If you are already enrolled in Medicare Part A and you would like to enroll in Part B under the Special Enrollment Period (SEP), you can apply online at Apply for Medicare Part B Online during a Special Enrollment Period. You can upload your application and documents that verify your group health plan coverage through your employer.
Full Answer
How do you add Part B to Medicare?
· Views: 97809. If you are already enrolled in Medicare Part A and you would like to enroll in Part B under the Special Enrollment Period (SEP), you can apply online at Apply for Medicare Part B Online during a Special Enrollment Period. You can upload your application and documents that verify your group health plan coverage through your employer. You can also …
Do I need Medicare Part B?
· To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS 40B) and the request for employment information form (CMS L564). You’ll complete the Medicare enrollment application and give the request for employment information form to the employer to fill out.
Where can I buy Medicare Part B?
· You would like to enroll in Part B during the Special Enrollment Period. You can complete form CMS-40B ( Application for Enrollment in Medicare – Part B [Medical Insurance]) and CMS-L564 (Request for Employment Information) online. You can also fax the CMS-40B and CMS-L564 to 1-833-914-2016; or return forms by mail to your local Social Security office .
Where to get Medicare Part B?
using our online Medicare application at www.ssa.gov If you already have Medicare Part A: 1. Go to “Apply Online for Medicare Part B During a Special Enrollment Period” and complete CMS-40B and CMS-L564. Then, upload your evidence of Group Health Plan or Large Group Health Plan. 2. Fax your CMS-40B and employer-signed CMS-L564 forms to

Can you add Medicare Part B at any time?
You can sign up for Medicare Part B at any time that you have coverage through current or active employment. Or you can sign up for Medicare during the eight-month Special Enrollment Period that starts when your employer or union group coverage ends or you stop working (whichever happens first).
How do I add Part B to my Medicare online?
You can use one of the following options to submit your enrollment request under the Special Enrollment Period: Go to “Apply Online for Medicare Part B During a Special Enrollment Period” and complete CMS-40B and CMS-L564. Then upload your evidence of Group Health Plan or Large Group Health Plan.
How long does it take for Medicare Part B to be approved?
You can also call the Social Security Administration at 1-800-772-1213 or go to your local Social Security office. It takes about 45 to 90 days to receive your acceptance letter after submitting your Medicare application.
How do I submit Medicare Part B?
Contact Social Security to sign up for Part B:Fill out Form CMS-40B (Application for Enrollment in Medicare Part B). ... Call 1-800-772-1213. ... Contact your local Social Security office.If you or your spouse worked for a railroad, call the Railroad Retirement Board at 1-877-772-5772.
Can I fax my part B application to Social Security?
You can also fax or mail your completed CMS-40B, Application for Enrollment in Medicare – Part B (Medical Insurance) and the CMS-L564, Request for Employment Information enrollment forms and evidence of employment to your local Social Security office.
What documents do I need to apply for Medicare?
What documents do I need to enroll in Medicare?your Social Security number.your date and place of birth.your citizenship status.the name and Social Security number of your current spouse and any former spouses.the date and place of any marriages or divorces you've had.More items...
Is Medicare Part B automatically deducted from Social Security?
Yes. In fact, if you are signed up for both Social Security and Medicare Part B — the portion of Medicare that provides standard health insurance — the Social Security Administration will automatically deduct the premium from your monthly benefit.
Can Medicare Part B be backdated?
This process allows individuals to request immediate or retroactive enrollment into Part B and the elimination of late enrollment penalties from the Social Security Administration (SSA).
Do you have to enroll in Medicare Part B every year?
For Original Medicare (Parts A and B), there are no renewal requirements once enrolled. Medigap plans ― also known as Medicare Supplement plans ― auto renew annually unless you make a change.
How long before you turn 65 do you apply for Medicare?
