There are three main methods that Medicare supplement plan companies use to set their rates. These are community-rated (no age-rated), issue-age-rated (initial age-rated), and attained-age-rated. Even when companies use the same rating method, the actual premiums will likely vary widely between the companies.
How do insurers determine Medicare supplement premiums?
Insurance companies use two types of ratings systems to determine how they will charge premiums of Medicare Supplement plans: Community Rating: This type of rating system does not allow the insurance company to use health status or claims experience to set rates for plans. In these rating systems, everyone in the community pays the same rate.
How will my Medicare supplement insurance plan rates increase?
There are three different pricing models that insurance companies can use to determine how your Medicare Supplement Insurance plan rates may increase in the future. Each type of pricing system can produce a different rate for current and incoming plan members. Community-rated plans charge the same rate for every plan member, regardless of age.
Are Medigap rates different for Medicare supplement plans?
However, Medigap, or Medicare Supplement plans, have rates that are different as they are offered by authorized private insurance companies and have different coverages available. What is a Medicare Supplement Plan?
Are Medicare supplement plans standardized?
Before we dive in, it’s important to remember that Medicare Supplement plans are standardized. So, regardless of the company that you purchase your plan from or how much you pay for it, the benefits of the plan letter will be the same. How Do Companies Set Prices for Medicare Supplements?

How are Medigap premiums determined?
The premium is based on the age you are when you buy (when you're "issued") the Medigap policy. Premiums are lower for people who buy at a younger age and won't change as you get older. Premiums may go up because of inflation and other factors, but not because of your age.
Do Medicare Supplement premiums increase every year?
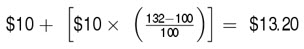
Medicare supplement rate increases usually average somewhere between 3% and 10% per year. And sometimes Medicare supplement rate increases even happen twice in the same year! Years of costly rate increases can be an economic hardship, to say the least.
Do all Medicare Supplement plans pay the same?
Medicare Supplement insurance plans are sold by private insurance companies and can help you pay for out-of-pocket costs for services covered under Original Medicare. Different Medicare Supplement insurance plans pay for different amounts of those costs, such as copayments, coinsurance, and deductibles.
Who has the cheapest Medicare supplement insurance?
What's the least expensive Medicare Supplement plan? Plan K is the cheapest Medigap plan, with an average cost of $77 per month for 2022.
Does Medicare Supplement cost increase with age?
Medicare Supplement Insurance premiums tend to increase with age.
What is the downside to Medigap plans?
Some disadvantages of Medigap plans include: Higher monthly premiums. Having to navigate the different types of plans. No prescription coverage (which you can purchase through Plan D)
What is the average cost of AARP Medicare supplement insurance?
1. AARP Medigap costs in states where age doesn't affect the pricePlan nameAverage monthly cost for AARP MedigapPlan A$158Plan B$242Plan C$288Plan F$2566 more rows•Jan 24, 2022
Which Medigap covers the most?
Policies C and F are the most comprehensive, but they generally cost more. See the Medigap Plan Benefits Chart for a fuller explanation of what each policy covers. Please note that this information is only applicable to plans sold beginning June 1, 2010.
What is the average cost of Medicare Supplement plans?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization. Several factors impact Medigap costs, including your age and where you live.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
Who is the largest Medicare Supplement provider?
UnitedHealthcareAARP's Medicare Supplement Insurance plans are insured exclusively by UnitedHealthcare, which is the largest provider of Medicare Supplement Insurance. AARP/UnitedHealthcare Medigap plans have low complaint rates when compared to most competitors.
How much do Medigap plans increase each year?
between 2% to 6% annuallyThe average Medicare Supplement Plan G rate increase is between 2% to 6% annually. Remember, this percentage can be higher or lower based on your carrier. It is important to understand the rate increase history for the carrier with which you choose to enroll.
When is the best time to buy Medicare Supplement?
The best time to purchase a Medicare Supplement is during your Medicare Supplement Open Enrollment Period, which starts the first six months that you are enrolled in Medicare Part B and are 65 or older. During this period, you have the right to join any Medicare Supplement plan, regardless of pre-existing conditions or disabilities.
