Get a letter that tells you about the likely risk to the privacy of your information ("breach notification"). Get a separate paper copy of this notice. You may file a privacy complaint with:
Full Answer
What is the privacy policy for Medicare?
This privacy policy describes what information we collect, why we collect it, and what we do with it. This privacy notice is for Medicare.gov, es.Medicare.gov, and other Medicare.gov subdirectories, like Medicare.gov/physiciancompare.
Do patients have a right to a privacy notice?
Patients have the right to receive a notice explaining how a provider or health plan uses and discloses their health information. a. How do patients get a notice of privacy practices? Health care providers usually give patients this notice on their first visit and post it in the facility where patients may see it.
What rights do patients have under the HIPAA Privacy Rule?
This guide explains the rights that patients have under the HIPAA Privacy Rule. It also answers many questions the Privacy Rights Clearinghouse receives from individuals on a regular basis. For more information about HIPAA and medical privacy, see Privacy Rights Clearinghouse: Medical Privacy. 2. The right to receive a notice of privacy practices
What does it mean when a provider does not accept Medicare?
This means that while non-participating providers have signed up to accept Medicare insurance, they do not accept Medicare’s approved amount for health care services as full payment. Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ).
Can disclose information to Medicare CMS without consent?
If a Medicare provider or supplier is a covered entity, it is subject to the Privacy Rule which implements provisions of the Health Insurance Portability and Accountability Act of 1996 (HIPAA), and generally cannot disclose protected health information on Medicare beneficiaries or other patients without the permission ...
What are 3 rights everyone on Medicare has?
— Call your plan if you have a Medicare Advantage Plan, other Medicare health plan, or a Medicare Prescription Drug Plan. Have access to doctors, specialists, and hospitals. can understand, and participate in treatment decisions. You have the right to participate fully in all your health care decisions.
Does Medicare sell your personal information?
We don't sell any information you provide when you visit Medicare.gov. For information on how we share information, see How CMS uses information collected on Medicare.gov.
How does Medicare affect patient access to care?
February 03, 2021 - Medicare coverage increases seniors' access to care and reduces affordability barriers, a study published in Health Affairs discovered. “The Medicare program pays for roughly one of every four physician visits in the United States, and in 2019 it covered roughly 60 million people.
What are some problems with Medicare?
"Medicare is not complete coverage. It doesn't include dental, vision and hearing. It doesn't cover long-term care. There can be high out-of-pocket costs if you don't have supplemental coverage, and supplemental coverage in Medicare is complicated," said Roberts, who wrote an editorial that accompanied the new study.
Can a doctor refuse to treat a Medicare patient?
Can Doctors Refuse Medicare? The short answer is "yes." Thanks to the federal program's low reimbursement rates, stringent rules, and grueling paperwork process, many doctors are refusing to accept Medicare's payment for services. Medicare typically pays doctors only 80% of what private health insurance pays.
Can Medicare look at your bank account?
Medicare plans and people who represent them can't do any of these things: Ask for your Social Security Number, bank account number, or credit card information unless it's needed to verify membership, determine enrollment eligibility, or process an enrollment request.
What is considered Medicare abuse?
What Is Medicare Abuse? Abuse describes practices that may directly or indirectly result in unnecessary costs to the Medicare Program. Abuse includes any practice that does not provide patients with medically necessary services or meet professionally recognized standards of care.
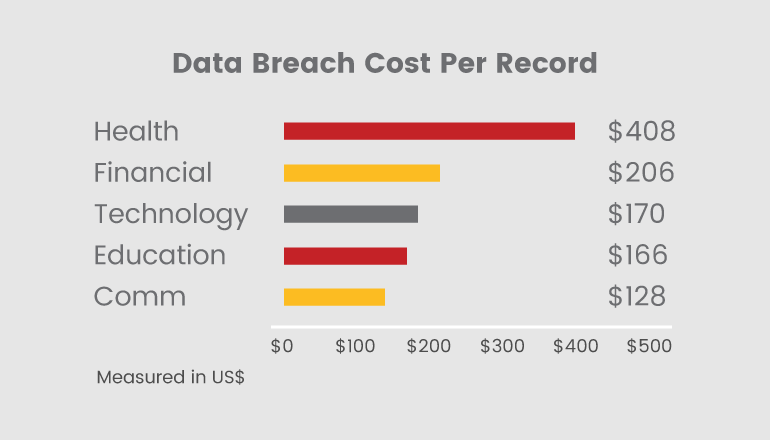
Can someone steal my identity with my Medicare number?