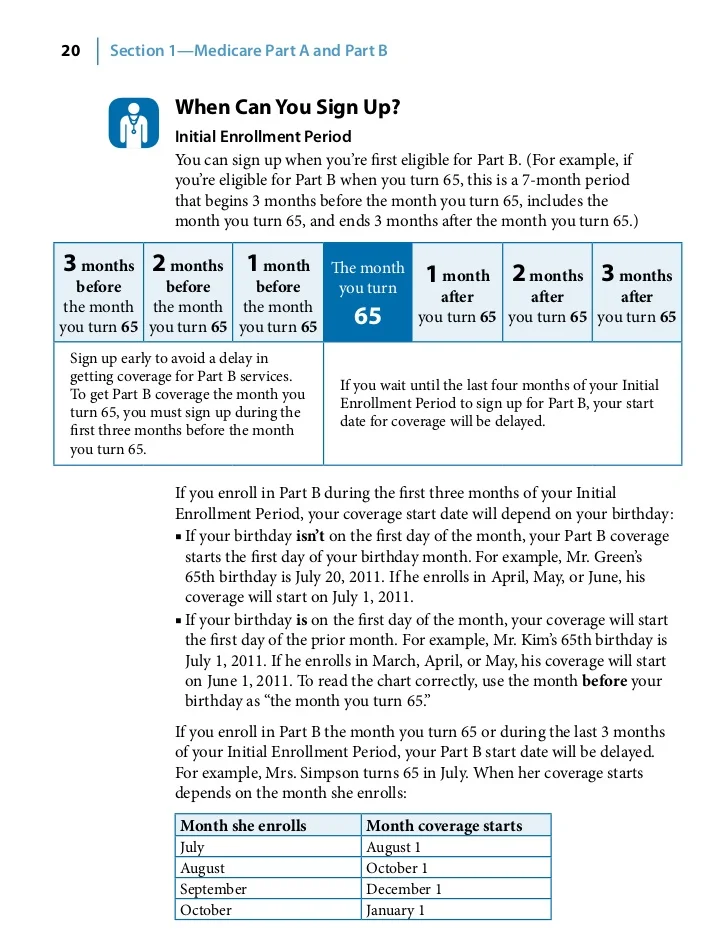
3 monthsYour first chance to sign up (Initial Enrollment Period) It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is the maximum income to qualify for Medicare?
To qualify, your monthly income cannot be higher than $1,010 for an individual or $1,355 for a married couple. Your resource limits are $7,280 for one person and $10,930 for a married couple. A Qualifying Individual (QI) policy helps pay your Medicare Part B premium.
What is the Medicare Part B special enrollment period (SEP)?
The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 month...
Do I qualify for the Medicare Part B special enrollment period?
You qualify for the Part B SEP if: you are eligible for Medicare because of your age or because you collect disability benefits. (People who have E...
How do I use the Part B SEP?
To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS...
What if an employer gives me money to buy my own health plan?
A note about individual coverage: you’ll qualify for an SEP if you delayed Part B because you had employer-sponsored coverage through a group healt...
Why Would I Need A Medicare Special Enrollment period?
Medicare has limited enrollment periods for Part A and Part B. Many people are automatically enrolled when they turn 65 or qualify through disabili...
When Might I Qualify For A Medicare Special Enrollment period?
Certain situations may qualify you to enroll in Part A and/or Part B using a Medicare Special Enrollment Period. Some qualifying situations may inc...
Medicare Special Enrollment Period For The Working Aged
If you (or your spouse) are still working when you turn 65 and have group coverage through an employer or union, you can generally delay Part A and...
Medicare Special Enrollment Period For International Volunteers
Individuals volunteering in a foreign country may be able to enroll in Part A and/or Part B with a Medicare Special Enrollment Period when they ret...
Medicare Special Enrollment Period For Disabled Tricare Beneficiaries
TRICARE is health insurance for retired and active-duty service members and their families. If you’re a retired service member, you must enroll in...
Medicare Special Enrollment Period If You Were Living Overseas
There are other situations where you may be able to enroll in Medicare outside of normal enrollment periods without a Special Enrollment Period. Th...
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
What to do if your Social Security enrollment is denied?
If your enrollment request is denied, you’ll have the chance to appeal.
How many forms do you need to submit to get SEP?
Beneficiaries must submit two forms to get approval for the SEP.
How to use SEP form?
To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS 40B) and the request for employment information form (CMS L564). You’ll complete the Medicare enrollment application and give the request for employment information form to the employer to fill out. You want to request additional copies of form L564 from Social Security if you’ve been covered through more than one job-based plan since you qualified for Medicare.
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
Can disabled people get SEP?
People 65 and older only qualify for this SEP if they have coverage through their own or their spouse’s job, but disabled individuals can also qualify because they’re covered by a non-spouse family member’s plan.
How to contact Social Security about Part B?
Please contact Social Security at 1-800-772-1213 ( TTY 1-800-325-0778) if you have any questions. Note: When completing the forms: State, “I want Part B coverage to begin (MM/YY)” in the remarks section of the CMS-40B form or online application. If your employer is unable to complete Section B, please complete that portion as best you can on behalf ...
Do you have to leave home to sign up for Medicare Part B?
For many people, signing up for Medicare Part B doesn’t require you to leave the comfort of home. Please visit our Medicare Part B webpage if: You are already enrolled in Medicare Part A. You would like to enroll in Part B during the Special Enrollment Period.
