These prior authorizations save money for insurers by bypassing unnecessary or expensive treatment options when other equally effective options exist that are included in the plan’s formulary. The formulary includes the list of medications that are covered under an insurance plan.
Full Answer
What is Medicare prior authorization?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare. Private, for-profit plans often require Prior Authorization.
What services require prior approval from Medicare Advantage?
The services most often requiring prior approval are durable medical equipment, skilled nursing facility stays, and Part B drugs. But, each Advantage plan is different. If you have an Advantage plan, contact your plan provider to determine if or when prior authorization is necessary.
How much does prior authorization cost providers?
Processed prior authorization (PA) amounted to a $528 million administrative cost for providers in 2019. PA increased in both cost and the amount of time per transaction. Health plans warn another increase in the use of PA is coming.
Should the federal government require automated prior authorization?
“The federal government needs to streamline prior authorization by requiring a national automated approach to minimize administrative costs and delays in patient care.” Providers would save $355 million annually from a complete shift to electronic PA processes, according to the CAQH report.
How much money does prior authorization save?
The just released CAQH 2019 Index, which concluded that the healthcare industry can save $13.3 billion on administrative waste through automation of eight transactions including prior authorizations, said the medical industry could see potential annual savings of $454 million by transitioning to electronic prior ...
What are the benefits of prior authorization?
The prior authorization process can help you:Reduce the cost of expensive treatments and prescriptions by first requiring you to try a lower-cost alternative.Avoid potentially dangerous medication combinations.Avoid prescribed treatments and medications you may not need or those that could be addictive.
What is a prior authorization and why do you need it?
A prior authorization (PA), sometimes referred to as a “pre-authorization,” is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
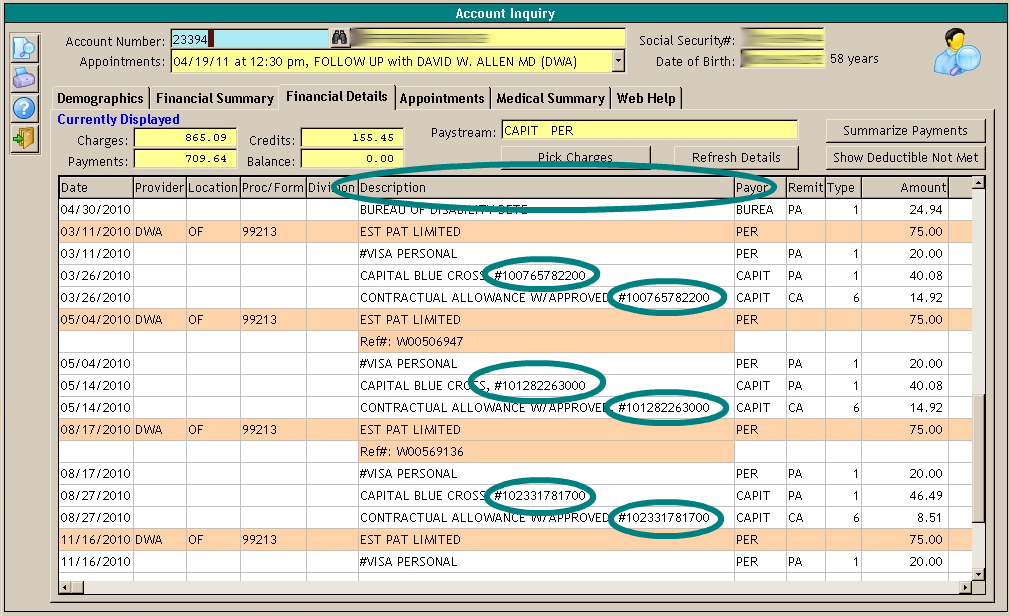
How do you deal with prior authorization in medical billing?
