Send paper claims to: Palmetto GBA Railroad Medicare P.O. Box 10066 Augusta Augusta, officially Augusta–Richmond County, is a consolidated city-county on the central eastern border of the U.S. state of Georgia. The city lies across the Savannah River from South Carolina at the head of its navigable portion. Georgia's second-largest city after Atlanta, Augusta is loca…Augusta
How do I enroll for electronic claims with railroad Medicare?
Before filing claims electronically to Railroad Medicare, you must have an EDI enrollment packet on file with Palmetto GBA. See our Electronic Data Interchange (EDI) resources for more information on enrolling for electronic claim submissions.
What is the fax number for Medicare for railroad Medicare?
Fax 532 (invoice) and 733 (opt out providers) ADS Letters to: (803) 264-0697 Railroad Medicare does not accept CMS-1500 claim forms via fax. View our main Contact Us page for information on how to submit a general inquiry or to contact a different department.
How do I get a railroad Medicare ptan?
Once Railroad Medicare receives a CMS-1500 (02/12) form, we will obtain your enrollment data from your local MAC and issue you a Railroad Medicare PTAN if everything can be verified on the MAC’s file, including the Tax Identification Number (TIN) (item 25), billing name and billing address (item 33).
How do I file a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Can you submit claims to Medicare electronically?
How to Submit Claims: Claims may be electronically submitted to a Medicare Administrative Contractor (MAC) from a provider using a computer with software that meets electronic filing requirements as established by the HIPAA claim standard and by meeting CMS requirements contained in the provider enrollment & ...
What is the EDI number for railroad Medicare?
888-355-9165The packet contains forms and explanations for each of the services offered by our Electronic Data Interchange (EDI) department. For further information regarding any of this material, please call the Railroad Medicare Provider Contact Center at 888-355-9165.
Does railroad Medicare have a provider portal?
Palmetto GBA Railroad Medicare is pleased to offer eServices, our free Internet-based, provider self-service portal. The application provides information access over the Web for the following online services: Eligibility.
Is railroad Medicare the same as Medicare?
A: The only difference is that retired railroad beneficiaries have their Part B benefits administered by the Palmetto GBA Railroad Retirement Board Specialty Medicare Administrative Contractor (RRB SMAC) regardless of where they live. Members should be certain to advise providers of this when they receive treatment.
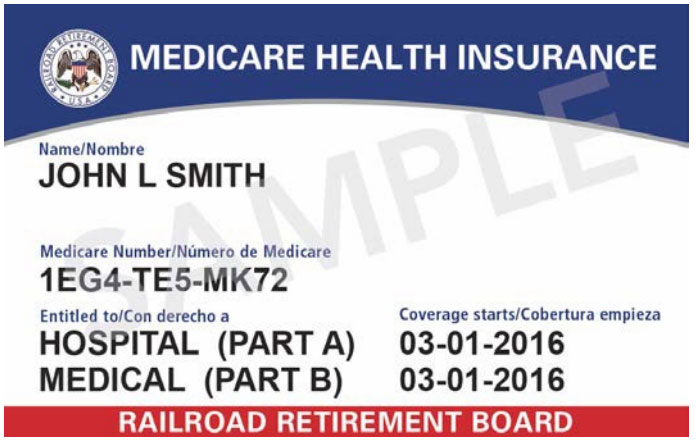
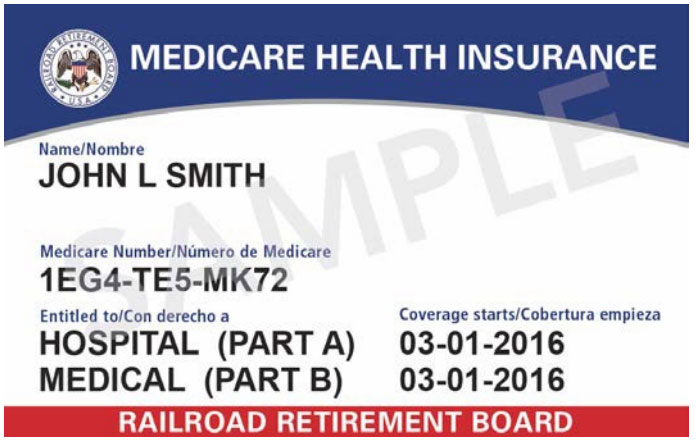
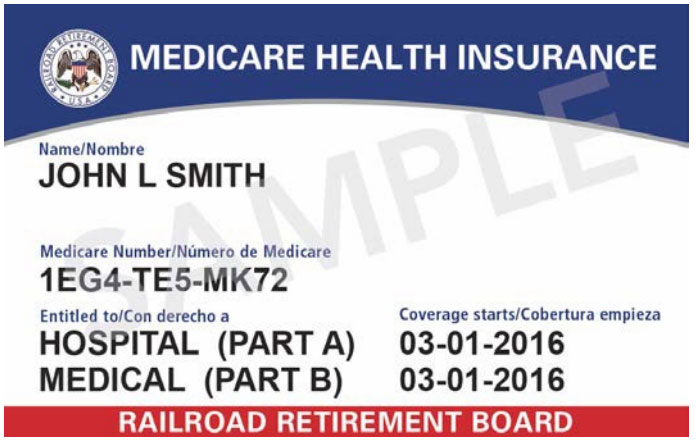
What do Railroad Medicare ID numbers look like?
