How do I submit Medicare primary/Blue plan secondary claims? • For members with Medicare primary coverage and Blue plan secondary coverage, submit claims to your Medicare intermediary and/or Medicare carrier. • When submitting the claim, it is essential that you enter the correct Blue plan name as the secondary carrier.
Full Answer
How do I submit a Medicare Secondary claim?
All professional and institutional providers should submit Medicare Secondary claims electronically. If a paper claim is submitted, it must be accompanied by a copy of the Medicare EOB. Electronic claims will need to contain specific information in the 837 claims transaction set.
How do I bill Medicare as the secondary payer?
You must follow the MSP rules and bill Medicare as the secondary payer after the primary payer has made payment. We’ll inform you on your remittance advice how much you can collect from the patient after we make payment. NOTE:
Is Medicare primary or secondary?
Is Medicare Primary or Secondary? - Who Pays First - MedicareFAQ Medicare is always primary if it’s your only form of coverage. When you introduce another form of coverage into the picture, there’s predetermined coordination of benefits.
How do I determine if Medicare is the primary payer?
Determine if Medicare is the primary payer by asking patients or their representative(s) for MSP information. Bill primary payer before billing Medicare. Submit an Explanation of Benefits (EOB) or remittance advice from the primary payer with all MSP information.
What is Medicare Secondary Payer?
When did Medicare start?
Why is Medicare conditional?
How long does ESRD last on Medicare?
What age is Medicare?
Does GHP pay for Medicare?
Does Medicare pay for workers compensation?
See more
About this website
How do I file Medicare secondary claims electronically?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.
How do I bill Medicare Secondary?
When Medicare is the secondary payer, submit the claim first to the primary insurer. The primary insurer must process the claim in accordance with the coverage provisions of its contract.
Do you submit primary and secondary insurance at the same time?
It is a common mistake to think that primary and secondary insurance claims get billed out at the same time. However, this is incorrect. When billing for primary and secondary claims, the primary claim is sent before the secondary claim.
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
When the same BCBS payer issues the primary and secondary or supplemental policies?
Commercial Ins/ BCBSQuestionAnswerwhen same payer issues the primary, secondary, or supplemental policiesyou would submit one claim for all policiesmandatory second surgical system is necessary whenpatient is considering elective, non-emergency surgical care33 more rows
Is Medicare secondary or primary?
primaryMedicare is primary and your providers must submit claims to Medicare first. Your retiree coverage through your employer will pay secondary.
How does billing work with 2 insurances?
If you have multiple health insurance policies, you'll have to pay any applicable premiums and deductibles for both plans. Your secondary insurance won't pay toward your primary's deductible. You may also owe other cost sharing or out-of-pocket costs, such as copayments or coinsurance.
How do you use two health insurance plans?
When you have two health insurance plans, this doesn't mean that you'll be fully covered twice by each insurance plan. Instead, one will need to be assigned as your primary plan, while the other will take the secondary spot. That means the total amount that your two plans pay will never exceed 100% of the cost.
How do you determine which insurance is primary and which is secondary?
The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" to pay. The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer.
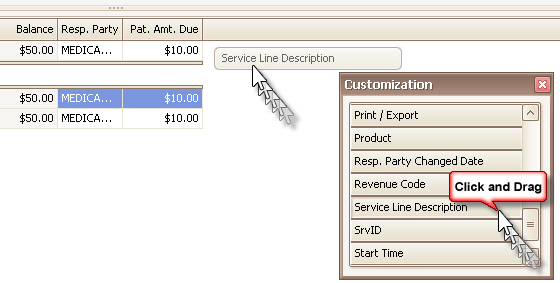
When submitting a secondary claim what fields will the secondary insurance be in?
Secondary insurance of the patient is chosen as primary insurance for this secondary claim; primary insurance in the primary claim is chosen as secondary insurance in the secondary claim. Payment received from primary payer should be put in 'Amount Paid (Copay)(29)' field in Step-2 of Secondary claim wizard.
How do Medicare crossover claims work?
1. What is meant by the crossover payment? When Medicaid providers submit claims to Medicare for Medicare/Medicaid beneficiaries, Medicare will pay the claim, apply a deductible/coinsurance or co-pay amount and then automatically forward the claim to Medicaid.
Who files Medicare supplement claims?
Your Medicare Part A and B claims are submitted directly to Medicare by your providers (doctors, hospitals, labs, suppliers, etc.). Medicare takes approximately 30 days to process each claim.
Medicare Secondary Payer Fact Sheet for Provider, Physician, and Other ...
Title: Medicare Secondary Payer Fact Sheet for Provider, Physician, and Other Supplier Billing Staff Author: CMS/CMM/PCG/DPIPD Subject: Medicare Secondary Payer Fact Sheet for Provider, Physician, and Other Supplier Billing Staff
Medicare Secondary Payer (MSP) Manual
10 - General Information (Rev. 81, Issued: 07-29-11, Effective: 01-01-12, Implementation: 01-03-12) Medicare Part A and Part B Contractors obtain information pertinent to the identification
Medicare Secondary Payer - CMS
Medicare econdary Payer MLN Booklet Page 3 of 16 MLN006903 April 2021. What’s Changed? Clarified policy on accepting payment for services if another insurer is primary to Medicare
Is Medicare Primary or Secondary? - Who Pays First - MedicareFAQ
Group Coverage Through Small Employer. If your employer has fewer than 20 employees, Medicare will be your primary coverage and the employer coverage will be your secondary coverage.If you do not enroll in Part B, your employer coverage will not pay their portion of your medical claims.
