Is CPT code 87086 covered by Medicare?
CMS (Medicare) has determined that Bacterial Culture, Urine (CPT Codes 87086, 87088) is only medically necessary and, therefore, reimbursable by Medicare when ordered for patients with any of the diagnostic conditions listed below in the “ICD-9-CM Codes Covered by Medicare Program.”
How to get reimbursement from Medicare?
How to Get Reimbursed From Medicare To get reimbursement, you must send in a completed claim form and an itemized bill that supports your claim. It includes detailed instructions for submitting your request. You can fill it out on your computer and print it out.
How do I Pay my Medicare premium Bill?
If you get a "Medicare Premium Bill" from Medicare, there are 4 ways to pay your premium, including 2 ways to pay online: Log into (or create) your secure Medicare account — Select “Pay my premium” to make a payment by credit card, debit, card, or from your checking or savings account.
How long does it take for Medicare to reimburse my medical bills?
It takes Medicare at least 60 days to process a reimbursement claim. If you haven’t yet paid your doctors, be sure to communicate with them to avoid bad marks on your credit.
Does CPT code 87086 need a modifier?
CPT Code For Urinalysis With Culture CPT 81001 and CPT 81002 will be reported when Urinalysis is done. If done with culture, then it would be separately reportable with CPT 87086 and CPT 87088 with culture. No modifier is required to bill these services in addition.
Does Medicare cover urine cultures?
Testing for asymptomatic bacteriuria as part of a prenatal evaluation may be medically appropriate but is considered screening and, therefore, not covered by Medicare.
What does CPT code 87086 mean?
87086, 87088. Urine Culture, Bacterial. Coverage Indications, Limitations, and/or Medical Necessity. A bacterial urine culture is a laboratory test service performed on a urine specimen to establish the probable etiology of a presumed. urinary tract infection.
What ICD 10 codes cover urine culture?
Unspecified abnormal findings in urinemicrobiological examination R82.79 (culture)positive culture R82.79.
Why does Medicare not pay for urinalysis?
Urine screenings for employment and other non-medical reasons would not be eligible for coverage under Medicare benefits. With Medicare Part B coverage, most medically necessary diagnostic tests do not require copays or coinsurances. Part A benefits cover diagnostic tests for inpatient hospital stays.
What diagnosis will cover a urinalysis?
Healthcare providers often use urinalysis to screen for or monitor certain common health conditions, such as liver disease, kidney disease and diabetes, and to diagnose urinary tract infections (UTIs).
Does Medicare pay for venipuncture?
Physician-Performed Venipuncture If a venipuncture performed in the office setting requires the skill of a physician for diagnostic or therapeutic purposes, the performing physician can bill Medicare both for the collection – using CPT code 36410 – and for the lab work performed in-office.
Can you bill for urine collection?
99000 is intended to be reported when the practice incurs costs to handle and/or transport a specimen to a lab. For example, if the practice employs a messenger service to transport a specimen, then you can bill 99000. If the lab picks up the specimen at no cost to the practice it is not appropriate to report 99000.
What is the difference between automated and non automated urinalysis?
Automated is when they send it in for resultsand non-automated is the dipstick.
Does Medicare cover urine tests?
Medicare also covers clinical laboratory services, including urine drug testing (UDT), under Part B. Physicians use UDT to detect the presence or absence of drugs or to identify specific drugs in urine samples.
What is the ICD-10 code for urinalysis?
ICD-10 code R82. 90 for Unspecified abnormal findings in urine is a medical classification as listed by WHO under the range - Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified .
Does Medicare pay for CPT 81002?
Medicare has not paid any of our 81002, 85610 services, they paid the E/M = 99214, 99213 or 99215's.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What to do if a pharmacist says a drug is not covered?
You may need to file a coverage determination request and seek reimbursement.
What happens if you see a doctor in your insurance network?
