They’re a special kind of Medicare Advantage Plan where enrollees use the same healthcare provider for both Medicare and AHCCCS
Arizona Health Care Cost Containment System
The Arizona Health Care Cost Containment System is the name of the Medicaid program in the state of Arizona. As with all Medicaid programs, it is a joint program between the state and the Centers for Medicare and Medicaid Services. It became the final such state Medicaid program to implemented under Title XIX when it began in October 1982 as a section 1115 demonstration project. The progra…
Full Answer
How do Medicare benefits and Medicaid work together?
How Do Medicare Benefits and Medicaid Work Together? The Centers for Medicare & Medicaid Services (CMS) manages the social health programs called Medicare and Medicaid. These programs are specially designed to help disabled, senior, and low-income people afford health coverage.
What is an AHCCCS Medicare Advantage plan?
They’re a special kind of Medicare Advantage Planwhere enrollees use the same healthcare provider for both Medicare and AHCCCS. The healthcare provider will then assume the burden of making the proper insurance claims to the two programs while monitoring each individual’s overall health maintenance program.
What are Medicare and Medicaid?
The Centers for Medicare & Medicaid Services (CMS) manages the social health programs called Medicare and Medicaid. These programs are specially designed to help disabled, senior, and low-income people afford health coverage. These two health insurances cover two different population sectors.
What is AHCCCS (health care cost containment system)?
The Arizona program has been called the Arizona Health Care Cost Containment System (or AHCCCS) since its inception. A key element of the AHCCCS program can be understood from its name: Arizona’s approach has focused on containing the cost of Medicaid at least as much as on providing complete or quality care.
How does AHCCCS work with Medicare?
With AHCCCS Freedom to Work benefits, you will only have to pay a small $2.30 copayment for most prescription drugs. Note: If you are eligible for Medicare, your AHCCCS Freedom to Work will probably cover your Medicare Part D premium and any deductibles in your Part D plan.
Can I have AHCCCS and Medicare?
AHCCCS Members who also have Medicare are called Dual Eligible Members. Being enrolled in the same health plan for Medicare and Medicaid is called “alignment.” Alignment provides: • One plan that coordinates all care. A comprehensive provider network.
Does AHCCCS cover Medicare premiums?
AHCCCS QMB – ONLY is Medicare Savings Program that pays Medicare Part A premium (when applicable) and Medicare Part B premium. Claim payments are limited to Medicare deductible, coinsurance, and copay when Medicare pays first.
Is Arizona AHCCCS Medicaid or Medicare?
MedicaidProvider Enrollment Services Available Online Arizona Health Care Cost Containment System (AHCCCS) is Arizona's Medicaid agency that offers health care programs to serve Arizona residents. Individuals must meet certain income and other requirements to obtain services.
Does AHCCCS cover Medicare Part B?
AHCCCS SLMB-PART B BUY-IN is strictly a Medicare Savings Program that pays Medicare Part B premium. No claim payments are done by AHCCCS Administration. For questions regarding Medicare coverage, call 1-800-MEDICARE.
Do you have to pay for Medicare in Arizona?
Original Medicare costs (Part A and B) in Arizona are the same nationwide. The Medicare Part A premium can cost you $0, $274, or $499, depending on how long you or your spouse worked and paid Medicare taxes. For Part A hospital inpatient deductibles and coinsurance, you pay: $1,556 deductible for each benefit period.
Does Social Security count as income for AHCCCS?
