- CMS-1500 Claim Form Instructions.
- CMS-1500 Claim Form Tutorial.
How do I get the Medicare form I Need?
Durable medical equipment (DME) coverage. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
How do I submit a patient request for medical payment form?
that you respond to the NSC as soon as possible. Failure to do so may delay your enrollment. ENROLLMENT PROCESS. The process for becoming a Medicare DMEPOS supplier is as follows: 1. The applicant completes and submits the the Medicare enrollment application (Form CMS-855S) and all supporting documentation to the NSC. 2.
What if I need DME and I’m in a Medicare Advantage plan?
To get the Medicare form you need, find the situation that applies to you. Get forms in alternate formats. I want to make sure Medicare can give my personal health information to someone other than me (Authorization to Disclose Personal Health Information form/CMS-10106). Fill out Authorization to Disclose Personal Health Information. This form is available both in English …
How do I apply for Medicare as a DMEPOS supplier?
Definitions of blue words are on pages 18–19. Note: The information in this booklet describes the Medicare Program at the time this booklet was printed. Changes may occur after printing. Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most
What is a Medicare CMN form?
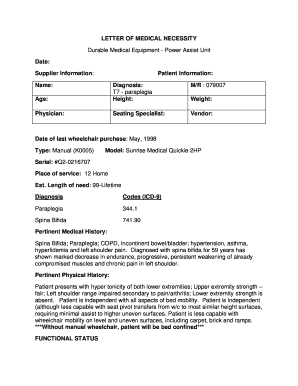
A certificate of medical necessity (CMN) is documentation from a doctor which Medicare requires before it will cover certain durable medical equipment (DME). The CMN states the patient's diagnosis, prognosis, reason for the equipment, and estimated duration of need.
How do I submit a DME claim to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Which is the claim form used for billing DME?
CMS-1500 formThe CMS-1500 form is the standard claim form used by a non-institutional provider or supplier to bill Medicare carriers and durable medical equipment regional carriers (DMERCs) when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of ...Dec 1, 2021
What is DME assessment?
Face-to-face encounter is a popular term for the assessment completed by practitioners during a patient visit for durable medical equipment, such as power mobility, oxygen and CPAP therapy. This generates associated paperwork that is often referred to as face-to-face documentation.
How do I claim Medicare receipts?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov pin. On your homepage, select Make a claim. Make sure you have details of the service, cost and amount paid to continue your claim.Dec 10, 2021
Can I make a Medicare claim online?
Claim Medicare benefits online If you can't claim at the doctor's office, you can submit a Medicare claim online using either: your Medicare online account through myGov.Dec 10, 2021
What are DME claims?
TRICARE covers Durable Medical Equipment (DME) when prescribed by a physician and includes, but is not limited to, items such as wheelchairs, CPAP machines, crutches, etc.
Does DME need a modifier?
In addition to an appropriate HCPCS code for the DME item, many HCPCS codes require a modifier. The modifiers are used to provide more information about the item. For example, the modifier may tell HMSA that an item is new, used, or rented on a capped basis.
What is the difference between the CMS-1500 form and UB 04 form?
When a physician has a private practice but performs services at an institutional facility such as a hospital or outpatient facility, the CMS-1500 form would be used to bill for their services. The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities.
How do I write a DME order?
Standardized DMEPOS Written Order/PrescriptionBeneficiary name or Medicare Beneficiary Identifier (MBI) Number.Description of the item.Quantity, if applicable.Treating practitioner name or National Provider Identifier (NPI)Date of the order.Treating practitioner signature.Jan 12, 2022
What is a 5 element order?
The 6407- required order is referred to as a five-element order (5EO). The 5EO must meet all of the requirements below: The 5EO must include all of the following elements: Beneficiary's name. Item of DME ordered - this may be general – e.g., "hospital bed"– or may be more specific.
What DME means?
Durable Medical EquipmentEquipment and supplies ordered by a health care provider for everyday or extended use. Coverage for DME may include: oxygen equipment, wheelchairs, crutches or blood testing strips for diabetics.
What is the Medicare enrollment form for DMEPOS?
DMEPOS suppliers must enroll in the Medicare program using the Medicare enrollment application (Form CMS-855S) in order to be eligible to receive Medicare payment for covered services provided to Medicarebeneficiaries.
What is NPI in DMEPOS?
The National Provider Identifier (NPI) will replace health care provider identifiers in use today in standard health care transactions. DMEPOS suppliers must obtain their NPI prior to enrolling in the Medicare program. Enrolling in Medicare authorizes you to bill and be paid for services furnished to Medicare beneficiaries.
Enrollment forms
I have Part A and want to apply for Part B (Application for Enrollment in Part B/CMS-40B).
