- Funding overview. There are two main sources of funding for Medicare Advantage. Advantage plans pay for the services otherwise covered by Medicare parts A and B.
- Bidding process. The Advantage plan bidding process involves two steps. First, each plan submits a bid to Medicare, based on the estimated cost of Part A and Part B benefits ...
- Base rate and risk adjustment rate. Medicare Advantage uses the bid and the benchmark to determine the base rate. ...
- Sources of Medicare funds. Two trust funds held by the United States Department of the Treasury supply the money for Medicare payments.
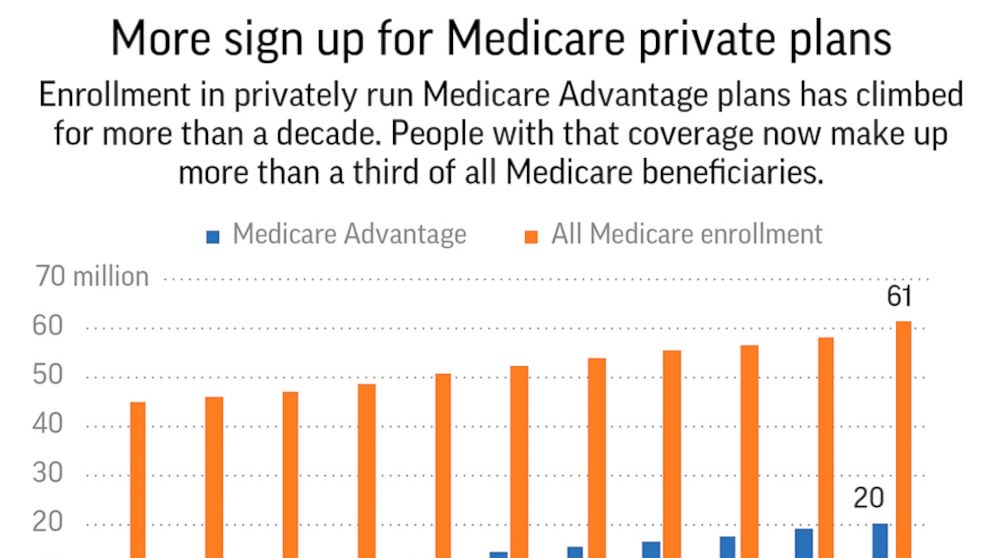
- Percentage of Medicare spending on Advantage plans. In 2019, Medicare payments to Advantage plans to fund Part A and Part B benefits were $250 billion, according to the Kaiser Family ...
- Summary. Medicare Advantage is funded from two main sources. The plans receive some funding through monthly plan premiums, but most of the money comes from Medicare.
Full Answer
How do insurance companies make money on Medicare Advantage?
How Medicare Advantage Plans Make Money (Video) CMS Pays Medicare Advantage Plans Medicare Advantage companies have a contract with the federal government. Medicare pays these private companies to take on the risk of its policyholders. So, instead of Medicare paying for your claims, they pay the insurance company to manage them.
What do you pay in a Medicare Advantage plan?
Sep 15, 2018 · In addition to the Part B premium, which you must continue to pay when you enroll in Medicare Advantage, some Medicare Advantage plans also charge a separate monthly premium. The insurance company uses this pool of money from the Medicare Trust Funds plus any additional premiums paid by plan members to pay the covered health care expenses for …
How much does Medicare pay Advantage plans?
How do Medicare Advantage plans make money? As you can see from other answers, the basic formula is straightforward enough: In return for agreeing to provide all Medicare benefits to your customers (“enrollees”) in your plan, the Medicare Advantage company gets a payment from CMS, the agency that runs Medicare and can also charge enrollees a supplementary premium.
Does Medicare Advantage save you money?
Medicare pays a fixed amount for your care each month to the companies offering Medicare Advantage Plans. These companies must follow rules set by Medicare. Each Medicare Advantage Plan can charge different out-of-pocket costs . They can also have different rules for how you get services, like: Whether you need a referral to see a specialist
See more
When you join a Medicare Advantage Plan, Medicare pays a fixed amount for your coverage each month to the company offering your Medicare Advantage Plan. Companies that offer Medicare Advantage plans must follow rules set by Medicare. However, each Medicare Advantage Plan can charge different out-of-pocket costs and
How do 0 premium Medicare Advantage plans make money?
Medicare Advantage plans are provided by private insurance companies. These companies are in business to make a profit. To offer $0 premium plans, they must make up their costs in other ways. They do this through the deductibles, copays and coinsurance.
What is the biggest disadvantage of Medicare Advantage?
The primary advantage is the monthly premium, which is generally lower than Medigap plans. The top disadvantages are that you must use provider networks and the copays can nickel and dime you to death.Dec 12, 2021
Is Medicare Advantage profitable for insurance companies?
In 2019, when the most recent data is available, private insurers averaged 4.5 percent profit margins on their Medicare Advantage plans. Between 2016 and 2018, Medicare Advantage plans reported nearly double the profit margins per customer compared to individual and employer plans.Oct 20, 2021
Why are Medicare Advantage plans so much cheaper?