If you see a doctor in your plan’s network, your doctor will handle the claims process. Your doctor will only charge you for deductibles, copayments, or coinsurance. However, the situation is different if you see a doctor who is not in your plan’s network.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
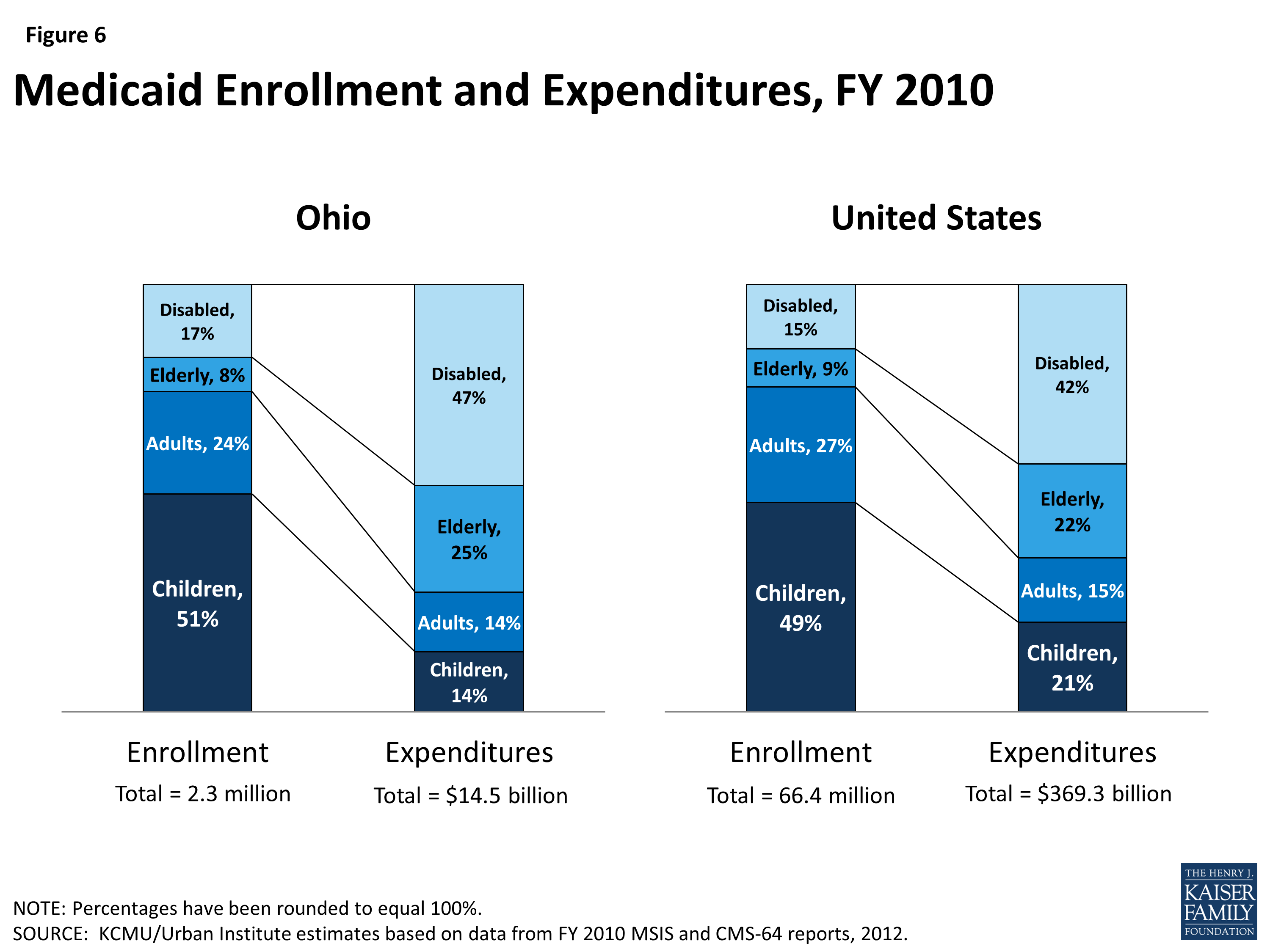
Medicaid
Medicaid is a joint federal/state program that helps with medical costs for some people with limited income and resources.
Medicare Savings Programs
State Medicare Savings Programs (MSP) programs help pay premiums, deductibles, coinsurance, copayments, prescription drug coverage costs.
PACE
PACE (Program of All-inclusive Care for the Elderly) is a Medicare/Medicaid program that helps people meet health care needs in the community.
Lower prescription costs
Qualify for extra help from Medicare to pay the costs of Medicare prescription drug coverage (Part D). You'll need to meet certain income and resource limits.
Programs for people in U.S. territories
Programs in Puerto Rico, U.S. Virgin Islands, Guam, Northern Mariana Islands, American Samoa, for people with limited income and resources.
Find your level of Extra Help (Part D)
Information for how to find your level of Extra Help for Medicare prescription drug coverage (Part D).