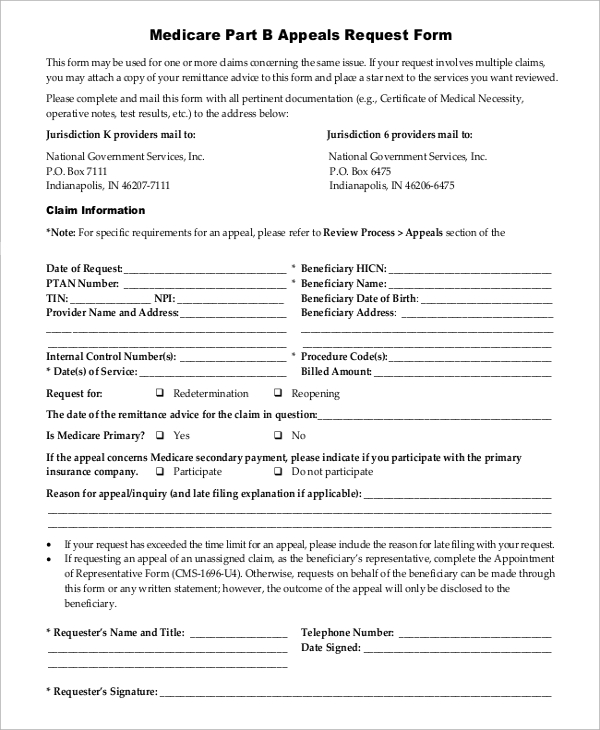
Appeals forms
I want to appoint a representative to help me file an appeal (Appointment of Representative form/CMS-1696).
What is assignment in Medicare?
Assignment —An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance.
Does Medicare pay for DME repairs?
Medicare will pay 80% of the Medicare-approved amount (up to the cost of replacing the item) for repairs. You pay the other 20%. Your costs may be higher if the supplier doesn’t accept assignment.
How long does it take to change your Medicare billing information?
It’s important to keep your enrollment information up to date. To avoid having your Medicare billing privileges revoked, be sure to report any change within 30 days. Changes include, but are not limited to: a change in ownership. an adverse legal action. a change in practice location.
What is DMEPOS in Medicare?
Suppliers who receive Medicare reimbursement for durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS) are required to: If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers.
What to do if your business doesn't dispense DMEPOS?
If your business doesn’t dispense or furnish DMEPOS, you should use the Medicare Enrollment Guide for Providers & Suppliers. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should refer to the Medicare Enrollment Guide for Institutional Providers.
When will CMS reprocess claims?
Claims for these accessories submitted prior to July 1, 2020, with dates of service from January 1, 2020 through June 30, 2020, will need to be reprocessed to ensure that CMS pays the unadjusted fee schedule amounts, as required by section 106 of the Further Consolidated Appropriations Act, 2020.
What is gap filling in Medicare?
For newly covered items of DMEPOS paid on a fee schedule basis where a Medicare fee does not exist , the Centers for Medicare & Medicaid Services (CMS) uses a process to establish fees called gap-filling. This allows Medicare to establish a price that aligns with the statutory requirements for the DMEPOS fee schedule.
What is Medicare Accessibility Act?
CMS is implementing the Patient Access and Medicare Protection Act to ensure that beneficiaries have access to wheelchair accessories and seat and back cushions when furnished with Group 3 complex rehabilitative power wheelchairs. To ensure beneficiary access to these accessories particularly for these vulnerable populations, advance payment may be available for suppliers. Prior to July 1, suppliers will be paid the adjusted fee schedule rates. The average reduction during this period for these items is approximately 10%. During this time, CMS has announced that suppliers are able to submit a single advance payment request for multiple claims if the conditions described in CMS regulations at 42 CFR Section 421.214 are met. Additional information is below.
What is a DMEPOS file?
The DMEPOS public use file contains fee schedules for certain items that were adjusted based on information from the DMEPOS Competitive Bidding Program in accordance with Section 1834 (a) (1) (F) of the Act.
What is TTFT in Medicare?
TTFT is a system consisting of an electromagnetic field generator and transducer arrays and will be covered under the Medicare Part B benefit for durable medical equipment (DME) for items and services furnished on or after September 1, 2019.
When will Medicare change the KU modifier?
As aforementioned, these system changes will be implemented on July 1, 2020.
Does Medicare cover CGMs?
Based on input from patients and other stakeholders, The Centers for Medicare & Medicaid Services (CMS) is announcing important changes in its written policies regarding how Medicare covers continuous glucose monitors (CGMs). These changes are consistent with the Agency’s approach of putting patients first and incentivizing innovation and use of e-technology.
When will phase 2 of DME start?
Phase II will begin October 21, 2019 and expands prior authorization of these codes to the remaining states and territories.
When will the DMEPOS process end?