Foremost Task: Ensure the CPT code is CorrectBest Practices for Prior Authorization: ... Keep Necessary Information Ready : ... Follow recommended treatment guidelines: ... Meet all Payer Criteria: ... Get Preauthorization for Mundane Procedures: ... Monitor Insurance Carrier Websites Regularly: ... Update Contracts with Insurance Companies:More items...•
What is prior authorization Medicare?
Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
What happens if you don't get prior authorization?
If you're facing a prior-authorization requirement, also known as a pre-authorization requirement, you must get your health plan's permission before you receive the healthcare service or drug that requires it. If you don't get permission from your health plan, your health insurance won't pay for the service.
How do pre authorizations work?
A pre-authorization is a restriction placed on certain medications, tests, or health services by your insurance company that requires your doctor to first check and be granted permission before your plan will cover the item.
What does it mean when a pharmacy needs a prior authorization?
When your pharmacist tells you that your prescription needs a prior authorization, it simply means that more information is needed to see if your plan covers the drug. Only your doctor can provide this information and request a prior authorization.
Why is it important to get preauthorization if the patient's insurance requires you to do so?
Before certain procedures can be preformed or a patient hospitalization, many insurance companies require precertification's or preauthorization. If this is not done, insurance claims will be denied.
Why authorization is important in medical billing?
Authorization does not guarantee payment of bills. However, not having a pre-approval can result in non-payment or denial of the bills. Thus, prior authorization services in medical billing is important for faster claims and better financial position of the organization.
What is a pre-authorization amount?
Also commonly referred to as a “pre-auth” or “auth-only”, is a pre-authorization that places a hold on your customer's credit card for a specified dollar amount based on a projected sale amount. This guarantees you access to their credit limit for the specified amount.
What is the difference between precertification and prior authorization?
Prior authorization—sometimes called precertification or prior approval—is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.
What steps are some insurers taking to reduce wait times?
Some companies, such as Cigna, are trying to close the time gaps with improved technology that would pull information directly from the EHR.
What is the Patients Role in the Pre-authorization Process?
Providers need to educate patients that having insurance doesn’t mean that they will automatically receive an array of tests and treatments on demand. Evidence-based guidelines dictate that unless a given test or treatment is medically necessary, it won’t be covered, whether or not the patient is insured.
Have a dedicated staff integrated into practice workflow
Physicians and other care delivery providers are particularly frustrated with the administrative burdens of prior authorizations. Providers overwhelmingly agree that prior approvals for services and prescriptions are a regulatory burden, delay patient access to care, and create unnecessary work.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Does Medicare cover CT scans?
If your CT scan is medically necessary and the provider (s) accept (s) Medicare assignment, Part B will cover it. Again, you might need prior authorization to see an out-of-network doctor if you have an Advantage plan.
What is CMS in Medicare?
The Centers for Medicare & Medicaid Services (CMS) runs a variety of programs that support efforts to safeguard beneficiaries’ access to medically necessary items and services while reducing improper Medicare billing and payments. Through prior authorization and pre-claim review initiatives, CMS helps ensure compliance with Medicare rules.
What is pre claim review?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submitting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical ...
How much does a PA transaction cost?
The PA cost per manual transaction increased from $6.60 in 2018 to $10.92 in 2019. PA time per manual transaction increased from 16 minutes in 2018 to 21 minutes in 2019.
How much does PA processing cost?
Providers’ PA processing cost was $528 million in 2019 (no total cost was estimated in 2018). Provider savings from switching to electronic PA increased from $278 million in 2018 to $355 million in 2019. The PA cost per manual transaction increased from $6.60 in 2018 to $10.92 in 2019.
Does Medicare and Medicaid have PA standards?
As part of that effort, in November, the American Hospital Association urged the Centers for Medicare & Medicaid Services to develop PA standards and increase its oversight of the health plans the agency regulates. CAQH has adopted some voluntary health plan rules that aim to ease PA burdens, Todd said.
Is PA increasing in cost?
PA increased in both cost and the amount of time per transaction. Health plans warn another increase in the use of PA is coming. Providers’ costs and time consumption from prior authorization (PA) markedly increased in 2019, according to a not-for-profit alliance.