Social security benefits are counted for all MA programs as unearned income. Ongoing benefits are paid monthly.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
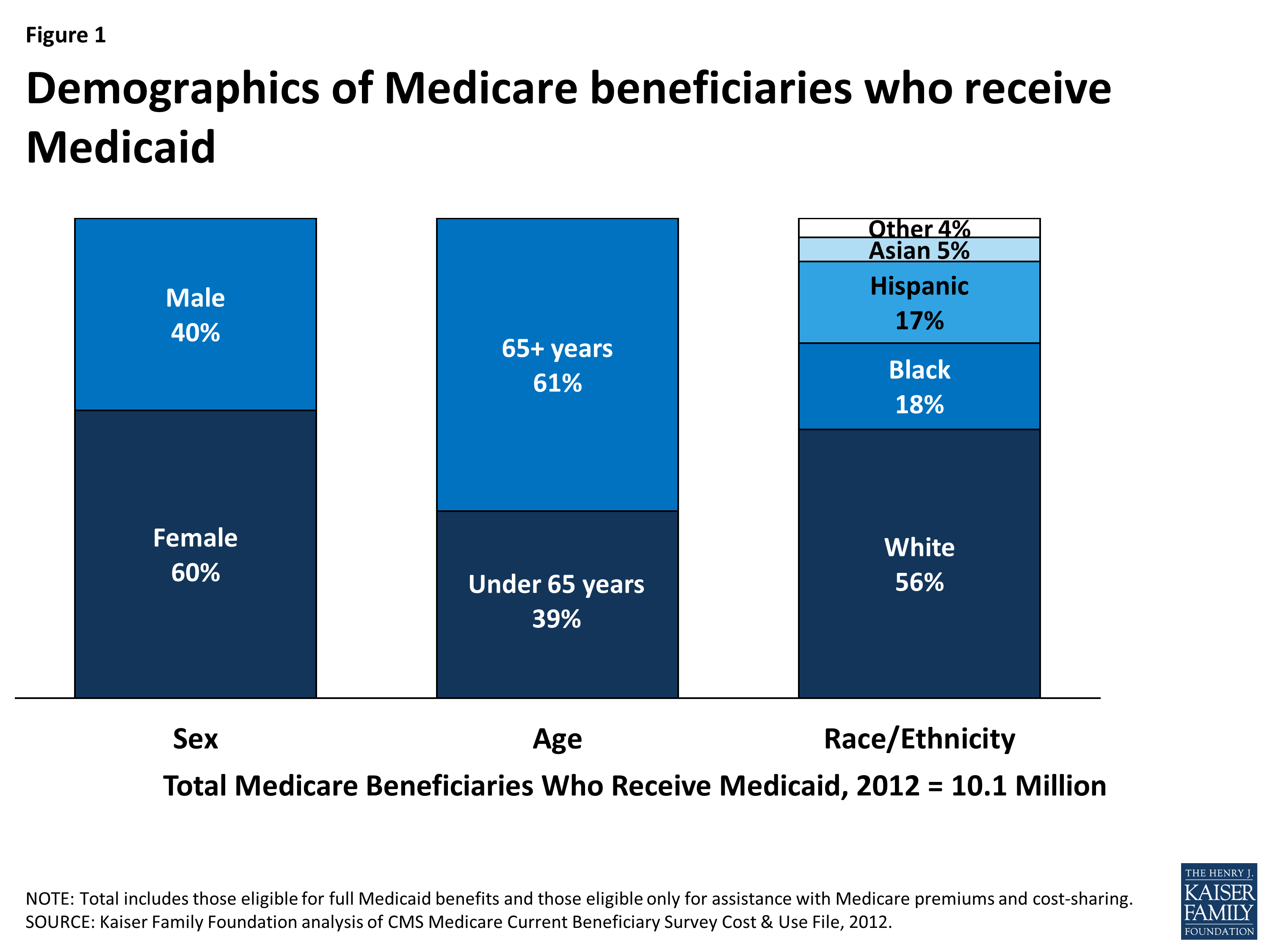
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
What is Medicare in Arizona called?
The Arizona Health Care Cost Containment System (AHCCCS) is Arizona's Medicaid agency, and Medicaid within the state is often referred to as “AHCCCS.” Although the agency provides the medical insurance coverage, DES determines the eligibility for Medicaid.
How much does Medicare cost in Arizona?
Medicare in Arizona by the NumbersPeople enrolled in Original MedicareAverage plan costAnnual state spending per beneficiary781,211Plan A: $0 to $499 per month* Plan B: $170.10 per month**$9,201
Does Arizona have Medicare?
Summary: Medicare in Arizona provides health care coverage to residents 65 years and older and people with some disabilities. Currently, there are over one million Medicare beneficiaries in this popular retirement state. Choices in Medicare allow beneficiaries to find the right plan for their needs and budget.
Citizenship And Noncitizen Requirements
You must be a U.S. citizen or meet specific noncitizen requirements to be eligible for AHCCCS Freedom to Work.
Ahcccs Freedom To Work Program
When you have a job and your income is more than regular AHCCCS allows, you may be eligible for the AHCCCS Freedom to Work Program. The AHCCCS Freedom to Work Program covers the same services that standard AHCCCS covers, including visits to the doctor, hospital stays, medical equipment, home care services, and mental health services.
Weve Got You Covered So You Can Do Life
Health Choice Pathway is a Health Plan with a Medicare contract and a contract with the state Medicaid program. Enrollment in Health Choice Pathway depends on contract renewal. Health Choice Pathway is an affiliate of Blue Cross® Blue Shield® of Arizona.
