
For individuals, the easiest way to find your Medicare provider identification number is to look on your Medicare card. The Medicare number format typically consists of your Social Security number followed by a special identifying code. It's also helpful to know what the "A" and "B" on your Medicare benefits signify.
Full Answer
How do I get a Medicare Provider Identifier?
A Medicare provider becomes certified once they’ve passed inspection by a state government agency. Medicare provider certification involves a lengthy application form. Once the Medicare provider is approved, they receive a National Provider Identifier (NPI) and Medicare billing number. What if my provider is not approved? Medicare only covers care from certified …
How do I find Medicare providers who have opted out?
To participate as a Medicare Program provider or supplier, submit the Medicare Participating Physician or Supplier Agreement (Form CMS-460) upon initial enrollment. You’ve 90 days after your initial enrollment approval letter is sent to decide if …
How do I know if my Medicare enrollment has been updated?
Apply online to obtain a National Provider Identifier (NPI) using the National Plan & Provider Enumeration System (NPPES). You may also update your information on file by accessing the system. Access the NPI enumeration system (NPPES) Search for provider NPI information using the NPI Registry Medicare Provider Enrollment (PECOS) Access
How do I find out what Medicare coverage I have?
The letter will explain that Medicare records indicate you do not have an enrollment record in PECOS because you enrolled in Medicare prior to implementation of PECOS and you have not submitted any updates or changes to your Medicare enrollment information in …
What is a Medicare provider?
A Medicare provider is a physician, health care facility or agency that accepts Medicare insurance. Providers earn certification after passing inspection by a state government agency. Make sure your doctor or health care provider is approved by Medicare before accepting services.
What is the difference between a Medicare provider and supplier?
Supplier means a physician or other practitioner, or an entity other than a provider, that furnishes health care services under Medicare.
Is the Medicare provider number the same as NPI?
The NPI is the National Provider Identifier, and is a unique identification number provided to facilities and other medical entities. The Medicare Provider Number is also known as the CCN (CMS Certification Number). This is the six-digit Medicare certification number for a facility.
Is Pecos ID same as Medicare number?
The following walk-thru explains how a user can find their Medicare ID number in PECOS. Medicare numbers are also known as the CCN, P-Tan, Oscar, Provider number, or Medicare ID.
What is a Medicare Part B provider?
Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers. medically necessary.
What is an authorized official?
An authorized official means an appointed official (i.e. chief executive officer, chief financial officer, general partner, chairman of the board, or 5 percent or greater direct owner) to whom the organization has granted the legal authority to enroll it in the Medicare program, to make changes or updates to the ...Mar 3, 2022
How do I get my Medicare number?
Sign in to myGov and select Medicare. If you're using the app, open it and enter your myGov PIN. On your homepage, select My card. You'll see your current Medicare card.Mar 15, 2022
How many digits is a Medicare ID number?
11 charactersThe MBI has 11 characters, like the Health Insurance Claim Number (HICN), which can have up to 11.
Is the organization a subpart?
A subpart is a component of an organization health care provider that furnishes health care and is not itself a separate legal entity. If you are an individual who is a health care provider and who is incorporated, you may need to obtain an NPI for yourself (Type 1) and an NPI for your corporation or LLC (Type 2).
What does a Medicare ID number look like?
On a Medicare card, an MBI will appear similar to this: 1EG4-TE5-MK73. The second, fifth, eighth, and ninth characters are always letters while the first, fourth, seventh, tenth, and eleventh characters are always numbers. You can visit cms.gov for more information on the format of an MBI.
How do I know if a provider is enrolled in Pecos?
To determine if you have a current enrollment record in the PECOS, you can do the following:Utilize the national file of Medicare physicians and non-physician practitioners who are eligible to order / refer and have current enrollment records in the PECOS. ... Utilize Internet-based PECOS.More items...•Nov 17, 2017
What is a Pecos provider?
PECOS stands for Provider, Enrollment, Chain, and Ownership System. It is the online Medicare enrollment management system that allows individuals and entities to enroll as Medicare providers or suppliers.Dec 11, 2020
What is Medicare provider certification?
Medicare provider certification involves a lengthy application form. Once the Medicare provider is approved, they receive a National Provider Identifier (NPI) and Medicare billing number.
What does it mean to be certified by Medicare?
To be approved or certified by Medicare means that the provider has met the requirements to receive Medicare payments.
What is Medicare provider?
A Medicare provider is a person, facility, or agency that Medicare will pay to provide care to Medicare beneficiaries. For example, a Medicare provider could be: The same Medicare provider may be covered by Original Medicare (Part A and Part B), Medicare Advantage, and Medicare Supplement.
Does Medicare cover non-certified providers?
Medicare only covers care from certified Medicare providers. If you receive a typically covered service from a non-certified provider, your care may not be covered. If you wish to continue using that provider, you may have to pay all costs out of pocket.
How to change Medicare enrollment after getting an NPI?
Before applying, be sure you have the necessary enrollment information. Complete the actions using PECOS or the paper enrollment form.
How to get an NPI for Medicare?