A main reason why Medicare Advantage carriers can offer low to zero-dollar monthly premium plans is because Medicare pays the private companies offering the plans to take on your health risk.
Is Medicare Advantage more expensive than Medicare?
Abstract. The costs of providing benefits to enrollees in private Medicare Advantage (MA) plans are slightly less, on average, than what traditional Medicare spends per beneficiary in the same county.Jan 28, 2016
Can I drop my Medicare Advantage plan and go back to original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
How much money did Humana make last year?
Humana annual revenue for 2020 was $77.155B, a 18.9% increase from 2019. Humana annual revenue for 2019 was $64.888B, a 14.01% increase from 2018.
How much money do insurance companies make?
Insurers and Profit Margins Many insurance firms operate on margins as low as 2% to 3%. Smaller profit margins mean even the smallest changes in an insurance company's cost structure or pricing can mean drastic changes in the company's ability to generate profit and remain solvent.
How much profit do health care insurance companies make?
Big-name health insurers raked in $8.2 billion in profit for the fourth quarter of 2019 and $35.7 billion over the course of the year.
What is the highest rated Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
Can I switch from Medigap to Medicare Advantage?
Can you switch from Medicare Supplement (Medigap) to Medicare Advantage? Yes. There can be good reasons to consider switching your Medigap plan. Maybe you're paying too much for benefits you don't need, or your health needs have changed and now you need more benefits.Jun 24, 2021
What is the difference between AARP Medicare Complete and AARP Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) is an alternative way to get your benefits under Original Medicare (Part A and Part B). By law, Medicare Advantage plans must cover everything that is covered under Original Medicare, except for hospice care, which is still covered by Original Medicare Part A.
What does the trust fund pay for?
The money in this trust fund pays for Part A expenses such as inpatient hospital care, skilled nursing facility care, and hospice.
Does Medicare Advantage charge a monthly premium?
In addition to the Part B premium, which you must continue to pay when you enroll in Medicare Advantage, some Medicare Advantage plans also charge a separate monthly premium.
Does Medicare Advantage have a lower cost?
In return, however, Medicare Advantage plans tend to have lower out-of-pocket costs than Original Medicare, and unlike Original Medicare, Medicare Advantage plans also have annual limits on what you have to pay out-of-pocket before the plan covers all your costs.
Can I enroll in a zero premium Medicare Advantage plan?
You may be able to enroll in a zero-premium Medicare Advantage plan (although, remember, you still have to pay your regular Part B premium) and you may have other costs, such as copayments and coinsurance.
How does Medicare Advantage make money?
Medicare Advantage Plans make money in the same ways that other health insurance plans make money. They collect premiums, hold expenses down, invest, and pay claims. Insurance businesses work in similar overall fashion to individuals. You collect a paycheck, hold expenses down, save or invest, and pay your bills.
How much do Medicare Advantage plans get paid?
The Medicare Advantage plans/providers get paid (depending on region) $750 to $1,500 per month per beneficiary . If they pay less in claims than they take in from the Government, they make a profit. The MA companies make a LOT of profit on most beneficiaries and lose HUGE amounts on a small percentage of beneficiaries.
How much is Medicare Part A deductible?
Medicare Part A deductible is $1420/year and -0- after, Advantage plan is $250/day in hosp for 1st 5 or 7 days for each hospital stay). Under Part B, an Advantage plan has a copay for each visit to a Doctor or service, and you can’t buy a supplemental for a Medicare advantage plan.
What is MSA in Medicare?
MSA: Medicare Advantage Medical Savings Account is a High Deductible health insurance plan that deposit funds into an account used for paying your healthcare cost. SNP: Medicare Advantage Special needs Plans are specific to the needs of individuals with specific debilitating, usually chronic, conditions.
What is Medicare Advantage?
Medicare Advantage Plans usually put you in a network. Most Medicare Advantage Plans put you in a network of specialist and doctors. Usually, this might be a viable option for folks that do not have a dedicated doctor and live out their days in one place.
How much profit does Medicare Advantage make?
At the end of the year, if it does all these things successfully, the Medicare Advantage plan can make a profit (usually a percent or two of the premium, not 46%). If they mess it up (which is easy to do), they can lose millions. There are reasons why companies go to all this trouble. The cash flow is tremendous.
What is Medicare Part A and Part B?
Generally, when a person enrolls in Original Medicare, they get Medicare Part A, and Medicare Part B. But they are still responsible for 20% of the medical bill and prescription drugs. This is where Medicare Advantage, Medicare Supplement, and PDP plans plans come in. Medicare Advantage Plans are managed by Companies.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
Can't offer drug coverage?
Can’t offer drug coverage (like Medicare Medical Savings Account plans) Choose not to offer drug coverage (like some Private Fee-for-Service plans) You’ll be disenrolled from your Medicare Advantage Plan and returned to Original Medicare if both of these apply: You’re in a Medicare Advantage HMO or PPO.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
What is Medicare Advantage Plan?
A Medicare Advantage Plan is intended to be an all-in-one alternative to Original Medicare. These plans are offered by private insurance companies that contract with Medicare to provide Part A and Part B benefits, and sometimes Part D (prescriptions). Most plans cover benefits that Original Medicare doesn't offer, such as vision, hearing, ...