Does CAQH have HIPAA?
CAQH has adopted some voluntary health plan rules that aim to ease PA burdens, Todd said. And in 2020 it plans submit to federal regulators recommendations for requiring health plan changes through HIPAA. “There are definitely efforts underway to move that very manual process to a more electronic process,” Todd said.
What is prior authorization?
Prior authorization – also known as precertification, preauthorization, prior approval, prior notification, prospective review, and prior review – requires health care providers to establish eligibility and obtain approval from the patient’s health plan before care is delivered to qualify for payment. Payers use PA as a strategy to reduce utilization of overused or low-value services, reduce spending, and improve care quality.1 Health care payers employ physicians, nurses, and other health care professionals to support the development and execution of PA policies. These policies are routinely updated based on new treatments and medical guidelines, and their application can accelerate the adoption of new standards of care.
How to apply for PA?
The process of applying for and receiving PA varies by payer, but generally involves obtaining the payer’s PA form, completing all required clinical and administrative information, submitting the form to the health plan, and, if needed, contacting service representatives or other personnel at the plan for follow up.
How does PA affect health care?
There are a modest number of studies on the impacts of PA programs on health care utilization and spending. Prescription drug applications have been received the most study. Some research has also examined use of PA for imaging, medical devices, transportation, and other therapies. The research shows that PA programs reduce utilization of the targeted treatment, sometimes with offsetting increased use of preferred treatments. The evidence also shows PA programs generally reduce spending on the targeted care, although where overall health care costs are tracked, the PA-focused reductions do not always translate to lower overall health spending. While the evidence base is not substantial enough to draw firm conclusions, PA effectiveness has varied by the type of care to which it has been applied. Brief summaries of selected research findings on the impacts of PA on health care use, cost, and quality for various types of care follow. Medical imaging. There is evidence that PA for medical imaging can be effective in reducing utilization and associated health care costs. Multiple studies have found PA policies were associated with reduced use of magnetic resonance imaging, computer-aided tomography scanning, and cardiac imaging.10
What is PA policy?
Prior authorization (PA) policies are used to varying degrees by both public and private payers to manage the use of costly or potentially avoidable care. Prescription drugs, durable medical equipment, and diagnostic radiology are common targets.
Why are PA requests delayed?
Often, approvals of authorization requests are delayed due to missing information. Consistency in submission processes would make it easier to develop manual or automated systems to meet information requirements and reduce such delays.
Does automation reduce PAs?
While automation does not reduce the number of PAs, it can make the processing of PAs less burdensome and more uniform across health plans and pharmacy benefit managers. Providers who exclusively use an electronic method for PA requests have reported spending on average 2.5 fewer hours on PA each week. However, few providers find themselves exclusively using a single solution, with 76% reportedly using more than one channel to complete PA requests.
Is PA covered by Medicare?
While commercial insurers have been implementing PA policies for many years, the use of PA under Medicare has historically been limited. Recent demonstration programs and the growing role of managed care organizations in delivering care to Medicare and Medicaid enrollees are expanding the use of PA for the publicly insured.

What Steps Are Some Insurers Taking to Reduce Wait Times?
What Is The Patients Role in The Pre-Authorization Process?
- Providers need to educate patients that having insurance doesn’t mean thatthey will automatically receive an array of tests and treatments on demand.Evidence-based guidelines dictate that unless a given test or treatment ismedically necessary, it won’t be covered, whether or not the patient isinsured. An example is a patient demanding an MRI for ba...
Have A Dedicated Staff Integrated Into Practice Workflow
- Physicians and other care delivery providers are particularly frustratedwith the administrative burdens of prior authorizations. Providersoverwhelmingly agree that prior approvals for services and prescriptions are aregulatory burden, delay patient access to care, and create unnecessary work. Shifting the responsibility of prior authorizations to a dedicated staffcould help to reduce t…