Why do insurance companies charge more for quarterly payments?
Some companies will charge more for quarterly, semi-annual, and annual payments, because they prefer that you pay monthly. Furthermore, it is easier and more cost-effective for insurance companies to process payments paid electronically, rather than by check or credit card.
What is community rated Medicare?
There are three methods that a company can use to set rates for their Medicare Supplement policies: • Community-rated: With this pricing policy, every member, regardless of age, pays the same price. Hence, the name “Community.”. • Issue-age-rated: Your age is used for pricing, and is locked in on your policy start date.
Do women get lower Medicare?
Some insurance companies offer lower rates on Medicare Supplement plans for women. According to research, women typically live longer, which means they pay more for their coverage over their lifetime. Women also tend to enjoy better health and thus claim less.
What is the average Medicare Supplement Insurance rate?
The average rate for Medicare Supplement Insurance (Medigap) Plan F in 2019 was $169 per month. 1 So what does this mean for Medicare beneficiaries who are interested in finding a Medigap plan? While Medigap plan benefits are standardized in most states (which means that – for example – Medicare Plan F in North Carolina offers ...
How many different pricing models are there for Medicare Supplement?
There are three different pricing models that insurance companies can use to determine how your Medicare Supplement Insurance plan rates may increase in the future. Each type of pricing system can produce a different rate for current and incoming plan members. Community-rated plans charge the same rate for every plan member, regardless of age.
How long does it take to enroll in Medigap?
Your Medigap Open Enrollment Period starts as soon as you are at least 65 years old and enrolled in Medicare Part B. During the six months of your Medigap OEP, insurance companies cannot deny you a Medigap plan or charge you higher plan premiums based on your health.
How much is Medigap Plan G in New York?
In 2018, the average monthly premium rate of Medigap Plan G in New York was $304 per month. In the same year, the average monthly cost of Medigap Plan G in Iowa was only $102. 1. The difference in Medigap rates from one state to another can vary widely, similar to how the cost of a gallon of gas can differ greatly from one state to another.
What is community rated health insurance?
Community-rated plans charge the same rate for every plan member, regardless of age. For example, a 75-year-old Medigap beneficiary with a community-rated plan will pay the same rate as a 65-year-old beneficiary with the same plan. Issue-age-rated plans have rates based on the age at which you purchased the plan.
Does Medicare vary based on carrier?
Medigap rates can vary based on carrier. Original Medicare (Part A and Part B) premiums are standardized by the federal government. Private insurance companies that offer Medicare Supplement Insurance plans, however, are free to set their own rates. How a carrier rates (prices) its plans, inflation and other factors can cause premiums ...
Does Medigap go up as you get older?
As you get older, your Medigap rate will gradually go up . Some insurance companies may offer Medigap plan discounts for women, non-smokers, married couples, those who pay their premium for the entire year and more. Be sure to ask your plan provider if they offer any discounts before you sign up for a Medigap plan.
How much can Medicare increase from current budget?
By Federal statute, the Medicare annual budget request cannot increase more than $20 million from the current budget.
How much does Medicare pay for medical services?
The Medicare reimbursement rates for traditional medical procedures and services are mostly established at 80 percent of the cost for services provided. Some medical providers are reimbursed at different rates. Clinical nurse specialists are paid 85 percent for most of their billed services and clinical social workers are paid 75 percent ...
How many specialists are on the Medicare committee?
Medicare establishes the reimbursement rates based on recommendations from a select committee of 52 specialists. The committee is composed of 29 medical professionals and 23 others nominated by professional societies.
Why use established rates for health care reimbursements?
Using established rates for health care reimbursements enables the Medicare insurance program to plan and project for their annual budget. The intent is to inform health care providers what payments they will receive for their Medicare patients.
What is the original objective of Medicare?
The original objective was to establish a uniform payment system to minimize disparities between varying usual, customary, and reasonable costs. Today, Medicare enrollees who use the services of participating health care professionals will be responsible for the portion of a billing claim not paid by Medicare.
Who needs to be a participant in Medicare?