It will contain capital letters (all letters with the exception of S, L, O, I, B and Z) and numbers (0-9). The 2nd, 5th, 8th, and 9th characters will always be a letter, while characters 1, 4, 7, 10, and 11 will always be a number. The 3rd and 6th characters will be a letter or a number.
What is an EDI submitter?
A Submitter ID number is a unique number identifying electronic submitters. A Submitter ID can be used to transmit Part A, Part B and HHH EDI transactions to CGS. You must request a Submitter ID if you will be submitting claims directly to CGS.
How do I check my railroad Medicare claims?
If you'd like to use the IVR, you can do so by calling 800–833–4455. From the main menu, press one (1) for claim status. You will need your Railroad Medicare number, date of birth, name, and date of service for the claim you are searching for. Claim status is available Monday thru Friday from 7 a.m. through 11 p.m. ET.
How do I add a provider to my Medicare RR?
Please call our Provider Contact Center at 888-355-9165 for assistance. Choose option 3 for Provider Enrollment.
Is railroad Medicare a Medicare Advantage Plan?
Yes, Railroad Medicare beneficiaries can choose to enroll in Medicare Advantage plans.
Who administers railroad Medicare?
As part of the retirement program, the RRB also has administrative responsibilities under the Social Security Act for certain benefit payments and railroad workers' Medicare coverage. In fiscal year 2021, the RRB paid retirement-survivor benefits of nearly $13.2 billion to about 519,000 beneficiaries.
Who is railroad Medicare?
The Medicare program covers railroad workers just like workers under social security. Railroad retirement payroll taxes include a Medicare hospital insurance tax just like social security payroll taxes.
Does railroad Medicare accept corrected claims?
In the case where a minor error or omission is involved, you can request that Railroad Medicare reopen the claim so the error or omission can be corrected rather than going through the written appeals process. Reopenings may be submitted in written form, over the telephone or through our eServices online portal.
Where do I file Part A, DMEPOS and Home Health and Hospice claims for Railroad Medicare beneficiaries?
Part A — The jurisdictional A/B Medicare Administrative Contractors (A/B MACs) process hospital facility claims and skilled nursing facility claims for both Medicare and Railroad Medicare beneficiaries. You can use the CMS MAC Website List to find your local A/B MAC.
How long does it take for Medicare to reject a claim?
Rejected claims must be corrected and resubmitted no later than 12 months from the date of service. Medicare will deny claims received after the deadline date.
What is DMEPOS in Medicare?
Durable medical equipment (DMEPOS) — The jurisdictional DME Medicare Administrative Contractors (DME MACs) process claims for DMEPOS items for both Medicare and Railroad Medicare beneficiaries. You can use the CMS MAC Website List to find your local DME MAC.
What is Medicare 277CA report?
If you submit claims via the Electronic Data Interchange (EDI) option, our ACE tool will return pre-adjudicated Part B claims information through a claim acknowledgement transaction report, called a Medicare 277CA report. Submitters will receive the Medicare 277CA report with ACE Smart Edits if a claim is identified as containing a potential claim submission error that requires the submitters attention.
How long does it take to file a claim with the MAC?
Claims must be filed to the appropriate MAC no later than 12 months, one calendar year, from the date of service. Timely filing is determined by the date a processable claim is received by the appropriate MAC.
Do you have to submit Medicare electronically to Railroad?
If you are required to submit electronically to your local Medicare Administrative Contractor (MAC), CMS requires you to submit electronically to Railroad Medicare, regardless of how many Railroad Medicare patients you may serve.
Do you need an EDI packet to file a Medicare claim?
Before filing claims electronically to Railroad Medicare, you must have an EDI enrollment packet on file with Palmetto GBA. See our Electronic Data Interchange (EDI) resources for more information on enrolling for electronic claim submissions.
What is a PTAN for Medicare?
Before billing Railroad Medicare, you must be enrolled with and have a Provider Transaction Access Number (PTAN) for your local Part B MAC. Because Railroad Medicare’s enrollment records will match what your local MAC has on file, please make sure your enrollment information is current with your MAC before requesting a Railroad Medicare PTAN.
Can you receive Medicare payments from railroad?
EFT allows a financial institution to deposit Railroad Medicare payments directly into a designated account. Once you have been established to receive funds EFT, you will no longer be eligible to receive your Railroad Medicare payments via paper checks.
How do I file a claim?
