There are 2 general eligibility requirements to qualify for a Medicare Advantage plan (Medicare Part C):
- You must be enrolled in Original Medicare (Medicare Part A and Part B).
- You must live in the service area of a Medicare Advantage insurance provider that is accepting new users during your...
Full Answer
How do I know if I have Medicare Advantage?
Nov 18, 2021 · There are 2 general eligibility requirements to qualify for a Medicare Advantage plan (Medicare Part C): 1. You must be enrolled in Original Medicare (Medicare Part A and Part B). 2. You must live in the service area of a Medicare Advantage insurance provider that is accepting new users during ...
How to switch from Original Medicare to Medicare Advantage?
How to join a Medicare Advantage Plan. Use Medicare's Plan Finder. Visit the plan's website to see if you can join online. Fill out a paper enrollment form. Contact the plan to get an enrollment form, fill it out, and return it to the plan. All plans must offer …
How much can you make to qualify for Medicare?
Mar 14, 2022 · There are several ways to enroll in a Medicare Advantage plan. Complete an online enrollment form on the plan provider’s website. Complete a hard copy of the enrollment form and mail it to the provider. Call the insurance company support line. Call Medicare at 1-800-633-4227.
How do I enroll in Medicare Advantage?
Oct 13, 2021 · In most cases, here’s all you need to qualify for a Medicare Advantage plan. You must: Be enrolled in Medicare Part A and Part B, or be eligible for them Live within the plan’s service area. That means that when you find a plan you’d like to sign up for, make sure the plan serves the county where you live. Read more on this later in this article.
Can I be turned down for a Medicare Advantage plan?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
How do you qualify for a Medicare Advantage plan?
1. You must be enrolled in Original Medicare (Medicare Part A and Part B). 2. You must live in the service area of a Medicare Advantage insurance provider that is accepting new users during your application period.Nov 18, 2021
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
Why is Medicare Advantage being pushed so hard?
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.Feb 24, 2021
What are 4 types of Medicare Advantage plans?
Medicare Advantage PlansHealth Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
Can you have Medicare and Medicare Advantage at the same time?
If you join a Medicare Advantage Plan, you'll still have Medicare but you'll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. You must use the card from your Medicare Advantage Plan to get your Medicare- covered services.
Is Medicare Advantage more expensive than Medicare?
Clearly, the average total premium for Medicare Advantage (including prescription coverage and Part B) is less than the average total premium for Original Medicare plus Medigap plus Part D, although this has to be considered in conjunction with the fact that an enrollee with Original Medicare + Medigap will generally ...Nov 13, 2021
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.Dec 21, 2021
Which company has the best Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
Does Medicare cover dental?
Dental services Medicare doesn't cover most dental care (including procedures and supplies like cleanings, fillings, tooth extractions, dentures, dental plates, or other dental devices). Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
How Much Does Medicare Advantage Cost?
The average premium for a Medicare Advantage plan in 2021 was $21.22 per month. For 2022 it will be $19 per month. Although this is the average, some premiums cost $0, and others cost well over $100. For more resources to help guide you through the complex world of medical insurance, visit our Medicare hub.
How old do you have to be to qualify for Medicare?
To qualify for Original Medicare, you must be: An American citizen or permanent legal resident of at least 5 years in a row. Aged 65 or older, or eligible due to disability.
Is Medicare Advantage different from Original Medicare?
Qualifying for a Medicare Advantage plan is actually not too different from qualifying for Original Medicare, Part A and Part B.
What age do you have to be to get Medicare Advantage?
Most people qualify for Medicare Part A and Part B when they turn age 65 or have received disability benefits from the Social Security Administration or Railroad Retirement Board ...
What is Medicare Advantage Plan?
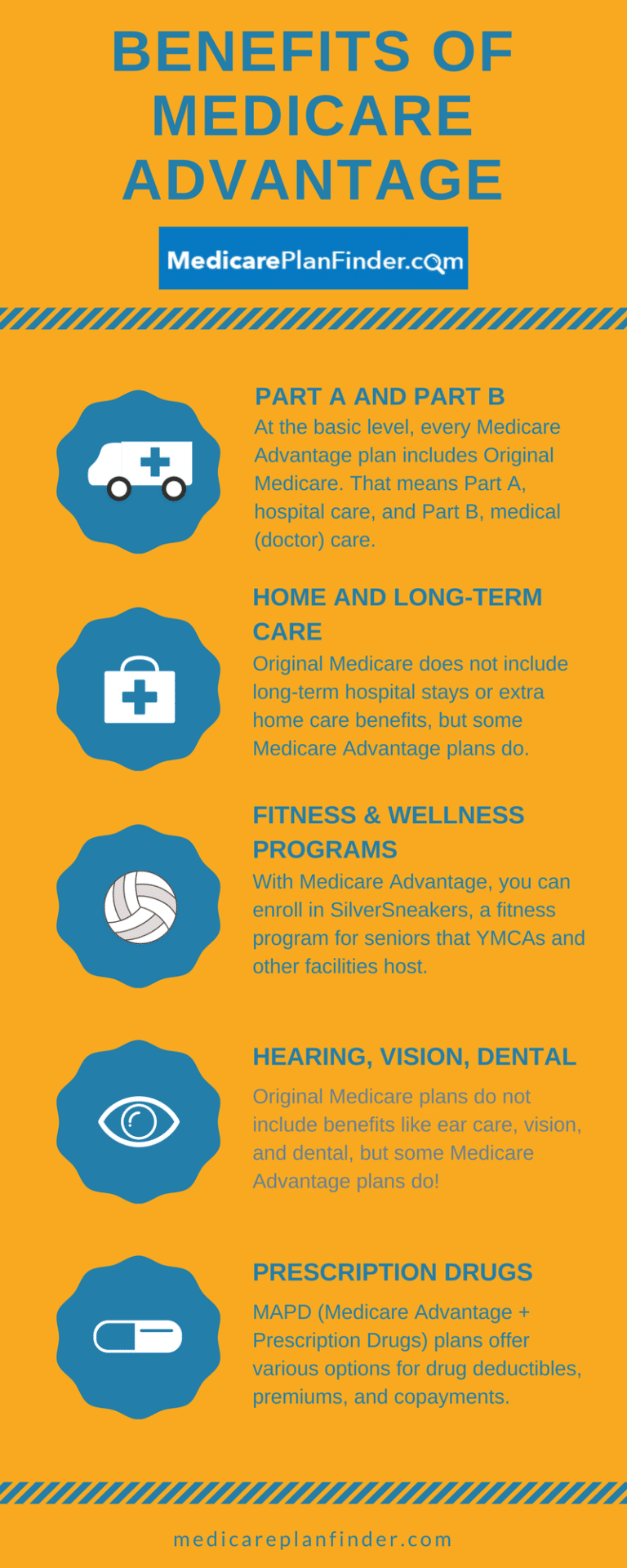
Medicare Advantage plans are an alternative way for people to receive their Medicare Part A (hospital) and Part B (medical) benefits from private insurance companies approved by Medicare.