Medical identity theft happens when someone steals or uses your personal information (like your name, Social Security Number, or Medicare Number) to submit fraudulent claims to Medicare and other health insurers without your permission. Medicare is working to find and prevent fraud and abuse.
How has Medicare helped the elderly?
Medicare guarantees affordable health insurance. And it helps insulate beneficiaries from rising health care costs. People enrolled in the program may still pay thousands of dollars a year for health care, but their access to health care is vastly better than before the program existed.
Is Medicare affordable?
Beneficiaries in traditional Medicare with no supplemental coverage are vulnerable to high out-of-pocket expenses because Medicare, unlike marketplace and large employer plans, has no cap on out-of-pocket spending for covered services. But even those with supplemental coverage can face affordability challenges.
Who is Medicare through?
The Centers for Medicare & Medicaid Services (CMS) is the federal agency that runs Medicare. The program is funded in part by Social Security and Medicare taxes you pay on your income, in part through premiums that people with Medicare pay, and in part by the federal budget.
What is the Medicare deductible for 2020?
In 2020, the Medicare Part B deductible is $198 per year.
What was the Medicare deductible for 2019?
In 2019, the Medicare Part B deductible is $185 per year.
What counts toward the Medicare Part B deductible?
Basically, any service or item that is covered by Part B counts toward your Part B deductible.
What happens once you reach the deductible?
Once you meet the required Medicare Part B deductible, you will typically be charged a 20 percent coinsurance for all Part B-covered services and i...
Is there a way to avoid paying the Medicare Part B deductible?
There are two ways you may be able to avoid having to pay the Medicare Part B deductible: Medicare Supplement Insurance or a Medicare Advantage plan.
There are certain people who have a right to obtain your information
Medicare is required to share your information with the following parties, when requested:
There are certain circumstances in which Medicare may use or share your information
Medicare is allowed to share your personal information under the following circumstances:
You have rights as a Medicare beneficiary
As a Medicare beneficiary, you are protected by certain rights concerning your private information.
You may have additional Medicare coverage options
Depending on where you live, there may be Medicare Advantage (Medicare Part C) and Medicare Part D prescription drug plans available in your area.
What is a cookie on Medicare.gov?
During a visit to Medicare.gov, a cookie is placed in the browser of the devices used to view the website. When that same device is used to visit third-party websites that are displaying Medicare.gov ads, ads for Medicare.gov may be shown to that device because it had previously visited Medicare.gov.
How old do you have to be to call Medicare?
Medicare.gov isn’t intended to solicit information of any kind from children under age 13. If you believe that we've received information from a child under age 13, call us at 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
Does CMS use cookies?
We don’t identify a user by using cookies. CMS also uses these technologies on Medicare.gov: Persistent cookies for digital advertising: Similar to persistent cookies identified above, CMS uses persistent cookies for outreach through digital advertising.
Does Medicare.gov collect information?
Medicare.gov doesn’t collect name, contact information, Medicare Number, or other similar information through these websites unless you choose to provide it. We do collect other, limited, non-personally identifiable information automatically from visitors who read, browse, and/or download information from our website.
Does Medicare have a privacy manager?
Medicare.gov offers a Privacy Manager which gives you control over what tracking and data collection takes place during your visit. Third-party tools are enabled by default to provide a quality consumer experience.
What are written privacy procedures?
These include who has access to protected information, how it will be used within the entity, and when the information may be disclosed. Covered entities will also need to take steps to ensure that their business associates protect the privacy of health information.
When did the HHS pass the privacy law?
The law gave Congress until August 21, 1999, to pass comprehensive health privacy legislation. When Congress did not enact such legislation after three years, the law required the Department of Health and Human Services (HHS) to craft such protections by regulation. In November 1999, HHS published proposed regulations to guarantee patients new ...
How long do covered entities have to comply with HIPAA?
As required by the HIPAA law, most covered entities have two full years - until April 14, 2003 - to comply with the final rule's provisions. The law gives HHS the authority to make appropriate changes to the rule prior to the compliance date. COVERED ENTITIES.
What is the final rule of privacy?
The final rule establishes the privacy safeguard standards that covered entities must meet, but it gives covered entities the flexibility to design their own policies and procedures to meet those standards.
What are the rights of patients under the final rule?
Under the final rule, patients will have significant new rights to understand and control how their health information is used. Patient education on privacy protections. Providers and health plans will be required to give patients a clear written explanation of how the covered entity may use and disclose their health information.
What is information protected?
INFORMATION PROTECTED. All medical records and other individually identifiable health information used or disclosed by a covered entity in any form, whether electronically, on paper, or orally, are covered by the final rule . CONSUMER CONTROL OVER HEALTH INFORMATION.