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
Call 888-355-9165, select Option 5 for Customer Service
Representatives are available Monday through Friday from 8:30 a.m. to 4:30 p.m. for all time zones with the exception of PT, which receives service from 8 a.m. to 4 p.m.
Contact a Different Department
View our main Contact Us page for information on how to submit a general inquiry or to contact a different department.
Provider Contact Center: 1-888-355-9165
Call the Provider Contact Center (PCC) to speak with representatives in Customer Service, Provider Enrollment, Electronic Data Interchange, eServices and Telephone Reopenings.
Interactive Voice Response (IVR): 1-877-288-7600
Use the IVR to request routine claim status, beneficiary eligibility, and payment information and to request a duplicate remittance advice.
Email Us
Use our contact form to submit general inquiries or to provide feedback on our website. For security reasons please do not submit requests involving PHI/PII with this form.
Contact Palmetto GBA Departments
For information on contacting a specific department by phone, email, fax, or for instructions on submitting documentation by mail, please select a department:
Feedback to the Railroad Retirement Board (RRB)
If you would like to send any feedback to the RRB regarding your experience with Palmetto GBA, please direct your comments to: [email protected] .
What Medicare Parts does RRB automatically enroll you in?
If you are receiving Railroad Retirement benefits or railroad disability annuity checks when you become eligible for Medicare, RRB should automatically enroll you in Medicare Parts A and B . You should receive your red, white, and blue Medicare card and a letter from RRB explaining that you have been enrolled in Medicare.
What to do if you are not collecting Railroad Retirement?
If you are not collecting Railroad Retirement benefits when you turn 65, you should contact your local RRB field office to enroll in Medicare. If you are under 65 and have a disability, you will have to fulfill different eligibility requirements to qualify for Medicare.
Do doctors have to bill Medicare Part B?
Your doctors and other providers should bill a separate contractor for services covered under Part B. Your providers must send Railroad Medicare Part B claims to the Part B contractor selected by RRB. Always make sure your providers know you have Railroad Medicare to ensure that Medicare pays in a timely manner.
Does RRB collect Medicare?
RRB will collect your Medicare premiums. If you receive Railroad Retirement benefits or railroad disability annuity checks, your Medicare Part B premium should be automatically deducted from your check each month. If you do not qualify for premium-free Part A, it will also be deducted from your check.
What information is needed for attachments for Medicare?
All attachments must identify the patient’s name, Medicare ID number, date of service and other pertinent information
How many service lines are required for a CMS 1500?
More than six service lines per CMS-1500 claim form. Do not compress two lines of information on one line. If more than six service lines are required, see instructions listed below under "Claims Submitted with Multiple Pages."
What is the CMS 1500 form?
The CMS-1500 claim form answers the needs of many insurers. It is the basic form prescribed by the Centers of Medicare & Medicaid Services (CMS) for the Medicare program for claims from physicians and suppliers. The revised version of the CMS 1500 claim form is version and is approved under the OMB control number 0938-1197.
When did Medicare stop making payments electronically?
Reminder: The Administrative Simplification and Compliance Act (ASCA) prohibits Medicare from making payments on claims not submitted electronically on or after October 16, 2003, unless a provider is small (fewer than 10 full-time equivalent employees for providers required to bill Medicare carriers) or meets one of the very few limited exceptions to this requirement.
Can a CMS 1500 claim be scanned?
If multiple CMS-1500 claim forms are submitted with totals on each claim form, the claims will be scanned as separate claims and not as multi-page claim.
Do you list other supplemental coverage in item 9?
Do not list other supplemental coverage in Item 9 and its subdivisions at the time a Medicare claim is filed. Other supplemental claims are forwarded automatically to the private insurer if the private insurer contracts with the carrier to send Medicare claim information electronically.
Can you submit paper claims electronically?
Even if you qualify to submit paper claims, consider submitting electronically.
Can Medicare cards be similar?
A: This can easily happen as the two Medicare cards are very similar. The doctor’s office should pay close attention to the specific details printed on your Railroad Medicare card.
Does Medicare cover injectable cancer drugs?
A: Only in limited instances will Medicare Part B provide for prescription drug coverage, such as for certain injectable cancer drugs or immunosuppressive drugs. All other Medicare benefits for prescription drugs require enrollment in a Part D Prescription Drug Program.
Does Medicare cover dental implants?
A: In most cases, Medicare does not cover dental services, specifically, services related to the care, treatment, filling, removal, or replacement of teeth, or structures directly supporting teeth. This would include check-ups, cleanings, and dental devices (such as dentures, dental plates, dental implants, or bridges) as well as extractions or other procedures performed to prepare the mouth for dentures (including reconstruction of the ridge) or titanium implants.
Does Medicare pay for hearing aids?
A: No, Medicare does not pay for hearing aids or hearing exams, when the purpose of the exam is to determine whether you need hearing aids or for fitting hearing aids.
When Do I Need to File A Claim?
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them an...