Medicare calculates the penalty by multiplying 1% of the "national base beneficiary premium" ($33.37 in 2022) times the number of full, uncovered months you didn't have Part D or creditable coverage. The monthly premium is rounded to the nearest $.10 and added to your monthly Part D premium.
How can I avoid paying the Medicare Part D penalty?
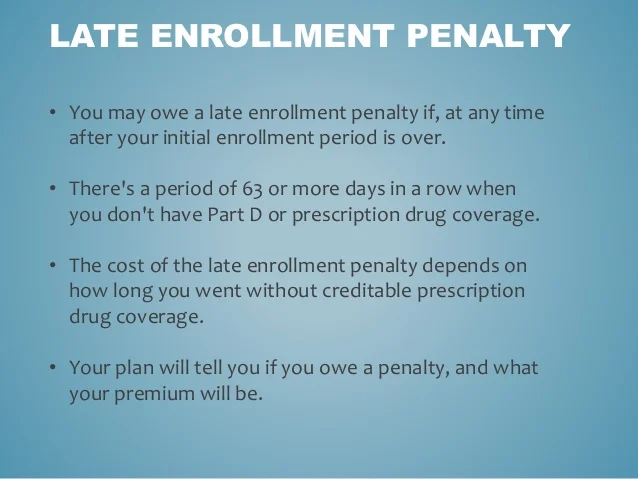
that may be added to a person’s monthly premium for Medicare drug coverage (Part D). A person enrolled in a Medicare plan may owe a late enrollment penalty if they go without Part D or other creditable prescription drug coverage for any continuous period of 63 days or more after the end of their Initial Enrollment Period for Part D coverage.
What are the rules of Medicare Part D?
May 27, 2021 · Here is an example of a common Part D penalty. Let’s suppose you started shopping and purchased your Medicare Part D Prescription Drug Plan in 2021, nine months after your Initial Enrollment Period (IEP) ended. One percent of the “national base beneficiary premium of $33.06 is $0.33 which will be multiplied by 9 months. $0.33 x 9 = $2.97
Is it mandatory to have Medicare Part D?
Dec 13, 2019 · To eliminate the companies’ fear healthy individuals on Medicare (CMS) might not participate in the drug program, a penalty for non-enrollment is included if they don’t join Part D or enroll in an advantage plan by the deadline, if they don’t qualify for an exemption.
How do you calculate Medicare penalty?
Multiply $0.3337 by the number of months you are late enrolling ($0.3337 X 10) 2022 Part D penalty = $3.34/mo → rounded to the nearest ten cents → $3.30/mo. The penalty is assessed monthly…and for life! The constant factor will be that you were 10 months late in this example, but what will change is the Part D national base premium.
How do I avoid late enrollment penalty for Part D?
3 ways to avoid the Part D late enrollment penaltyEnroll in Medicare drug coverage when you're first eligible. ... Enroll in Medicare drug coverage if you lose other creditable coverage. ... Keep records showing when you had other creditable drug coverage, and tell your plan when they ask about it.
How do you explain late enrollment penalty?
The late enrollment penalty amount typically is 1% of the “national base beneficiary premium” (also called the base beneficiary premium) for each full, uncovered month that the person didn't have Medicare drug coverage or other creditable coverage. The national base beneficiary premium for 2022 will be $33.37.
How long is a member responsible for a late enrollment penalty?
For most people, you have to pay the LEP as long as you are enrolled in the Medicare prescription drug benefit. There are some exceptions: If you receive Extra Help, your penalty will be permanently erased. If you are under 65 and have Medicare, your LEP will end when you turn 65.
Does Part D penalty go away when you turn 65?
In most cases, you will have to pay that penalty every month for as long as you have Medicare. If you are enrolled in Medicare because of a disability and currently pay a premium penalty, once you turn 65 you will no longer have to pay the penalty.
How do I appeal a Part D Penalty?
Part D Late Enrollment Penalty Reconsideration Request Form An enrollee may use the form, “Part D LEP Reconsideration Request Form C2C” to request an appeal of a Late Enrollment Penalty decision. The enrollee must complete the form, sign it, and send it to the Independent Review Entity (IRE) as instructed in the form.Dec 1, 2021
When did Part D become mandatory?