Do I have to pay Medicare Part B premium?
You must pay the Medicare Part B premium. Typically, you are still responsible for paying your Medicare Part B premium when you enroll in a Medicare Advantage plan. An exception may exist for people with limited incomes that qualify them for a Part B premium government subsidy. In addition to the Medicare Part B premium, ...
What is Medicare Advantage?
According to Medicare.gov, Medicare Advantage (also known as Medicare Part C) plans are a type of Medicare health plan. They are offered by a private company that contracts with Medicare to provide all your Part A and Part B benefits. In addition, most Medicare services are covered through Medicare Advantage.
Can I Switch From a Medicare Advantage Plan back to Original Medicare?
You can switch plans by joining the plan of your choice during enrollment periods. You will be automatically disenrolled from your old plan when your new plan begins. Enrollment periods for switching back to Original Medicare are October 15 through December 7 and January 1-March 31.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What is Medicare Advantage?
Medicare Advantage is private insurance's counterpart to Original Medicare. It's a great alternative for receiving your Medicare coverage. Rather than purchasing individual components through Original Medicare, Medicare Advantage bundles benefits from Part A and Part B and can even include drug coverage, vision, dental, hearing, ...
How to find my Medicare number?
Go to the Medicare Plan Finder. If you'd like to save your search results, choose the "Log in or Create Account" option and enter your Medicare number, email address, and other information. If you just want to do a quick search, select "Continue without logging in."
How long does Medicare Advantage last?
If you’re new to Medicare, you’ll want to enroll in an MA Plan during your Initial Enrollment Period (IEP). This period lasts for seven months— three months before the month when you turn 65, and three months after.
When is the open enrollment period for Medicare?
There’s also a Fall Open Enrollment Period (October 15 through December 7) during which you may sign up. Learn about enrollment periods and when they apply to you.
How to change Medicare Advantage plan?
The Medicare Open Enrollment Period, also known as the Annual Election Period (AEP), runs yearly from October 15 to December 7, during which Medicare beneficiaries can apply for Medicare Advantage plan coverage. Beneficiaries can make the following changes to their coverage during this two-month period: 1 Switch from Original Medicare to Medicare Advantage 2 Switch from a Medicare Advantage plan back to Original Medicare 3 Switch from a Medicare Advantage plan to a different Medicare Advantage plan in their service area 4 Switch from a Medicare Advantage plan that doesn’t include drug coverage to one that does, and vice versa
How long does it take to enroll in Medicare Advantage?
Enrolling in a Medicare Advantage plan during your Initial Enrollment Period. When you first become eligible for Medicare, you have a 7-month Initial Enrollment Period (IEP) to enroll in Medicare. Then once enrolled in Part A and Part B, you can sign up for a Medicare Advantage plan (also known as Medicare Part C).
What is Medicare Advantage?
Medicare Advantage plans are provided through private insurance companies and offer the same benefits as Original Medicare, with some also offering prescription drug coverage and vision, dental or hearing care.
What happens if you miss the enrollment period?
If you missed the other enrollment periods, you generally have to wait for the next Annual Election Period. However, there are certain special circumstances that could qualify you for a Special Enrollment Period, such as: You moved out of your current Medicare Advantage plan’s service area. You are eligible for Medicaid.
When is Medicare open enrollment?
The Medicare Open Enrollment Period, also known as the Annual Election Period (AEP), runs yearly from October 15 to December 7 , during which Medicare beneficiaries can apply for Medicare Advantage plan coverage.
When does IEP end?
If you are aging into Medicare, then your IEP begins 3 months before the month that you turn 65 and ends 3 months after the month you turn 65. For example, if you age into Medicare in May, then your Initial Enrollment Period begins February 1st and ends August 31st. People with End-Stage Renal Disease generally cannot enroll in a Medicare Advantage ...
How does Medicare work with my job-based health insurance when I stop working?
Once you stop working, Medicare will pay first and any retiree coverage or supplemental coverage that works with Medicare will pay second.
When & how do I sign up for Medicare?
You can sign up anytime while you (or your spouse) are still working and you have health insurance through that employer. You also have 8 months after you (or your spouse) stop working to sign up.
Do I need to get Medicare drug coverage (Part D)?
Prescription drug coverage that provides the same value to Medicare Part D. It could include drug coverage from a current or former employer or union, TRICARE, Indian Health Service, VA, or individual health insurance coverage.