Are diabetic shoes covered by Medicare?
· Medicare also requires: Verification of your need for therapeutic shoes and/or inserts from the doctor who treats your diabetes. Prescription for therapeutic shoes and/or inserts from a podiatrist or other qualified provider. Remember that even with Medicare, you may still pay a portion of the bill.
What are the Medicare requirements for diabetic shoes?
Medicare Part B (Medical Insurance) covers the furnishing and fitting of either of these each calendar year, if you have diabetes and severe diabetic foot disease: One pair of custom-molded shoes and inserts; One pair of extra-depth shoes; Medicare also covers: 2 additional pairs of inserts each calendar year for custom-molded shoes
How do I get diabetic shoes through Medicare?
The supplier of your prescription shoes must also be Medicare-approved in order for coverage rules to apply. Under Part B coverage and cost-sharing rules, you may be able to receive one pair of shoes each calendar year. If your shoes are custom-molded, Part B may also provide coverage for two more pairs of inserts.
What is the best Medicare-approved diabetic shoe brands?
· Medicare Part B covers diabetic shoes, inserts and in some cases molded shoes, if you qualify under the Medicare guidelines. Firstly, to qualify for shoes and inserts with Medicare Part B you have to have a diagnosis and certification from your physician that you have diabetes this has to be from the physician who is actually personally managing you systemic diabetes …

Does Medicare cover shoe inserts?
Medicare also covers: 2 additional pairs of inserts each calendar year for custom-molded shoes. 3 pairs of inserts each calendar year for extra-depth shoes. Medicare will cover shoe modifications instead of inserts.
Does Medicare cover therapeutic shoes?
Medicare will only cover your therapeutic shoes if your doctors and suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren't enrolled, Medicare won't pay the claims submitted by them. It's also important to ask your suppliers ...
What are therapeutic shoes?
Therapeutic shoes & inserts 1 One pair of custom-molded shoes and inserts 2 One pair of extra-depth shoes
What is original Medicare?
Your costs in Original Medicare. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. , you pay 20% of the. Medicare-Approved Amount.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference. , and the Part B.
How to find out how much a test is?
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like: 1 Other insurance you may have 2 How much your doctor charges 3 Whether your doctor accepts assignment 4 The type of facility 5 Where you get your test, item, or service
Does Medicare cover diabetic shoes?
Though these shoes require a prescription, they are considered durable medical equipment in most cases. This means they fall under Medicare Part B coverage and cost-sharing rules.
What is Medicare Part B?
Special shoes and inserts can help prevent these conditions, and Medicare Part B (Medical Insurance) coverage may provide patients with help covering the costs.
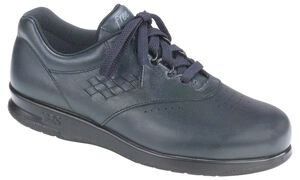
Why are toe boxes wider?
Interior stitching and seams are kept to a minimum, and the toe box is often higher and wider than a non-prescription shoe. This allows the foot to move within the shoe without excess rubbing between toes or around the heel and joints, which helps prevent sores and blisters from forming.
What is the exterior of a sock made of?
Their exterior is often made of a supple leather or soft fabric material with foam padding across the top of the foot and around the collar of the shoe.
Prevention of Diabetic Foot Injury and Infection
By following this list about foot care, you can decrease your chance of problems:
What are Diabetic Shoes?
All shoes are not created equal. To qualify as a diabetic shoe, certain standards must be met:
Will Medicare Pay for Diabetic Shoes?
Each calendar year, Medicare Part B (Medical Insurance) covers either:
Are You Ready for Great Foot Care?
Our site provides information about state-of-the-art foot care. You will find information about treatments, advanced technologies, and upcoming events. We also assist you in finding needed resources such as diabetic shoes.
How much does a diabetic shoe cost?
Diabetic shoes typically retail anywhere from $100-$160 for a good quality pair, however the prescribing physician will charge Medicare up to four times that amount with the bill coming out to upwards of $500.
How do I get diabetic shoes?