What is Medicare Part A?
Original Medicare. Original Medicare includes Part A (hospital insurance) and Part B (medical insurance). To help pay for things that aren't covered by Medicare, you can opt to buy supplemental insurance known as Medigap (or Medicare Supplement Insurance). These policies are offered by private insurers and cover things that Medicare doesn't, ...
What is the Cares Act?
On March 27, 2020, President Trump signed a $2 trillion coronavirus emergency stimulus package, called the CARES (Coronavirus Aid, Relief, and Economic Security) Act, into law. It expands Medicare's ability to cover treatment and services for those affected by COVID-19.
Can you sell a Medigap plan to a new beneficiary?
But as of Jan. 2, 2020, the two plans that cover deductibles—plans C and F— cannot be sold to new Medigap beneficiaries.
Do I have to sign up for Medicare if I am 65?
Coverage Choices for Medicare. If you're older than 65 (or turning 65 in the next three months) and not already getting benefits from Social Security, you have to sign up for Medicare Part A and Part B. It doesn't happen automatically.
Does Medicare cover vision?
Most plans cover benefits that Original Medicare doesn't offer, such as vision, hearing, and dental. You have to sign up for Medicare Part A and Part B before you can enroll in Medicare Advantage Plan.
Does Medicare automatically apply to Social Security?
It doesn't happen automatically. However, if you already get Social Security benefits, you'll get Medicare Part A and Part B automatically when you first become eligible (you don't need to sign up). 4. There are two main ways to get Medicare coverage: Original Medicare. A Medicare Advantage Plan.
How does Medicare pay?
Medicare pays the insurance company a fixed amount per enrollee per year to manage the care provided to the beneficiary who enrolled with the insurance company. These beneficiaries opt out of the traditional Medicare plan administered by the Government.
Is the denial rate for Medicare Advantage higher than traditional Medicare?
The denial rate on claims for these Medicare Advantage plans is much higher than traditional Medicare. This increases the cost to collect from these plans. As a practice you must be familiar to recognize this pool of patients and follow all the rules and regulations prior to rendering the service.
Is Medicare Advantage a private insurance?
Medicare Advantage Plans Are Lucrative for Insurance Companies. In an effort to control Medicare costs, the government few years ago introduced Medicare Advantage plans which are administered by private insurance companies. Medicare pays the insurance company a fixed amount per enrollee per year to manage the care provided to ...
Does Medicare Advantage require prior authorization?
Unlike, traditional Medicare which does not require prior authorization, Medicare Advantage plans operate like any managed care plan. This puts an extra burden on the practice to ensure all the rules imposed by such insurance company are followed prior to rendering care.
Is Medicare a cash cow?
These plans are aggressively marketed by insurance companies to Medicare beneficiaries. They have proven to be “cash cows” for the insurance industry. The insurance companies reimburse as per the Medicare rates, however to make them attractive to the average Medicare beneficiary they add extra benefits including health club memberships in some ...
How to choose a Medicare Advantage plan?
A no-premium Medicare Advantage plan might be a good idea for you if: 1 You’re healthy and are willing to take on the risk of a high deductible in exchange for low or no monthly premium. 2 You rarely go to the doctor and have enough money saved up to cover any very unexpected emergencies. 3 You’re dual eligible, meaning you’re eligible for both Medicare and Medicaid. 4 You don’t travel much and live in one state for the entire year.
What is Medicare Advantage?
In case you’re new to Medicare, Medicare Advantage is an alternative option for health coverage. Medicare Advantage, or MA, is offered by private insurance companies, and it’s approved by Medicare. MA plans cover everything traditional Medicare covers as well as emergency and urgent care. These plans often include extra perks, like dental coverage, ...
What is an HMO plan?
HMO Point-of-Service (HMO/POS) plans: HMO plans may allow you to get some services out-of-network for a higher copayment or coinsurance. Medical Savings Account (MSA) plans: These plans combine a high-deductible health plan with a bank account. Medicare deposits money into the account (usually less than the deductible).
How much does Medicare Part B cost?
As of 2018, that premium is $134 per month, and it generally comes right out of your social security check.
What is the maximum out of pocket limit for Medicare Advantage?
Some of the tradeoffs of Medicare Advantage when comparing it to Original Medicare are the networks and the co-pays, which accumulate to a maximum out-of-pocket limit anywhere between a couple thousand dollars to as high as $6,000 ...
How many types of Medicare Advantage are there?
When we talk about Medicare Advantage, we often refer to these plans as a single entity, but in reality, there are actually 6 different types of MA plans. Health Maintenance Organization (HMO) plans: In most HMOs, you can only go to doctors in your network (except in an urgent or emergency situation). Preferred Provider Organization (PPO) ...
Can MSAs be used for Medicare?
Medicare deposits money into the account (usually less than the deductible). You can use the money to pay for your health care services during the year. MSA plans don’t offer Medicare drug coverage. If you want drug coverage, you have to join a Medicare Prescription Drug Plan. The last one – Medical Savings Accounts (MSAs) – are another type ...