To receive reimbursement payments at the current rates established by Medicare, health care professionals and service companies need to be participants in the Medicare program.
Does Medicare accept all recommendations?
While Medicare is not obligated to accept all of the recommendations, it has routinely approved more than 90 percent of the recommendations. The process is composed of a number of variables and has been known for lack of transparency by the medical community that must comply with the rates.
How long does Medicare Supplement open enrollment last?
This timeframe may only happen once in your lifetime. Your Medicare Supplement Open Enrollment Period takes place during the six-month window that begins the first day of the month of your Part B effective date.
How to find Medigap premiums?
Because of this, Medigap premiums are unique for each beneficiary. When trying to find Medigap premium quotes, you first turn to the Internet. You complete a form on a website in order to see quotes. Before you see anything else, however, your phone number is requested. An agent will call you soon with your rate quotes, the site promises.
How much does a 65 year old woman pay for Medigap?
For example, a 65-year-old woman living in Florida pays an average of $195 in monthly premiums for Plan F. If she were living in Texas, the same woman would only be paying around $123 in monthly premiums for the same plan.
How much does Plan G cost?
Plan G quotes average roughly $169 per month for a woman who is the same age, living in the same ZIP Code. Texas follows the same pattern, with the 65-year-old man paying $112 on average for Plan G and the 65-year-old woman paying around $98. Not all states use your sex/gender to determine your Medigap premiums.
Is Medigap the same as Plan G?
This means that each letter plan has a set of benefits that will stay the same regardless of the carrier. The benefits will be identical if you go with a Plan G through Aetna or Cigna; the only difference will be the premium you pay.
Does Medigap have the same premiums as my neighbor?
Medigap Premium Rates Are Impacted by Multiple Factors. Even if your neighbor has the same Medigap letter plan through the same carrier as you, their premium will not be the same as yours. This is due to several factors that impact premium rates. It’s important to remember that all Medigap plans are standardized by the government.
What is Medicare Advantage?
Essentially: Medicare Advantage – Private plans that replace your Parts A, B, and in most cases, D. Also known as Part C. Medicare Part D – Prescription drug coverage plans, introduced in 2006. Generally, if you’re on Medicare, you aren’t charged a premium for Part A.
How much will Medicare premiums be in 2021?
There are six income tiers for Medicare premiums in 2021. As stated earlier, the standard Part B premium amount that most people are expected to pay is $148.50 month. But, if your MAGI exceeds an income bracket — even by just $1 — you are moved to the next tier and will have to pay the higher premium.
Why did Medicare Part B premiums increase in 2021?
That’s because 2021 Medicare Part B premiums increased across the board due to rising healthcare costs. Exactly how much your premiums increased though, isn’t based on your current health or Medicare plan or your income. Rather, it’s the soaring prices of overall healthcare.
How much of Medicare Part B is paid?
But the remaining 25% of Medicare Part B expenses are paid through your premium, which is determined by your income level. Medicare prices are quoted under the assumption you have an average income. If your income level exceeds a certain threshold, you will have to pay more.
Why are Social Security beneficiaries paying less than the full amount?
In 2016, 2017, and 2018, the Social Security COLA amount for most beneficiaries wasn’t enough to cover the full cost of the Part B premium increases, so most enrollees were paying less than the full amount, because they were protected by the hold harmless rule.
How much is Part B 2021?
So most beneficiaries are paying the standard $148.50/month for Part B in 2021. The hold harmless provision does NOT protect you if you are new to Medicare and/or Social Security, not receiving Social Security benefits, or are in a high-income bracket.
What are some changes you may make by choice?
The beginning of the year always brings about change. Some are changes you may make by choice, like deciding to quit smoking or being more active. And others are changes that have been determined for you, like changes to your Medicare monthly premiums.
What are the two types of Medicare Supplement Ratings?
Insurance companies use two types of ratings systems to determine how they will charge premiums of Medicare Supplement plans: Community Rating: This type of rating system does not allow the insurance company to use health status or claims experience to set rates for plans.
When should Medicare Supplement rate increase history be considered?
