Medicare Part B premium payments through the online portal, EZ Receipts app or by fax or mail. Upon approval, you will receive reimbursement by direct deposit or check depending how you set up your account. Each member in your household with Medicare Part A and B is eligible to receive this benefit.
Full Answer
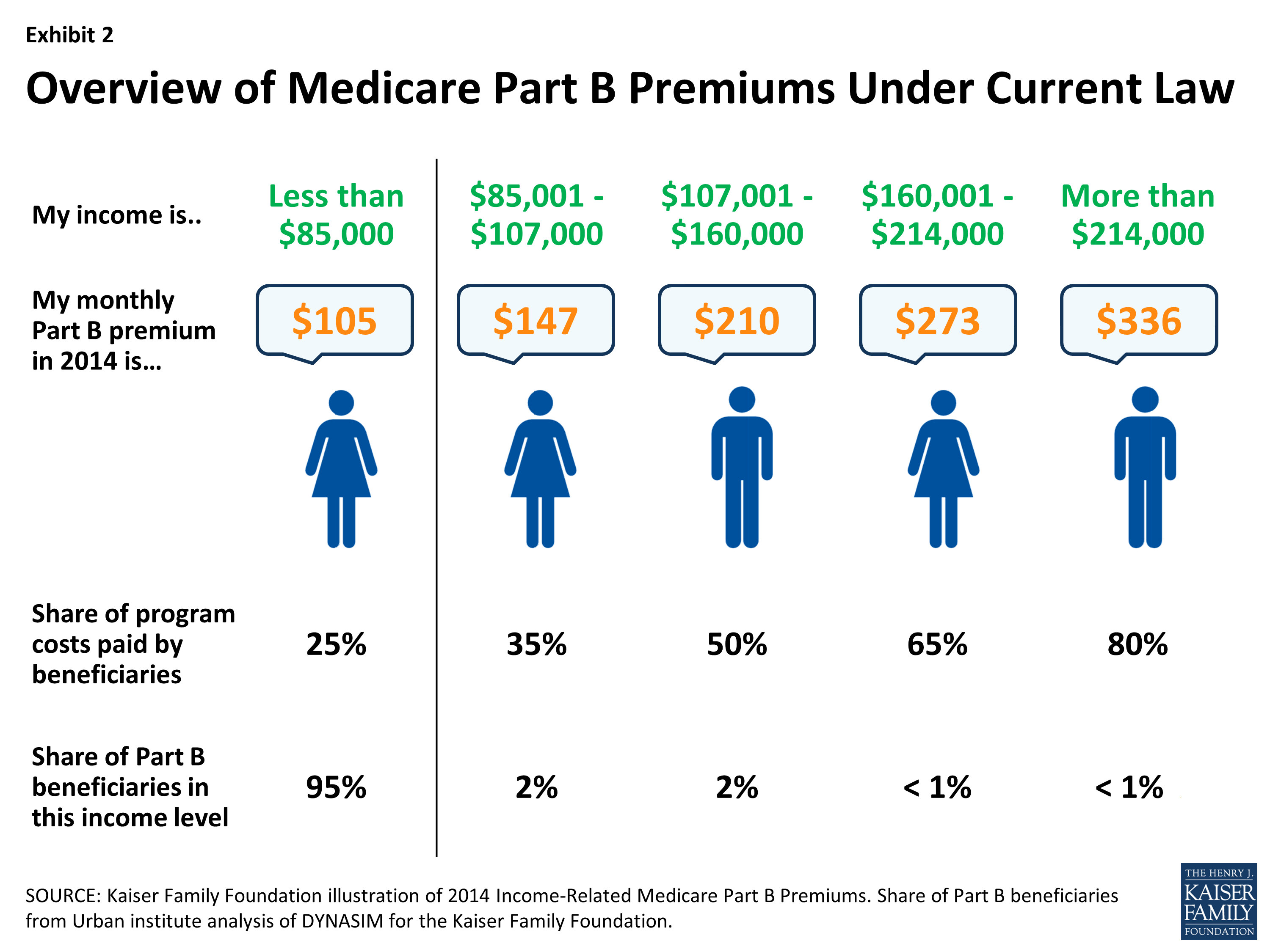
How much do you pay for Medicare Part B?
In most cases, you must complete a Part B reimbursement program application and include a copy of your Medicare card or Part B premium information. Medicare Savings Programs Finally, there are four Medicare Savings Programs for people who have limited income and resources but who earn too much to qualify for Medicaid. They are:
When can I add Part B to my Medicare?
Reimbursement checks are typically mailed out once a year. If you pay more than the standard Part B premium, you may be eligible for full reimbursement. Some pension plans may offer reimbursement only up to the standard premium amount. Reimbursement of Medicare Part B premiums isn’t available to most people, but it may be worth your while to ask your pension …
What is the maximum premium for Medicare Part B?
Jul 27, 2021 · How to Get Reimbursed From Medicare To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out. You can print it and fill it out by hand.
How do you enroll in Medicare Part B?
Jan 15, 2021 · If you are a new Medicare Part B enrollee in 2021, you will be reimbursed the standard monthly premium of $148.50 and do not need to provide additional documentation. If you received a Medicare Part B reimbursement of $144.60 on your pension check in 2020, you do not need to provide documentation and your Part B reimbursement will automatically increase …

What is Medicare Part B reimbursement?
One of the keys to understanding Medicare Part B reimbursement is “ assignment ,” which can be confusing for those not familiar with medical insurance terminology. Medicare’s definition of an assignment is “an agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for ...
How much is Medicare Part B deductible?