Medicare Part D Prescription Drug benefit Under the MMA, private health plans approved by Medicare became known as Medicare Advantage Plans. These plans are sometimes called "Part C" or "MA Plans.” The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.Dec 1, 2021
When did Medicare Part D become mandatory?
January 1, 2006In 2003 the Medicare Modernization Act created a drug benefit for seniors called Part D. The benefit went into effect on January 1, 2006.Aug 10, 2017
Is Medicare Part D required by law?
Is Medicare Part D Mandatory? It is not mandatory to enroll into a Medicare Part D Prescription Drug Plan.
How are Part D premiums determined?
The income that counts is the adjusted gross income you reported plus other forms of tax-exempt income. Your additional premium is a percentage of the national base beneficiary premium $33.37 in 2022. If you are expected to pay IRMAA, SSA will notify you that you have a higher Part D premium.
Do I need Medicare Part D if I don't take any drugs?
If you don't take any medications at all, you'll still want to enroll in Part D when you're first eligible (unless you have other creditable drug coverage), to avoid the late enrollment penalty described above.
Can I opt out of Medicare Part D?
To disenroll from a Medicare drug plan during Open Enrollment, you can do one of these: Call us at 1-800 MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Mail or fax a signed written notice to the plan telling them you want to disenroll.
What happens if I don't want Medicare Part D?
If you don't sign up for a Part D plan when you are first eligible to do so, and you decide later you want to sign up, you will be required to pay a late enrollment penalty equal to 1% of the national average premium amount for every month you didn't have coverage as good as the standard Part D benefit.
Is Mrs Martinez on Medicare?
Mrs. Martinez is currently eligible for Medicare, and her Initial Enrollment Period ended on May 31, 2016. She doesn’t have prescription drug coverage from any other source. She didn’t join by May 31, 2016, and instead joined during the Open Enrollment Period that ended December 7, 2018. Her drug coverage was effective January 1, 2019
Does Mrs Kim have Medicare?
Mrs. Kim didn’t join a Medicare drug plan before her Initial Enrollment Period ended in July 2017. In October 2017, she enrolled in a Medicare drug plan (effective January 1, 2018). She qualified for Extra Help, so she wasn’t charged a late enrollment penalty for the uncovered months in 2017. However, Mrs. Kim disenrolled from her Medicare drug plan effective June 30, 2018. She later joined another Medicare drug plan in October 2019 during the Open Enrollment Period, and her coverage with the new plan was effective January 1, 2020. She didn’t qualify for Extra Help when she enrolled in October 2019. Since leaving her first Medicare drug plan in June 2018 and joining the new Medicare drug plan in October 2019, she didn’t have other creditable coverage. However, she was still deemed eligible for Extra Help through December 2018. When Medicare determines her late enrollment penalty, Medicare doesn’t count:
Medicare Part D Penalty: What is it?
The Medicare Part D late enrollment penalty (also referred as “LEP”) is a specific dollar amount that is added to your Part D monthly premium. If you have enrolled in a Medicare Part D drug plan, you may be responsible to pay an enrollment penalty. This is typically added to your monthly Part D premium.
How the Penalty works
The late enrollment Part D penalty will generally happen for you if the following occurs:
How much are the part d penalties?
How much will you pay for your Part D penalty? The cost will depend on how long you were without a Part D plan (or creditable drug coverage).
What happens if you don't have a prescription drug?
If you didn’t have creditable prescription drug coverage and didn’t enroll in a Part D plan during your Initial Enrollment Period in Medicare, you will owe a lifetime penalty (except those on Medicaid or currently approved for the Extra Help program).
Can you get late enrollment for Part D?
However, that doesn’t mean you won’t receive a late enrollment notice when you finally do enroll in Part D prescription drug coverage.
What happens if you don't enroll in a prescription drug plan?
If you fail to enroll in a Prescription Drug Plan during your Initial Enrollment Period (IEP) AND you do not have creditable drug coverage, you may have to pay a late penalty. Creditable drug coverage is any plan expected to pay at least as much toward your costs as a Medicare Prescription Drug plan. Common examples are the health plans you have ...
How much is Part D premium?
And again, the amount changes yearly, because the base beneficiary premium changes yearly. It’s scheduled to decrease in 2019, to $33.19.
Does Medicare have late penalties?
In an effort to incentivize beneficiaries to enroll in the program as soon as they become eligible, Medicare levies late penalties against those who fail to do so. The amount of the penalty varies according to whether you were late enrolling in Part A, B, or D (or any combination of the three). Those penalties can add up quickly, especially ...