The only time that Medicare Supplement rate increase history should be considered is when the company has been in the market less than four years. Here’s why: Insurance companies that have just entered the market don’t have a claim history.
How to evaluate insurance companies?
They best way to evaluate a company boils down to four things: 1 Rate – Does the insurance company charge closer to the lower end of the market or the higher end? 2 Customer Service – You want an insurance company that provides great service to its members with a team that is knowledgeable about their products and responds quickly when you contact them. 3 Time in Market – Personally, I don’t offer companies with less than four years of market history. Most of the companies that I offer have at least 20 years in the Michigan Medicare Supplement market. They tend to have better claims experience and are managed for long term stability. 4 The Agent – The truth is if you’ve been with a Medicare Supplement company for more than 5 years, there tends to be a better rate for you. You should work with an insurance agent that keeps an eye on your policy after your purchase one and is available after the sale for customer service questions.
What is a claim experience rate increase?
Claims experience rate increase are based on the claims that an insurance company receives in a year vs what the collect in premiums from their clients within a specific group.
Why do insurance companies increase their rates after the first year?
After the first year, the rates have the largest increases because claim history starts to accumulate. By the end of the first four years, the company has stabilized on claims and premium.
Can you use smoking status to determine premiums?
While they can’t use health status and claims experience to determine premiums, they can use smoking status, age, and location to vary premiums. Attained Age Rating: This type of rating system sets the premium based on your age when you enroll. This starts lower than a community rating.
Is Medicare Supplement overrated?
As noted above, Medicare Supplement rate increase history is highly overrated based on the following features: Rate increase history does not dictate future rate increase. Most insurance companies are only in the market for a few years and their increases are not enough data to make a reasonable determination.
How to compare Medicare Supplement Plans 2021?
How to Compare Medicare Supplement Plans. You can use the 2021 Medigap plan chart below to compare the benefits that are offered by each type of plan. Use the scroll bar at the bottom of the chart to view all plans and information. Click here to view enlarged chart. Scroll to the right to continue reading the chart. Scroll for more.
What is the most popular Medicare Supplement?
Medigap Plan F is the most popular Medicare Supplement Insurance plan . 53 percent of all Medigap beneficiaries are enrolled in Plan F. 2. Plan F covers more standardized out-of-pocket Medicare costs than any other Medigap plan. In fact, Plan F covers all 9 of the standardized Medigap benefits a plan may offer.
How much is the Medicare Part B deductible for 2021?
In 2021, the Part B deductible is $203 per year. Medicare Part B coinsurance or copayment. After you meet your Part B deductible, you are typically required to pay a coinsurance or copay of 20 percent of the Medicare-approved amount for your covered services.
What is the second most popular Medicare plan?
Medigap Plan G is the second most popular Medigap plan, and it is quickly growing in popularity. Plan G enrollment spiked 39 percent in recent years. 2. Medigap Plan G covers all of the same out-of-pocket Medicare costs than Plan F covers, except for the Medicare Part B deductible.
What are the benefits of Medigap?
Here are some key facts about Medicare Supplement Insurance: 1 Medigap insurance doesn't typically offer any additional benefits. Instead, it picks up the out-of-pocket costs associated with Medicare. 2 Medigap insurance is accepted by any doctor, hospital or health care provider who accepts Medicare. 3 If your health care service or medical device is covered by Medicare, your Medigap plan would cover any additional out of pocket costs so that you don't pay anything for your services (depending on your Medigap plan coverage and whether or not you've reached certain Medicare deductibles).
How much coinsurance is required for skilled nursing?
There is no coinsurance requirement for the first 20 days of inpatient skilled nursing facility care. However, a $185.50 per day coinsurance requirement begins on day 21 of your stay, and you are then responsible for all costs after day 101 of inpatient skilled nursing facility care (in 2021).
How much does Medicare Part A cover?
Medicare Part A helps cover your hospital costs if you are admitted to a hospital for inpatient treatment (after you reach your Medicare Part A deductible, which is $1,484 per benefit period in 2021). For the first 60 days of your hospital stay, you aren't required to pay any Part A coinsurance.