Insure Kids Now
The Children's Health Insurance Program (CHIP) provides free or low-cost health coverage for more than 7 million children up to age 19. CHIP covers U.S. citizens and eligible immigrants.
How much does Medicare pay for a doctor appointment?
Typically, you will pay 20 percent of the Medicare-approved amount, and Medicare will pay the remaining 80 percent .
What does it mean when a doctor accepts Medicare assignment?
If a doctor or supplier accepts Medicare assignment, this means that they agree to accept the Medicare-approved amount for a service or item as payment in full. The Medicare-approved amount could potentially be less than the actual amount a doctor or supplier charges, depending on whether or not they accept Medicare assignment.
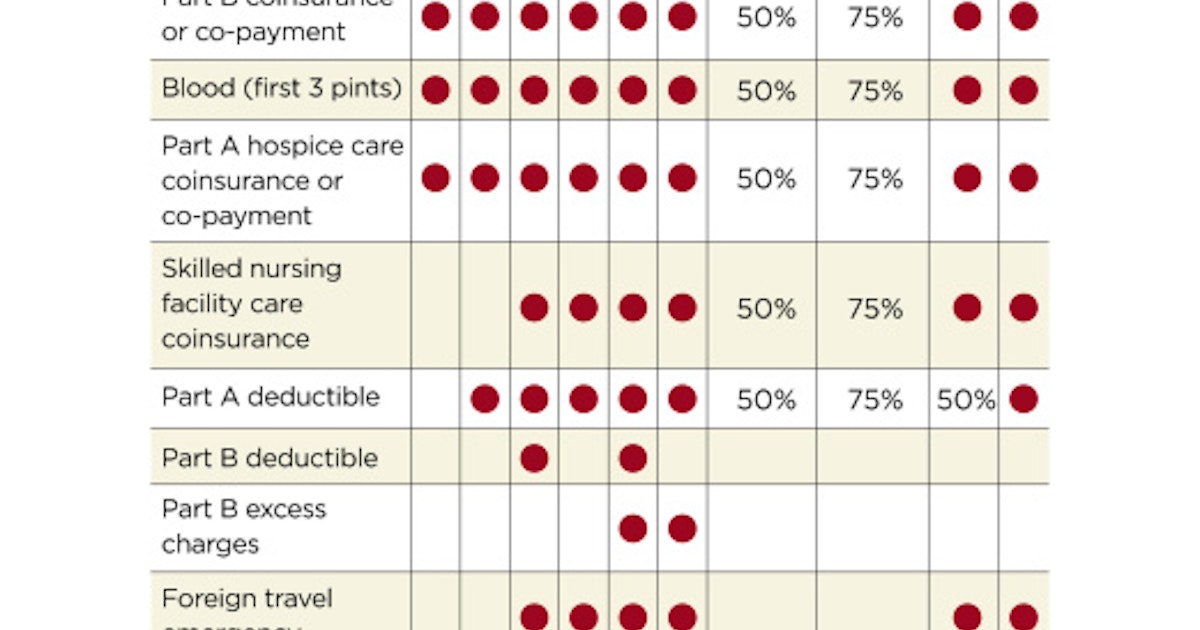
What is Medicare Supplement Insurance?
Some Medicare Supplement Insurance plans (also called Medigap) provide coverage for the Medicare Part B excess charges that may result when a health care provider does not accept Medicare assignment.
What is Medicare Part B excess charge?
What are Medicare Part B excess charges? You are responsible for paying any remaining difference between the Medicare-approved amount and the amount that your provider charges. This difference in cost is called a Medicare Part B excess charge. By law, a provider who does not accept Medicare assignment can only charge you up to 15 percent over ...
What is Medicare approved amount?
The Medicare-approved amount is the total payment that Medicare has agreed to pay a health care provider for a service or item. Learn more your potential Medicare costs. The Medicare-approved amount is the amount of money that Medicare will pay a health care provider for a medical service or item.
How much can a provider charge for not accepting Medicare?
By law, a provider who does not accept Medicare assignment can only charge you up to 15 percent over the Medicare-approved amount. Let’s consider an example: You’ve been feeling some pain in your shoulder, so you make an appointment with your primary care doctor.
Does Medicare cover a primary care appointment?
This appointment will be covered by Medicare Part B, and you have already satisfied your annual Part B deductible. Your primary care doctor accepts Medicare assignment, which means they have agreed to accept Medicare as full payment for their services. Because you have met your deductible for the year, you will split the Medicare-approved amount ...