Medicare Part B has an annual deductible that is currently set at $198 per year. Medicare will not pay anything under Part B until that amount is paid by the patient.
How much does an assignment cost if a provider does not accept it?
A provider who does not accept assignment can bill you for the $25 difference between the professional fee and the approved amount, plus the $15 coinsurance for a total of $40. From a financial standpoint, it is obvious that it’s to your advantage to find providers and suppliers that accept assignment.
What is Medicare coinsurance?
Medicare coinsurance is your responsibility. Finding providers who accept assignment will save you money and the potential issues of filing your own claim. Medicare claims are processed by contracted insurance providers known as MACs. You have the right to appeal any decision by Medicare.
What is billed fee?
The billed amount, or professional fee, is simply the amount for a service or item that appears on a provider’s bill. If no insurance was involved, that is the amount a patient would be charged. The Medicare-approved amount is what Medicare would pay for any covered service or item.
What percentage of Medicare Part B is paid?
The approved amount is also sometimes referred to as the Medicare Fee Schedule. Medicare Part B pays 80 percent of its approved amount. The remaining 20 percent that can be billed to the patient is known as the Medicare coinsurance.
What is an appeal in Medicare?
An appeal is an action you can take if you disagree with the way your claim was processed. If you believe a service or item was denied in error, or you disagree with the amount of payment, you have the right to appeal. You may also appeal if Medicare stops paying for an item or service that you are currently receiving and believe you still need.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What to do if a pharmacist says a drug is not covered?
You may need to file a coverage determination request and seek reimbursement.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
How to contact Medicare Part B?
If you have additional questions about your Medicare Part B reimbursement, please contact the Medical and Dental Benefits Section at (213) 279-3115, toll free at (844) 88-LAFPP ext. 93115, or via email to [email protected].
How much is Medicare Part B in 2021?
If you are a new Medicare Part B enrollee in 2021, you will be reimbursed the standard monthly premium of $148.50 and do not need to provide additional documentation. If you received a Medicare Part B reimbursement of $144.60 on your pension check in 2020, you do not need to provide documentation and your Part B reimbursement will automatically ...
Does LAFPP reimburse IRMAA?
You may submit a copy of the first page of your IRMAA letter if it contains your name, address and 2021 monthly Medicare Part B premium deduction. LAFPP does not reimburse IRMAA fees, so your Part B reimbursement will not exceed the 2021 standard monthly premium of $148.50.
How Does Medicare Reimbursement Work?
If you are on Medicare, you usually don’t have to submit a claim when you receive medical services from a doctor, hospital or other health care provider so long as they are participating providers.
How to Get Reimbursed from Medicare
While most doctors simply bill Medicare directly, some other health care providers may require you to file for reimbursement from Medicare.
Reimbursement for Original Medicare
You won’t likely see a bill for services covered by Original Medicare. Participating providers will simply bill Medicare directly.
Medicare Advantage
You will never have to file a Medicare reimbursement claim if you have a Medicare Advantage plan. Medicare pays the private companies that manage Medicare Advantage plans to handle your claims for you.
Part D Prescription Drug Plan Reimbursement
Medicare Part D Prescription Drug plans are administered by private insurance companies. Generally, these companies handle any reimbursement process so you don’t have to worry about filing one.
When Can I Request a Medicare Refund?
Typically, beneficiaries won’t need to request refunds or reimbursements for Medicare Part A and Part B services because health care providers bill Medicare directly and will only bill patients for deductibles, copayments, coinsurance or for services or items that are not covered by Medicare.
What Is a Medicare Premium Refund?
There are certain cases in which Medicare may issue a refund on your monthly premium.
Who Qualifies for a Medicare Premium Refund?
Members of Medicare Advantage plans that offer Part B premium reimbursements can be eligible for a full or partial refund of their Medicare Part B premium. In addition, retirees of certain organizations such as a city fire department are sometimes eligible for subsidies that issue full or partial reimbursements of Medicare premiums.
How Do I Get My Money Back from Medicare?
To get a refund or reimbursement from Medicare, you will need to complete a claim form and mail it to Medicare along with an itemized bill for the care you received. Medicare’s claim form is available in English and in Spanish.
Important Terminology
Billed Amount vs. Approved Amount
Assignment
- One of the keys to understanding Medicare Part B reimbursement is “assignment,” which can be confusing for those not familiar with medical insurance terminology. Medicare’s definition of an assignment is “an agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any mor…
What If The Doctor Or Supplier Does Not Accept assignment?
- This does not mean you cannot seek treatment from them. It also doesn’t mean the service or item will be denied by Medicare. These are both common misconceptions. However, there are some distinct disadvantages to using non-participating providers: 1. You may have to pay the entire charge for the service or item at the time of service. 2. You will usually end up paying mor…
How Are Medicare Part B Claims paid?
- All Medicare Part B claims are processed by contracted insurance providers divided by region of the country. The current term for these providers is “Medicare administrative contractors” (MACS). Providers file your Part B claim to one of the MACS and it is from them that you will receive a notice of how the claim was processed. The statement you wi...
Medicare Supplemental Insurance
- While not strictly a part of Medicare, “Medigap” plans are worth a brief mention. They are sold by private insurers in every state, and their main function is to pick up the 20 percent Medicare coinsurance. More extensive information on them is available on the Medicare website at this tab.
Filing An Appeal
- An appeal is an action you can take if you disagree with the way your claim was processed. If you believe a service or item was denied in error, or you disagree with the amount of payment, you have the right to appeal. You may also appeal if Medicare stops paying for an item or service that you are currently receiving and believe you still need. If you decide toappeal Medicare’s decision…