How long do you have to enroll in Medicare?
The first, of course, is to join a Medicare drug plan as soon as you are eligible. Your Initial Enrollment Period consists of the three months before the month you turn 65, the month of your 65th birthday, and the three months following your 65th birthday. The next way to avoid the penalty is to not go 63 days or more without creditable drug ...
Does Medicare send a letter to the drug plan?
The Medicare contractor sends both you and your drug plan a letter detailing its decision. It may decide the late penalty should be removed entirely, that the amount of the penalty is wrong, or that the penalty is entirely correct. Your drug plan will make the appropriate changes to your premium, sending you a letter detailing the changes and whether you’ll see a refund.
How long does Medicare Part D last?
As long as you have creditable drug coverage, you qualify for an SEP once that coverage ends. The Special Enrollment Period lasts a full eight months for Medicare Parts A and B, but only 63 days for Part D. If you allow more than 63 days to pass, you’ll likely have a late penalty. Finally, you can avoid the Part D penalty if you save ...
How long does it take for Medicare to reconsider?
You have 60 days to complete and return the reconsideration form. The clock starts ticking on the date of the correspondence that informed you of your late penalty. Medicare’s contractor typically makes it decision within 90 days. While waiting, you must pay the late penalty, as it is considered part of your monthly premium.
Why do you need a Medicare Part D plan?
Selecting a Medicare Part D plan tailored to your patients’ needs is a great opportunity to confirm they are receiving ideal benefits with the lowest out-of-pocket costs . Additionally, helping them enroll in ...
What is creditable coverage?
Creditable coverage is coverage -- often through an employer or union -- which meets Medicare’s minimum standards, since this coverage is expected to pay at least as much as Medicare’s standard Part D coverage would .
How long do you have to enroll in Part D?
The first is based off of the initial eligibility period for Part D coverage. If the patient’s birthday is in February, they have 3 months after that (until May 31st) to en roll in a Part D plan.
What happens if you disenroll from a health insurance plan?
If they are considering disenrolling from a plan, they will want to make sure they'll still be receiving the coverage they need, as they will be giving up benefits like the network of providers who participate in that plan, and cap on your out-of-pocket spending for medical bills.
How long does it take for Medicare to reconsider?
The resolution of the decisions is typically made in about 90 days, but patients can expect to wait a little longer due to the large number of requests being filed.
What is Medicare Part D?
Medicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs.
When did Medicare Part D go into effect?
Part D was enacted as part of the Medicare Modernization Act of 2003 and went into effect on January 1, 2006. Under the program, drug benefits are provided by private insurance plans that receive premiums from both enrollees and the government.
Do Part D plans have to pay for all covered drugs?
Part D plans are not required to pay for all covered Part D drugs. They establish their own formularies, or list of covered drugs for which they will make payment, as long as the formulary and benefit structure are not found by CMS to discourage enrollment by certain Medicare beneficiaries. Part D plans that follow the formulary classes and categories established by the United States Pharmacopoeia will pass the first discrimination test. Plans can change the drugs on their formulary during the course of the year with 60 days' notice to affected parties.
What is a Part D benefit?
Beneficiary cost sharing. Part D includes a statutorily-defined "standard benefit" that is updated on an annual basis. All Part D sponsors must offer a plan that follows the standard benefit. The standard benefit is defined in terms of the benefit structure and without mandating the drugs that must be covered.
What is excluded from Part D?
Excluded drugs. While CMS does not have an established formulary, Part D drug coverage excludes drugs not approved by the Food and Drug Administration, those prescribed for off-label use, drugs not available by prescription for purchase in the United States, and drugs for which payments would be available under Part B.
What is part D coverage?
Part D coverage excludes drugs or classes of drugs that may be excluded from Medicaid coverage. These may include: Drugs used for anorexia, weight loss, or weight gain. Drugs used to promote fertility. Drugs used for erectile dysfunction. Drugs used for cosmetic purposes (hair growth, etc.)
What is Medicare Part D cost utilization?
Medicare Part D Cost Utilization Measures refer to limitations placed on medications covered in a specific insurer's formulary for a plan. Cost utilization consists of techniques that attempt to reduce insurer costs. The three main cost utilization measures are quantity limits, prior authorization and step therapy.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.