Medicare Secondary Payer (MSP): Condition, Occurrence, Value, and ...
February 12, 2013 – Revised 10.01.15. Medicare Secondary Payer (MSP): Condition, Occurrence, Value, and Patient Relationship, and Remarks Field Codes. This article includes tables of some of the most common Condition, Occurrence, Value, Patient Relationship, and Remarks Field Codes associated with MSP claims.
Medicare Secondary Payer Billing & Adjustments (Home Health & Hospice)
Does an MSP record appear on the beneficiary’s eligibility file? Are you aware of an MSP situation? NO YES Contact the BCRC at 1.855.798.2627 NO Submit claim to Medicare as primary.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Does Medicare pay for workers compensation?
Medicare generally will not pay for an injury or illness/disease covered by workers’ compensation. If all or part of a claim is denied by workers’ compensation on the grounds that it is not covered by workers’ compensation, a claim may be filed with Medicare.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
Regulation Requirements
Wait 30 days from the Medicare Explanation of Benefits (EOB) date before submitting your secondary claim.
How to Submit
All professional and institutional providers should submit Medicare Secondary claims electronically. If a paper claim is submitted, it must be accompanied by a copy of the Medicare EOB.
How to learn more about Medicare?
How to Learn More About Your Medicare Options. Primary insurance isn't too hard to understand; it's just knowing which insurance pays the claim first. Medical billing personnel can always help you figure it out if you're having trouble. While it's not hard to understand primary insurance, Medicare is its own beast.
Is Medicare primary insurance in 2021?
Updated on July 13, 2021. Many beneficiaries wonder if Medicare is primary insurance. But, the answer depends on several factors. While there are times when Medicare becomes secondary insurance, for the most part, it’s primary. Let’s go into further detail about what “primary” means, and when it applies.
Is Medicare a primary or secondary insurance?
Mostly, Medicare is primary. The primary insurer is the one that pays the claim first, whereas the secondary insurer pays second. With a Medigap policy, the supplement is secondary. Medicare pays claims first, and then Medigap pays. But, depending on the other policy, you have Medicare could be a secondary payer.
Does Medicare pay your claims?
Since the Advantage company pays the claims, that plan is primary. Please note that Medicare WON’T pay your claims when you have an Advantage plan. Medicare doesn’t become secondary to an Advantage plan. So, you’ll rely on the Advantage plan for claim approvals.
Is Medicare a part of tricare?
Medicare is primary to TRICARE. If you have Part A, you need Part B to remain eligible for TRICARE. But, Part D isn’t a requirement. Also, TRICARE covers your prescriptions. Your TRICARE will be similar to a Medigap plan; it covers deductibles and coinsurances.
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer. This booklet gives an overview of the MSP provisions and explains your responsibilities in detail.
What happens if you don't file a claim with the primary payer?
File proper and timely claims with the primary payer. Not filing proper and timely claims with the primary payer may result in claim denial. Policies vary depending on the payer; check with the payer to learn its specific policies.
Why does Medicare make a conditional payment?
Medicare may make pending case conditional payments to avoid imposing a financial hardship on you and the patient while awaiting a contested case decision.
What is a COB in health insurance?
Coordination of Benefits (COB) allows plans to determine their payment responsibilities. The BCRC collects, manages, and uploads information to the Common Working File (CWF) about patients’ other health insurance coverage. Providers, physicians, and other suppliers must collect accurate MSP patient information to ensure that claims are filed properly.
Can Medicare make a payment?
Medicare can’t make payment when payment “has been made or can reasonably be expected to be made” under liability insurance (including self-insurance), no-fault insurance, or a WC law or plan of the United States, called a primary plan.
Can Medicare deny a claim?
Medicare may mistakenly pay a claim as primary if it meets all billing requirements, including coverage and medical necessity guidelines . However, if the patient’s CWF MSP record shows another insurer should pay primary to Medicare, we deny the claim.
Who must first bill the other insurance company before Medical Assistance will pay the claim?
If a recipient is covered by other insurance or third party benefits such as Worker’s Compensation, CHAMPUS or Blue Cross/Blue Shield, the provider must first bill the other insurance company before Medical Assistance will pay the claim. PROPER COMPLETION OF CMS-1500.
Do you need to complete 17-17B?
Required. Note: Completion of 17-17b is only required for Lab and Other Diagnostic Services.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Does Medicare pay for workers compensation?
Medicare generally will not pay for an injury or illness/disease covered by workers’ compensation. If all or part of a claim is denied by workers’ compensation on the grounds that it is not covered by workers’ compensation, a claim may be filed with Medicare.
