The best way to know which one you have is to call the number on the back of your insurance card. In some cases, it’s possible for someone to have both Medicare AND Medicaid. In order to enroll in both programs, the individual must meet the eligibility requirements for both programs.
How to confirm Medicaid benefits?
Mar 30, 2022 · Knowing which kind of Medicaid you have can be tricky. Every state has its own Medicaid program, which means coverage, requirements, and Medicaid cards will vary. The best way to know which one you have is to call the number on the back of your insurance card. Having Both Medicare and Medicaid
How do you get approved for Medicaid?
Aug 27, 2017 · Medicare is a program that is connected with Social Security. Medicare is available to any US citizen or permanent legal resident who has been in the US for at least 5 years and is at least 65 years old. In certain situations, it also may cover people with disabilities. For those who are younger than 65 to be eligible for Medicare you must:
How can I Check my Medicaid status online?
Each state has different rules about eligibility and applying for Medicaid. Call your State Medical Assistance (Medicaid) office for more information and to see if you qualify. You can also call 1-800-MEDICARE (1-800-633-4227) to get the phone number for your state's Medicaid office. TTY users can call 1-877-486-2048. Medicaid spenddown
How can you look up your Medicaid number?
The best way to find out if one has Medicare is to apply. The main websites for Medicare and Social Security have short and simple online application pages. One can apply and get an official answer very quickly. The sites state the qualifications needed, and they process moves quickly for most applicants. The Medicare system requires choices.