Step 1: Get a National Provider Identifier (NPI) You must get an NPI before enrolling in the Medicare Program. Apply for an NPI in 1 of 3 ways: Online Application: Get an I&A System user account. Then apply in the National Plan and Provider Enumeration System (NPPES) for an NPI.
How to request hardship exception for Medicare?
You may request a hardship exception when submitting your Medicare enrollment application via either PECOS or CMS paper form. You must submit a written request with supporting documentation with your enrollment that describes the hardship and justifies an exception instead of paying the application fee.
What are the two types of NPIs?
There are 2 types of NPIs: Type 1 (individual) and Type 2 (organizational). Medicare allows only Type 1 NPIs for solely ordering items or certifying services. Apply for an NPI in 1 of 3 ways:
How long does it take to become a Medicare provider?
You’ve 90 days after your initial enrollment approval letter is sent to decide if you want to be a participating provider or supplier.
What is Medicare Part B?
Medicare Part B claims use the term “ordering/certifying provider” (previously “ordering/referring provider”) to identify the professional who orders or certifies an item or service reported in a claim. The following are technically correct terms:
What is Medicare revocation?
A Medicare-imposed revocation of Medicare billing privileges. A suspension, termination, or revocation of a license to provide health care by a state licensing authority or the Medicaid Program. A conviction of a federal or state felony within the 10 years preceding enrollment, revalidation, or re-enrollment.
Do you need an enrollment record for PECOS?
You need an approved enrollment record in PECOS to continue to refer or order items or services for your Medicare patients. If you do not have a current and active Medicare enrollment record, it is imperative that you take the necessary action to establish your enrollment record as soon as possible.
Can you get Medicare for electronic health records?
It is possible that you may not be able to receive incentive payments from Medicare for meaningful use of certified electronic health records. These incentive payments are authorized by the American Recovery and Reinvestment Act of 2009. More information on this initiative, also known as HITECH, is available at ...
What does it mean when a provider opts out of Medicare?
What it means when a provider opts out of Medicare. Certain doctors and other health care providers who don't want to work with the Medicare program may "opt out" of Medicare. Medicare doesn't pay for any covered items or services you get from an opt out doctor or other provider, except in the case of an emergency or urgent need.
How long does a doctor have to opt out?
A doctor or other provider who chooses to opt out must do so for 2 years, which automatically renews every 2 years unless the provider requests not to renew their opt out status.
Do you have to pay for Medicare Supplement?
If you have a Medicare Supplement Insurance (Medigap) policy, it won't pay anything for the services you get.
Can you pay out of pocket for Medicare?
Instead, the provider bills you directly and you pay the provider out-of-pocket. The provider isn't required to accept only Medicare's fee-for -service charges. You can still get care from these providers, but they must enter into a private contract with you (unless you're in need of emergency or urgently needed care).
Do you have to sign a private contract with Medicare?
Rules for private contracts. You don't have to sign a private contract. You can always go to another provider who gives services through Medicare. If you sign a private contract with your doctor or other provider, these rules apply: You'll have to pay the full amount of whatever this provider charges you for the services you get.
Does Medicare cover health care?
You're always free to get services Medicare doesn't cover if you choose to pay for a service yourself. You may want to contact your State Health Insurance Assistance Program (SHIP) to get help before signing a private contract with any doctor or other health care provider.
What is an annual review of Medicare?
An annual review of your Medicare coverage can help you determine if your plan combination is right for your needs. For example, if you’re spending a considerable amount of money on prescription drugs, a Medicare Part D plan or a Medicare Advantage plan with prescription drug coverage may be something to consider.
What are the benefits of Medicare Advantage?
Most Medicare Advantage plans offer additional benefits not covered by Original Medicare, such as dental, vision and prescription drug coverage. Medicare Part D provides coverage for prescription medications, which is something not typically covered by Original Medicare.
How long does Medicare AEP last?
The Medicare AEP lasts from October 15 to December 7 every year. During this time, Medicare beneficiaries may do any of the following: Change from Original Medicare to a Medicare Advantage plan. Change from Medicare Advantage back to Original Medicare. Switch from one Medicare Advantage plan to another.
What is Medicare Part B?