Where Do I Get My Diabetic Shoes 1 In order to receive diabetic shoes, the prescribed patient must be fitted for diabetic shoes by a podiatrist or any other qualified individual. 2 The certifying physician is not allowed to provide the patient with the footwear, unless they practice in a defined rural area or there is a shortage of health professionals 3 The prescribing physician may be the supplier.
Does Medicare pay 80% of what they approve?
Medicare DOES NOT pay 80% of what is billed by the doctor, Medicare pays 80% of what they approve, regardless of the amount billed. This statement in your ad is wrong and misleading and creates bad faith between a doctor and their patients. Get your facts straight and stop lying to the public.
What are the conditions that can cause amputation?
2) Patient has at least one of the following conditions: 1 Partial or complete foot amputation 2 Foot ulcers 3 Calluses on either foot which can lead to ulcers 4 Nerve damage in feet w/ signs of calluses on either foot 5 Foot deformities such as hammertoes or bunions 6 Poor circulation in the feet
Does Medicare Advantage cover diabetic shoes?
If you have the Medicare Advantage plan, that means that you have coverage due to a private Medicare-approved insurance company. These plans should cover all that Original Medicare covers with an exception for hospice care, which is what Medicare Part A covers. (Let’s hope you won’t need that for quite some time.) Thus, if you are enrolled in a Medicare Part C Advantage plan you must have coverage on diabetic shoes if all of the eligibility conditions are met.
Does Medicare cover therapeutic shoes?
Naturally, the Part B deductible will apply. Medicare will cover your therapeutic shoes only on the condition that your doctors and suppliers are also enrolled in Medicare.
When was the Therapeutic Shoe Bill passed?
Way back in May of 1993 (has it been that long?) Congress passed the Therapeutic Shoe Bill, known as TSB for short. The purpose of TSB is to provide reimbursement on therapeutic inserts, shoes and necessary modifications for beneficiaries who have diabetes and meet the very specific eligibility requirements.
Does Medicare cover custom molded shoes?
That’s great! Medicare Part B covers the furnishing and fitting of one (1) pair of custom-molded shoes and inserts and one (1) pair of extra-depth shoes per calendar year, provided you are diabetic and have a severe foot disease as a result of diabetes: Medicare will also cover two (2) extra pairs of inserts each calendar year for custom-molded shoes and three (3) pairs of inserts each calendar year for extra-depth shoes. They will also cover shoe modification in lieu of inserts.
Do you have to keep up with paperwork for diabetes?
Yep. But, don’t sweat it. Most of the paperwork will be your doctor’s responsibility. You just have to keep up with it! (A school folder is highly recommended to keep everything organized.) The doctor treating you for your diabetes must be able to certify that you do indeed have diabetes.
Why do diabetics rely on Medicare?
Because the American government is convinced that socialized medicine is the Devil many diabetic patients rely on Medicare and other insurance to defray the costs of supplies, medications, doctor visits and of course specialized footwear.
Can diabetics get neuropathy?
Many diabetics suffer from chronic diabetic neuropathy. This is nerve damage that can make your feet vulnerable to injuries in quite a number of various ways. Based on the findings of the Nation Institutes of Health:
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
What is coinsurance in insurance?
Coinsurance: An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
How often do you have to have your eyes checked for glaucoma?
Part B will pay for you to have your eyes checked for glaucoma once every 12 months if you’re at increased risk of glaucoma. You’re considered high risk for glaucoma if you have:
Does Medicare cover diabetic shoes?
Medicare, and most insurance plans, may cover the cost of one pair of diabetic shoes and three pairs of custom inserts per calendar year. Co-payments, deductibles and some restrictions apply. Check Eligibility.
What is a wrist brace?
A wrist brace is a garment that is worn around the wrist to protect it. No Cost Shoes was created by Quantum Medical Supply to educate clients and prospective shoe fitters about diabetic shoes and the coverage that Medicare provides.
Can you use electric seat assist on a sofa?
Electric-powered portable seat assist can be used on most armchairs or sofas. Providing 100% lift, users enjoy the freedom of effortlessly rising from their chair, at home or when visiting.
What is a tens unit?
A Transcutaneous Electrical Nerve Stimulator, or TENS Unit, is primarily used for managing chronic pain. It is a pocket size, portable, battery-operated device that sends electrical impulses to certain parts of the body to block pain signals.