Given the importance of medical review activities to CMS’ program integrity efforts, CMS will discontinue exercising enforcement discretion for the Prior Authorization Process for Certain Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) items beginning on August 3, 2020, regardless of the status of the public health emergency. For Power Mobility Devices and Pressure Reducing Support Surfaces that require prior authorization as a condition of payment, claims with an initial date of service on or after August 3, 2020 must be associated with an affirmative prior authorization decision to be eligible for payment.
How long does it take to get a prior authorization?
Please note that all initial prior authorization decisions should be made in no more than 10 days. In cases where that timeframe could seriously jeopardize the life or health of the beneficiary, you may request an expedited review. Decisions for substantiated expedited reviews should be made within 2 business days.
When is the CMS call for pressure reducing support surfaces?
CMS will host a call to discuss the addition of pressure reducing support surfaces to the Required Prior Authorization List on Tuesday, June 4, 2019 from 2:00 p.m. to 3:30 p.m. Eastern Time (ET). For more information, please visit the Special Open Door Forums webpage.
Where can I download Medicare reimbursement form?
You can download the reimbursement form at Medicare’s website or at the link below. The form is called the Patient Request for Medical Payment form. You must carefully read and fill out each part of the form or else Medicare will send it back to you for you to complete and re-submit.
What is a DME in Medicare?
Medicare Reimbursement for Durable Medical Equipment. Wheelchairs, walkers, hospital beds, and oxygen pumps are all examples of durable medical equipment (DME). For a piece of medical equipment to be considered durable, it must be able to withstand extended use.
How much does Medicare pay for Part B?
Medicare Part B will pay 80% of the cost, while you pay the other 20%. This is known as your Part B coinsurance. Medicare has a pre-approved price for each type of durable medical equipment though, and these rates are heavily discounted from the retail price.
How long do you have to file a DME claim?
For Medicare to even consider your reimbursement claim, you must file it no later than 12 months after the date of service – or in this case date of which you purchased the equipment.
Is DME part of Medicare?
It’s important to use a DME provider that is either part of Medicare’s competitive bidding program or accepts Medicare assignment rates. Otherwise, you could end up having to pay excess charges up to an additional 15% of the approved price.
Does Medicare cover DME?
Medicare has fairly strict guidelines for covering DME. For instance, Medicare will not cover a power wheelchair if the only reason you need it is for getting around outside of your home. You must need the equipment to safely get around inside your home in order for Medicare to cover it at all.
How to become a Medicare provider?
Become a Medicare Provider or Supplier 1 You’re a DMEPOS supplier. DMEPOS suppliers should follow the instructions on the Enroll as a DMEPOS Supplier page. 2 You’re an institutional provider. If you’re enrolling a hospital, critical care facility, skilled nursing facility, home health agency, hospice, or other similar institution, you should use the Medicare Enrollment Guide for Institutional Providers.
How long does it take to change your Medicare billing?
To avoid having your Medicare billing privileges revoked, be sure to report the following changes within 30 days: a change in ownership. an adverse legal action. a change in practice location. You must report all other changes within 90 days. If you applied online, you can keep your information up to date in PECOS.
How to get an NPI?
If you already have an NPI, skip this step and proceed to Step 2. NPIs are issued through the National Plan & Provider Enumeration System (NPPES). You can apply for an NPI on the NPPES website.
Do you need to be accredited to participate in CMS surveys?
ii If your institution has obtained accreditation from a CMS-approved accreditation organization, you will not need to participate in State Survey Agency surveys. You must inform the State Survey Agency that your institution is accredited. Accreditation is voluntary; CMS doesn’t require it for Medicare enrollment.
Can you bill Medicare for your services?
You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify. You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.
How long does it take to get a recertification for home oxygen therapy?
The recertification at three months must reflect the results of an arterial blood gas or oxygen saturation test conducted between the 61st and 90th day of home oxygen therapy. If the beneficiary no longer requires home oxygen therapy after three months, retesting is not necessary.
What is a DIF in medical billing?
A DIF is completed and signed by the supplier. It does not require the cost, a narrative description of equipment or a physician's signature. For certain items or services billed to a DME MAC, the supplier must receive a signed CMN from the treating physician or a signed DIF from the supplier.
Do you have to maintain a copy of a faxed CMN?
It is in the supplier's interest to maintain a copy of what they faxed to the physician. Suppliers must maintain a copy of the completed CMN or DIF in their records. However, if the physician only faxes the front of the completed CMN then the supplier is only required to maintain the front portion of the CMN.
Do you have to send a CMN to a physician?
The CMN sent to the physician must be two-sided with instructions on the back. If the CMN is mailed to the physician, the supplier must send the two-sided form. If the CMN is faxed, the supplier must fax both the front and back of the form.