Ahcccs Freedom To Work And Medicare
If you are eligible for both AHCCCS Freedom to Work and Medicare, it will help you to have both because:
Does Medicaid Cover Dental In Arizona
Arizona Medicaid Dental coverage for Adults Arizona adults who are enrolled in MediCaid Access receive emergency dental care. Medicaid in Arizona does not cover exams, x-rays, cleanings or other preventive dentistry . For complete coverage details, visit the Arizona Healthcare Cost Containment System site.
Medicare And Medicaid Benefits Advice Az
Our licensed agents in the state of Arizona can give you professional advice and help you sort through your options and find the best AHCCCS health plan for your needs. We actually have a corporate office in Tucson, so we are very familiar with Arizona Medicare plans and have lots of agents eager to help you.
How Do I Submit A Claim Availity
How do I send claims to Availity ? Create a claim file using your current billing software. Click EDI File Management/Send and Receive EDI Files. Click the Send Files mailbox. Browse your computer for the batch claim file and click on it. Click Upload File Availity sends the claims to the appropriate payers.
What is specialized Medicare?
Enrolling in specialized Medicare plans allows dual eligible members to receive all of their health care services, including prescription drug benefits, from a single, integrated health plan.
What is dual eligible member?
AHCCCS continues developing integration initiatives to increase alignment and improve service delivery for individuals covered by both Medicare and Medicaid. These individuals, commonly referred to as “dual eligible members,” navigate multiple health systems to receive care. This health system fragmentation often results in poor communication, uncoordinated health care decisions and a lack of a patient-centered perspective. AHCCCS has moved toward increasing the coordination of health service delivery between these two health programs by contracting with Medicare Advantage Dual Special Needs Plans (D-SNPs) that are each affiliated with its partner AHCCCS Complete Care (ACC) Medicaid health plan. Requiring each ACC Medicaid health plan to offer a partner Medicare D-SNP promotes the enrollment or alignment of dual eligible members in the same health plan for both Medicare and Medicaid services to the greatest possible extent. Enrolling in specialized Medicare plans allows dual eligible members to receive all of their health care services, including prescription drug benefits, from a single, integrated health plan.
Ahcccs Medicaid Program Is Available For Low Income Individuals And Familys
The income limit in Arizona is less than $1,067 for an individuals or $1,437 for a couple per month.
Medicaid For Disabled And Elderly Residents
ALTCS is a state Medicaid program that can help certain individuals afford their medical care. This system provides specifically for the long-term medical needs of qualifying disabled, blind, or aged residents in the state. This program pays for the services you require once youve already exhausted your savings.
How We Can Help
If you are new to Medicare this is a stressful part of life to deal with. Our agents know the exact process on helping you find the right Medicare plan.
Current News Bulletins And Alerts
To avoid a claim denial, ensure youre using the correct place of service code when providing telehealth services for UnitedHealthcare Community Plan members.
How To Report Fraud Waste Or Abuse To The State Of Arizona
The Office of Inspector General for the State of Arizona provides a way for members, plans, providers, and the public to report all forms of suspected fraud, waste or abuse of the program. We encourage medical professionals and their staff to review the information available on the AHCCCS website.
How Much Can You Make And Keep Ahcccs
In the 1619 program, people on SSI can work and keep AHCCCS, even if they earn too much money to qualify for SSI cash benefits. The premiums for this program will not be required if you are on it. Those who live in Arizona and are on SSI and AHCCCS can have up to $41,015 in gross income and remain on AHCCCS even if they lose their SSI benefits.
Who Can Receive Services
AHCCCS offers medical programs and resources to serve Arizona residents who meet certain income and other requirements.
What is the difference between Medicare and Medicaid?
When you have dual enrollment, Medicare is your primary insurance that covers any costs first. Medicaid is your secondary payer. Every state has different benefits for people who qualify under dual eligibility, so it’s important that you check with your local Medicaid office.
Does Medicaid cover dental care?
Medicaid can cover a large variety of healthcare services like behavioral health for substance abuse and mental health or dental care. Medicaid also has a robust cost-sharing program that helps cover any out of pocket costs for economically disadvantaged participants.
Can seniors get medicaid?
Many seniors in the United States have dual eligibility for Medicare and Medicaid benefits. Generally, this means that you have enrolled in Medicare, but that you qualify for Medicaid as well due to your income.
Is Medicaid a secondary insurance?
Secondary Insurance. Medicaid can fill in the gap as a secondary insurance to Medicare. Any services you have that Medicare pays for like hospital care, doctor’s visits, skilled nursing facility care, or home care, Medicare will pay for as the primary payer.