Who is eligible for medicaid?
Medicaid eligibility is available to low-income families, pregnant women, children, the elderly, people with disabilities, and those who receive Supplemental Security Income (SSI). Because this program has firm income eligibility requirements, laws for eligibility vary depending upon the state in which you live. Typically, eligibility follows the following criteria:
What are the requirements for Medicaid?
Medicaid eligibility is available to low-income families, pregnant women, children, the elderly, people with disabilities, and those who receive Supplemental Security Income (SSI). Because this program has firm income eligibility requirements, laws for eligibility vary depending upon the state in which you live. Typically, eligibility follows the following criteria: 1 Applicants must meet federal and state requirements including residency, immigration status, and proof of citizenship 2 Applicants must meet financial need requirements on both federal and state levels
What is the purpose of poverty level?
This measurement helps determine who is eligible for certain programs and benefits. The federal poverty level plays a role in eligibility and Medicaid services.
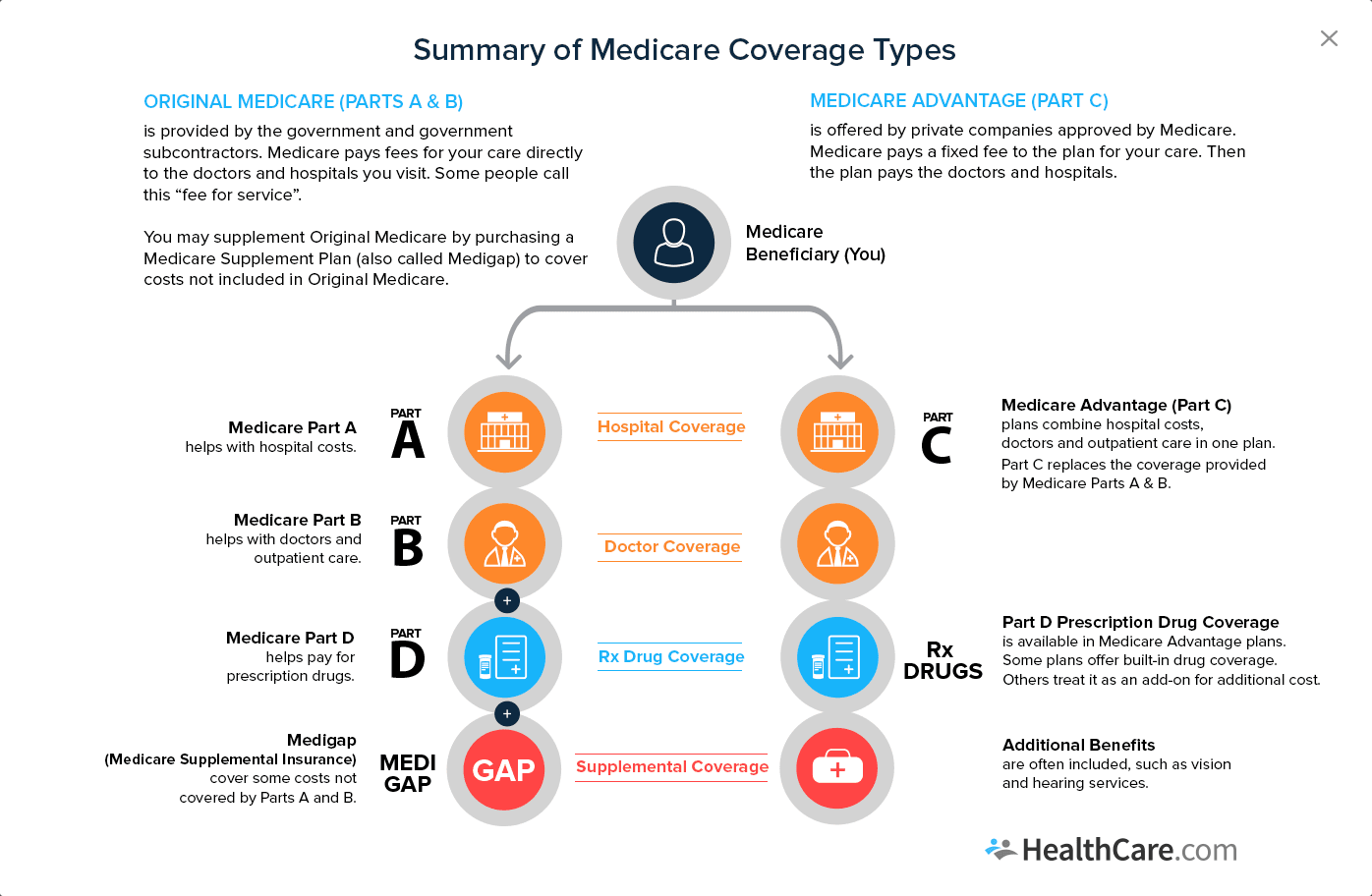
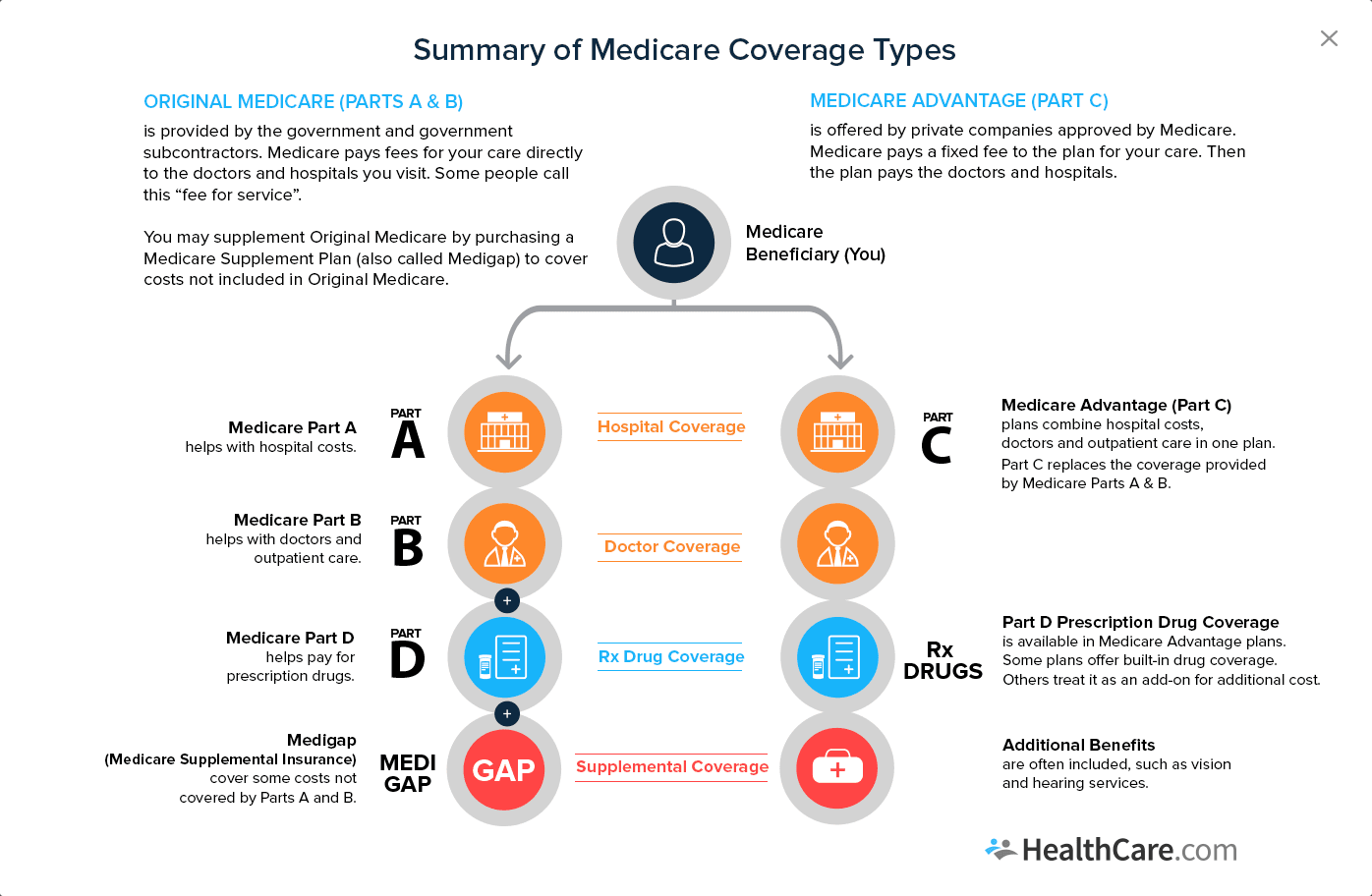
What is original Medicare?
Original Medicare is the standard Medicare program that the federal government offers. The government will directly pay for any health care services you receive. You can see any doctor or hospital that accepts Medicare. Here's how it works:
When does Medicare open?
Enrollment for Medicare is only open during certain times. In some cases, folks automatically enroll in Medicare when they turn 65. Some people are even automatically enrolled in Medicare when they turn 65. The 7 Month Initial Enrollment Period starts 3 months before turning 65, includes your birthday month, and ends 3 months after turning 65. It is important to know about all of your options so that when the time comes you know just what you want before applying for Medicare through Social Security.
What is the role of the primary payer in medical insurance?
The primary payer pays for your medical bills and then sends the remaining amount to the second payer.
How old do you have to be to get medicare?
Medicare is available to any US citizen or permanent legal resident who has been in the US for at least 5 years and is at least 65 years old. In certain situations, it also may cover people with disabilities. For those who are younger than 65 to be eligible for Medicare you must:
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is extra help?
And, you'll automatically qualify for. Extra Help. A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. paying for your.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
What is Medicare.gov?
Medicare is the agency that runs Medicare. It has many regional contractors that support the systems for payments, processing claims, and durable medical equipment. It oversees the performance of private insurance providers that sell Medicare Advantage, Medigap, and Prescription Drug plans. Medicare.gov is the ideal place to find ...