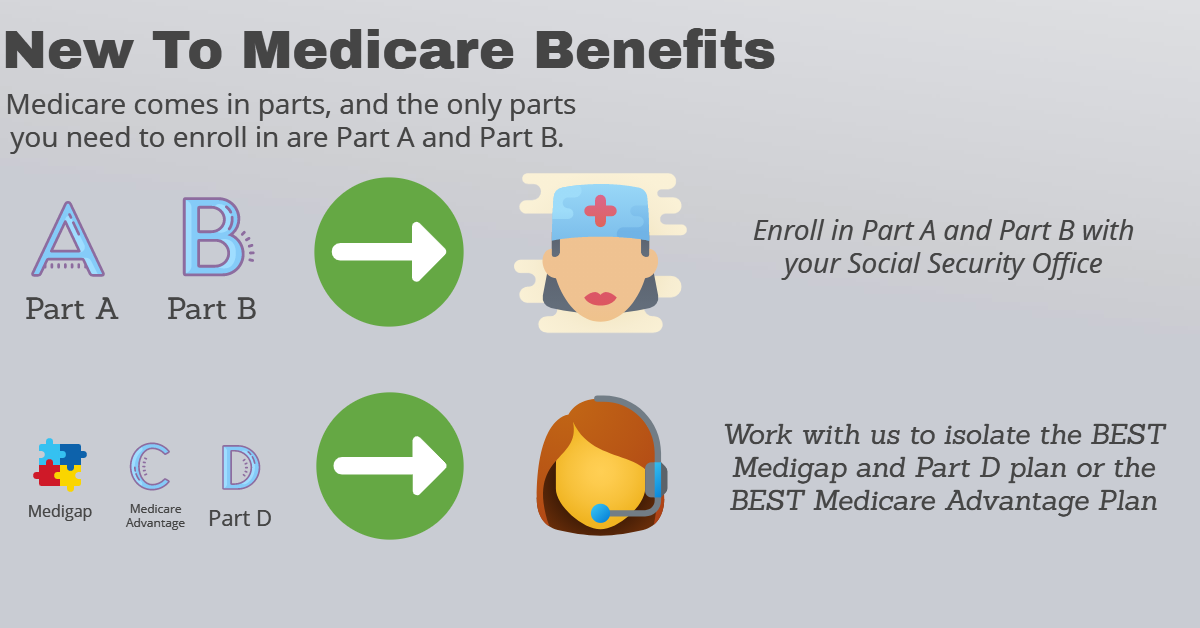
Medicare Part B is medical insurance and provides coverage for outpatient appointments and durable medical equipment. Part B is optional, but is required for anyone wanting to enroll in Medicare Part C, Part D or Medicare Supplement Insurance. Part A and Part B are known together as “Original ...
Is Medicare Part A and Part B the same?
Part A and Part B are known together as “Original Medicare.”. Medicare Part C, also known as Medicare Advantage, provides all the same benefits as Medicare Part A and Part B combined into a single plan sold by a private insurance company.
What is CR 6417?
Remember: Part B claims (CR 6417) that are the result of an order or a referral, must contain the National Provider Identifier (NPI) and the legal name of the ordering / referring provider and the ordering/referring provider must be in the PECOS. DMEPOS claims (CR 6421) that are the result of an order or a referral must contain the NPI and ...
What is the purpose of the PECOS article?
The purpose of this article is to provide guidance to assist physicians and non-physician practitioners in determining whether or not they have a current enrollment record in the PECOS, and if not, the necessary follow-up steps to take. Remember:
Who is eligible to order or refer items or services for Medicare beneficiaries?
For more information: Only physicians and certain types of non-physician practitioners are eligible to order or refer items or services for Medicare beneficiaries. They are as follows: Clinical social worker. To determine if you have a current enrollment record in the PECOS, you can do the following: 1.
Who can order Medicare services?
Only physicians and certain types of non-physician practitioners are eligible to order or refer items or services for Medicare beneficiaries. They are as follows: Doctor of medicine or osteopathy; Doctor of dental medicine; Doctor of dental surgery; Doctor of podiatric medicine; Doctor of optometry;
What is the maximum amount of Medicare Physician Fee Schedule?
If you are a Non-Participating provider, providing covered services and collecting payment from beneficiaries at the time of service, the maximum amount you may charge is 115% of the approved fee schedule amount for Non-Participating providers; which is 95% of the normal Medicare Physician Fee Schedule (MPFS).
How much can a non-participating provider bill Medicare?
Medicare will then send any reimbursement directly to the patient. As a Non-Participating Medicare Provider, you can bill the patient up to 115% of the Medicare Fee Schedule.
What is the most common Medicare Advantage plan?
There are coordinated care options such as HMOs or PPOs, private fee-for-service (PFFS) plans, and medical savings account (MSA) plans. The most common form of Medicare Advantage plan is the HMO. Apparently, there are a number of Medicare Advantage plans in which coverage is limited to only in-network providers.
What is the relationship status of a physical therapist with Medicare?
There are three possibilities for a Physical Therapist’s relationship-status with Medicare: 1) No relationship at all (notthe same as a “Non-Participating Provider” and also notthe same as “opting out”) 2) Participating Provider. 3) Non-Participating Provider.
Can you be a non-par provider for Medicare?
If you feel that you need to be able to treat Medicare beneficiaries, either financially or personally, but don’t want to wait for Medicare reimbursement (or denials), then being a Non-Par Provider might be a an option to consider regardless of the extra 15% you can bill.
Can a Medicare beneficiary see you out of network?
If a beneficiary with a Medicare Advantage plan wants to see you on a cash-pay basis, and you are out-of-network with that plan , you need to call the plan and ask them if it is okay for you to provide them with covered services and that the beneficiary pay you directly out-of-pocket.
Can non-par providers take payment in full?
This is hugely important for some practices in certain areas with certain demographics. Non-Par Providers can also take payment in full at the time of service directly from the beneficiary, so they are not waiting for a 3rd Party Payor to reimburse them.