Can you have both Medicare and Medicaid?
What happens if you’re someone who meets the criteria for both? Millions of individuals live on a fixed income, and this can qualify you for Medicaid coverage. Can you have both Medicare and Medicaid coverage, or do you have to choose one? If you qualify, you may be able to be a dual-eligible.
Does Medicaid pay cost sharing?
Medicaid can pay any cost-sharing charges you have. This help will depend on your income level. If the level is low enough, you could qualify for the Qualified Medicare Beneficiary (QMB) Medicare Savings Program. If you enroll in QMB, you won’t have to pay Medicare cost-sharing fees.
Does Medicare help with prescription drugs?
Prescription drugs are some of the biggest expenses people on Medicare face, and Medicaid can help. People who meet the eligibility requirements for dual enrollment in Medicare and Medicaid automatically get enrolled in the Extra Help program.
What is integrated care?
When care is provided to Medicare-Medicaid beneficiaries through an “integrated” care model, the beneficiary can get the full array of Medicaid and Medicare benefits through a single delivery system. This approach can improve care coordination and quality, and reduce administrative burdens. One such model is the Program for All-Inclusive Care ...
How many states are there in the Pace program?
PACE provides comprehensive medical and social services to certain frail elderly individuals enabling them to continue living in the community. There are currently 113 PACE programs operating in 32 states. In Spanish,“bien vivir” means “good life” or “to live a good life.”.
Does Medicare cover out of pocket medical expenses?
Medicare beneficiaries who have limited income and resources may get help paying for their Medicare premiums and out-of-pocket medical expenses from Medicaid. Medicaid also covers some important services not provided under Medicare, such as community-based long-term services and supports, nursing facility care (for stays beyond 100 days), ...
What age does AHCCCS cover?
AHCCCS typically covers state residents who are younger than 65
Why are some people denied AHCCCS?
Many residents are denied ALTCS benefits because they have too many resources to meet the eligibility requirements. Fortunately, this doesn’t mean that you can’t qualify later once you do.
What is the Medicaid program in Arizona?
The Medicaid program in Arizona is called AHCCCS (the Arizona Health Care Cost Containment System). AHCCCS is jointly federal and state funded and helps to support low-income individuals who are younger than 65 (though some who are older might be eligible).
How old do you have to be to qualify for AHCCCS?
To qualify for AHCCCS, you usually must be younger than 65 (though you can be 65 or older if you’re the caretaker or parent of a child). You must be either on Medicare as a pregnant woman or caretaker/parent of a child or be ineligible for Medicare services.
What to do if you don't meet the financial requirements for ALTCS?
If you don’t meet the financial requirements for ALTCS, a lawyer might be able to help
Can you get ALTCS if your income is higher than your income?
If your income is higher than these numbers, don’t let that deter you from pursuing ALTCS services. You might still be able to qualify for benefits by using a Miller Trust. Like other trusts, this type of trust must be legally sound in order to be considered valid.
Does income count as AHCCCS?
or a qualified noncitizen. Income-based AHCCCS will count most of the unearned and earned income you have. Some income doesn’t count, though , such as Supplemental Security Income.
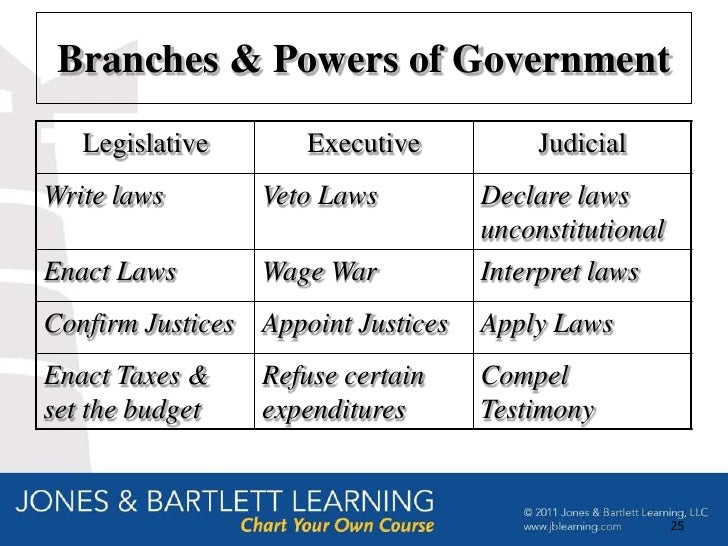
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.