How old do you have to be to get Medicare?
Medicare has four parts that cover hospital insurance, medical insurance, private all-in-one plans, and prescription drug benefits. Everyone age 65 or older can get Medicare. Disabled persons can get it while under age 65. Those who paid FICA taxes for ten years can get premium-free Medicare.
What is comparison shopping in Medicare?
Comparison shopping is the ideal tool for making selections of private health, prescription drug, and gap insurance plans.
What is Medicare and Social Security?
Medicare and Social Security provide tools for determining eligibility and benefits. Medicare is the national health care program for older Americans. The start date for Medicare coverage is important; many other features depend on the date of enrollment. Medicare has four parts that cover hospital insurance, medical insurance, ...
How long does it take to get Medicare referrals?
Recipients under age 65 get an automatic referral for Medicare after 24 months of payments. Persons with end-stage renal disease or ALS get automatic eligibility when diagnosed.
What is the Social Security Administration?
These dates determine rights later in the process. The Social Security Administration is a partner agency with the Centers for Medicare and Medicaid. It promotes Medicare and has an important portal for providing information on eligibility. You can find out if you’re eligible in a matter of minutes.
How long is the initial enrollment period for Medicare?
The Initial Enrollment Period is the seven-month period that includes the month of the 65th birthday. The period runs from three months before the birthday month, and for three months afterward . This is the ideal time to review options and make choices for Medicare coverage.
How long does medicaid last?
Benefits also may be covered retroactively for up to three months prior to the month of application, if the individual would have been eligible during that period had he or she applied. Coverage generally stops at the end of the month in which a person no longer meets the requirements for eligibility.
What is Medicaid coverage?
Medicaid is the single largest source of health coverage in the United States. To participate in Medicaid, federal law requires states to cover certain groups of individuals. Low-income families, qualified pregnant women and children, and individuals receiving Supplemental Security Income (SSI) are examples of mandatory eligibility groups (PDF, ...
What is Medicaid Spousal Impoverishment?
Spousal Impoverishment : Protects the spouse of a Medicaid applicant or beneficiary who needs coverage for long-term services and supports (LTSS), in either an institution or a home or other community-based setting, from becoming impoverished in order for the spouse in need of LTSS to attain Medicaid coverage for such services.
What is dual eligible for Medicare?
Eligibility for the Medicare Savings Programs, through which Medicaid pays Medicare premiums, deductibles, and/or coinsurance costs for beneficiaries eligible for both programs (often referred to as dual eligibles) is determined using SSI methodologies..
What is MAGI for Medicaid?
MAGI is the basis for determining Medicaid income eligibility for most children, pregnant women, parents, and adults. The MAGI-based methodology considers taxable income and tax filing relationships to determine financial eligibility for Medicaid. MAGI replaced the former process for calculating Medicaid eligibility, ...
What is 209b spending?
In addition to states with medically needy programs, 209 (b) states also must allow a spenddown to the income eligibility levels eligibility groups based on blindness, disability, or age (65 and older), even if the state also has a medically needy program. Thirty-six states and the District of Columbia use spenddown programs, ...
How many people are covered by medicaid?
Medicaid is a joint federal and state program that, together with the Children’s Health Insurance Program (CHIP), provides health coverage to over 72.5 million Americans, including children, pregnant women, parents, seniors, and individuals with disabilities. Medicaid is the single largest source of health coverage in the United States.
How many people are covered by medicaid?
Medicaid also provides coverage to 4.8 million people with disabilities who are enrolled in Medicare.
Can you be covered by Medicare and Medicaid?
Individuals who are enrolled in both Medicaid and Medicare, by federal statute, can be covered for both optional and mandatory categories.
Can Medicare help with out of pocket medical expenses?
Medicare enrollees who have limited income and resources may get help paying for their premiums and out-of-pocket medical expenses from Medicaid (e.g. MSPs, QMBs, SLBs, and QIs).