Why are psychotherapy notes considered sensitive?
Psychotherapy notes (used only by a psychotherapist) are held to a higher standard of protection because they are not part of the medical record and are never intended to be shared with anyone else. All other personal health information is considered to be sensitive and protected consistently under this rule.
How often do you have to send a health plan notice?
A health plan must give its notice to you at enrollment. It must also send a reminder at least once every three years that you can ask for the notice at any time. A health plan can give the notice to the “named insured” (subscriber for coverage).
What happens if you refuse to sign an acknowledgement?
If you refuse to sign the acknowledgement, the provider must keep a record of this fact.
Can a health plan give a notice to a spouse?
A health plan can give the notice to the “named insured” (subscriber for coverage). It does not also have to give separate notices to spouses and dependents. Content created by Office for Civil Rights (OCR) Content last reviewed on November 2, 2020.
Do you have to sign an acknowledgement of receipt?
The law does not require you to sign the “acknowledgement of receipt of the notice.”. Signing does not mean that you have agreed to any special uses or disclosures (sharing) of your health records. Refusing to sign the acknowledgement does not prevent a provider or plan from using or disclosing health information as HIPAA permits.
Why do doctors need to share information?
Doctors, nurses and hospitals need to share your information to ensure that you're getting the proper treatment and meds, and that none of those treatments conflict. Insurance companies require the same information to verify claims. Government agencies may request medical records to verify claims made through Social Security, ...
Why are electronic medical records important?
A. Electronic medical records (EMRs) provide health care providers with quick access to your information and a real-time tool to improve the quality of health care, as well as prevent medical errors and increase administrative efficiencies. In spite of their convenience, EMRs may make it harder to protect your privacy; when information is communicated electronically, there is always potential for security breaches. But keep in mind that providers of EMRs are laser-focused on these dangers, making EMRs more reliable and less vulnerable than an open chart left on a hospital counter.
What is the information on a doctor's credit report?
Information provided includes your name and address, your date of birth, Social Security number, your payment history and the name of the health provider owed money.
Can health care providers disclose health information?
Individual and group health plans, health care clearinghouses and health care providers may not disclose health information for marketing or provide data to a third party for marketing in exchange for direct or indirect payment unless there is authorization from the patient.
Can insurance companies share your medical history?
A. Absolutely not. One insurance company sharing your claims history with another would be considered unauthorized disclosure to a third party, which is a HIP AA violation. Insurers may access individual doctors' files for underwriting purposes, but only once you disclose your physicians' names in your application for coverage.
Can family members see medical records?
A. It depends. Although federal law does not prohibit ordinary health care practices — such as hospital staff discussing your condition and your treatment options with family members, or picking up a prescription for a relative — you must give written permission for your loved ones to see your official medical records. By designating family members as your "personal representative" in a signed letter or form, you give the health care providers the coverage they require to avoid HIPAA violations. So it's a good idea for you and aging parents — or adult children — to designate one another as personal representatives in case the need arises.
Can employers deny you a job based on genetic information?
A 2008 federal law prohibits employers from denying you a job or firing you, and health insurers from refusing coverage, based on genetic information. If you believe your rights have been violated, you can file a complaint with your provider or health insurer or with the U.S. Department of Health and Human Services. 4.
How does HIPAA Privacy Rule work?
describe how the HIPAA Privacy Rule allows the covered entity to use and share protected health information (PHI), and state that it will obtain the patient's permission for any other reason; tell patients about their rights under the HIPAA Privacy Rule; tell patients how to file a complaint with the covered entity;
What is the right to receive a notice of privacy practices?
The right to receive a notice of privacy practices. Patients have the right to receive a notice explaining how a provider or health plan uses and discloses their health information. a.
What is NPP in healthcare?
A notice of privacy practices (NPP) will often contain jargon that can be difficult for patients to understand. For explanations of commonly used HIPAA terms, see Privacy Rights Clearinghouse Fact Sheet 8a: HIPAA Basics.
What does HIPAA charge for?
The covered entity can charge for supplies, staff time for copying and processing, and mailing (if applicable). The covered entity may charge for the time staff spends copying and processing the record.
What is a physician partner?
the physician’s partners; the health information manager or privacy officer at a hospital or facility where the physician practices; a local medical society; the state medical association; or. the state department of health. e.
What happens if a patient doesn't have a copy of the notice?
If a patient doesn’t have a copy of the notice, there may be one on the provider's or health plan’s website. If there isn’t one online, a covered entity's administrative office will be able to provide the information and a copy of the notice. 3. The right to access and request a copy of medical records.
How long does it take to get medical records corrected?
The covered entity must respond to the request within 60 days.