stay in a hospital for more than 90 days. These can only be used once. Part B: Typically, 20 percent of the Medicare-approved cost of the service for most services.
How much does Medicare pay for a hospital stay?
Part A: No fee for hospital stays of 60 days or less. For 61 to 90 days, $341 per day. For 91 days or more, $682 per day or full cost of stay. Medicare also provides 60 “lifetime reserve days” that beneficiaries can use if they need to stay in a hospital for more than 90 days. These can only be used once.
How much will Medicare Advantage cost in 2021?
If you sign up for a Medicare Advantage plan that includes prescription drugs with a mid-priced premium, CMS predicts you’ll pay $4,339 in 2021. These are just estimates, of course, but they can help you choose the policy that’s best for your health care needs and financial situation.
How often does the Medicare tab swing?
And the tab can swing wildly each year, depending on the state of a beneficiary’s health, where he or she lives, and whether the government and insurers have instituted any price increases — or decreases. Individual plans can also tinker with the services and drugs they cover.
Does Medicaid pay out of pocket?
If you qualify for Medicaid, the federal-state health insurance program for people with low incomes and individuals with disabilities, it will pay some or all of your out-of-pocket expenses. Individuals on both Medicare and Medicaid are known as “dual eligibles.”.
Does Medicare have out of pocket costs?
Medicare’s out-of-pocket costs — premiums, deductibles, copays and coinsurance — can easily result in a large tab each year. If you’re struggling to meet those expenses, you might be eligible for federal and state assistance. If you qualify for Medicaid, the federal-state health insurance program for people with low incomes ...
General out-of-pocket costs
Most every insurance has the following out-of-pocket elements. Medicare also imposes penalties for signing up too late for Part B or Part D. All rates below are for 2021.
Provider-based expenses
Your out-of-pockets are directly affected by the healthcare provider you see. Make sure you take this into consideration before you schedule any appointments.
Hospital-based expenses
Staying overnight in a hospital does not necessarily mean you are admitted as an in -patient. You pay for inpatient hospital stays with a Part A deductible and a 20% Part B coinsurance for any physician services. When you are placed under observation, Part B provides your only coverage.
How much do Medicare beneficiaries pay in out-of-pocket costs?
According to the Kaiser Family Foundation, the average Medicare beneficiary spent $5,460 in total out-of-pocket costs in 2016.
Seven ways to minimize out-of-pocket costs
You cannot avoid all out-of-pocket costs, but you can do your best to minimize them. Most importantly, you can plan and anticipate them so you can avoid surprise medical bills. Here’s what you can do:
1. Sign up on time
Enroll in Medicare on time to avoid late penalties, especially because you could get stuck paying some of those penalties for as long as you have Medicare coverage. It is important to not miss these deadlines.
2. Pick the right Medicare doctors
Choose doctors – whenever possible – who not only accept Medicare for payment but who also “accept assignment.” This means they signed a contract to charge no more than Medicare-approved rates for their services.
3. Ask about your hospital orders
Not all hospital stays are billed the same – even when you stay overnight. Ask your doctor about your orders, inpatient or observation, when you stay in the hospital.
4. Watch for billing errors
Check your Medicare bills for accuracy. Paying for services that were never provided or for other billing errors is wasteful. Do not hesitate to reach out to your doctor’s billing office if you have questions or concerns.
5. Consider Medicare supplement plans
Consider a Medicare supplement plan – also known as Medigap – to save on expenses not covered by Original Medicare. Depending on the plan you choose, they can help to cover your Part A deductible, Part A/B coinsurance, and even healthcare you receive in a foreign country.