How to contact Medicare for Part B?
For more information on Part B enrollment for U.S. citizens living abroad, contact Medicare at 1-800-MEDICARE (1-800-633-4227) . If you’re a TTY user, call 1-877-486-2048. Customer service representatives can be reached 24 hours a day, seven days a week.
What is a SEP in Medicare?
A Medicare Special Enrollment Period (SEP) can let you sign up for Original Medicare Part A and/or Part B outside of regular enrollment periods. If you’re not eligible for an SEP, you’ll have usually to wait until the next General Enrollment Period to sign up for Part A and/or Part B. You might also have to pay a late enrollment penalty ...
How long do you have to enroll in a new insurance plan?
You have eight months to enroll, beginning the month that employment or employment-based coverage ends – whichever happens first. You may not have to pay a late enrollment penalty for not enrolling when you were first eligible.
How many times can you use Medicare Special Enrollment?
The month that the person is notified of Part A enrollment. This Medicare Special Enrollment Period can only be used one time during the TRICARE beneficiary’s lifetime.
Does Cobra count as Medicare?
Keep in mind that COBRA and retiree health insurance don’t count as coverage based on current employment and won’t qualify you for a Medicare Special Enrollment Period when it ends. You also won’t get a Medicare Special Enrollment Period if your group coverage or employment ends during your Medicare Initial Enrollment Period.
How long do you have to enroll in Medicare if you are still working?
When that employment – or your health coverage – ends, you can typically enroll in Part A and Part B with a Medicare Special Enrollment Period. You have eight months to enroll, beginning the month that employment or employment-based coverage ends – whichever happens first. You may not have to pay a late enrollment penalty for not enrolling when you were first eligible.
When does Medicare enroll in Part A?
Medicare has limited enrollment periods for Part A and Part B. Many people are automatically enrolled when they turn 65 or qualify through disability. Read about automatic enrollment and Medicare’s usual enrollment periods.
What is a SEP in health insurance?
You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or.
How old do you have to be to get Medicare?
If you are age 65 or older, you or your spouse are still working and you are covered under a group health plan based on that current employment, you may not need to apply for Medicare medical insurance (Part B) at age 65. You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: 1 During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or 2 In the eight-month period that begins with the month after your group health plan coverage or the current employment it is based on ends, whichever comes first.#N#Exception: If your group health plan coverage or the employment it is based on ends during your initial enrollment period for Medicare Part B, you do not qualify for a SEP. Your initial enrollment period starts three months before the month you attain age 65 and ends three months after the month you turn 65. 3 If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months.
Can you get a SEP if you have cobra?
If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months. Note : COBRA and retiree health plans aren't considered coverage based on current employment. If you have that type of coverage, you will not be eligible for a SEP when it ends.
Can you get a SEP if you have a group health plan?
Exception: If your group health plan coverage or the employment it is based on ends during your initial enrollment period for Medicare Part B, you do not qualify for a SEP.
Do people on Social Security have a special enrollment period?
People who receive Social Security disability benefits and are covered under a group health plan from either their own or a family member's current employment also have a special enrollment period and premium rights similar to those for workers age 65 or older.
What can I do with my Medicare Advantage Plan?
What can I do? Join a Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Switch from your current plan to another Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Drop your Medicare Advantage Plan with drug coverage and return to Original Medicare .
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
When can you make changes to your health insurance plan?
Whenever your employer or union allows you to make changes in your plan .
Why does Medicare take an action?
Medicare takes an official action (called a "sanction") because of a problem with the plan that affects me.
What to do if you made wrong choice on Medicare?
Call center representatives can help you throughout the year with options for making changes.
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
When does the 8 month special enrollment period start?
Your 8-month Special Enrollment Period starts when you stop working, even if you choose COBRA or other coverage that’s not Medicare.
What is a Medicare leave period?
A period of time when you can join or leave a Medicare-approved plan.
How long can you join a health insurance plan?
You can join a plan anytime while you have job-based health insurance, and up to 2 months after you lose that insurance.
What happens if you miss the 8 month special enrollment period?
If you miss this 8-month Special Enrollment Period, you’ll have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B. The penalty goes up the longer you wait to sign up.
Does Cobra end with Medicare?
Your COBRA coverage will probably end when you sign up for Medicare. (If you get Medicare because you have End-Stage Renal Disease and your COBRA coverage continues, it will pay first.)
Do you have to tell Medicare if you have non-Medicare coverage?
Each year your plan must tell you if your non-Medicare drug coverage is creditable coverage. Keep this information — you may need it when you’re ready to join a Medicare drug plan. (Don’t send this information to Medicare.)