
In order to opt-out, providers must submit an Opt Out Affidavit with Medicare and must keep a Private Contract with all beneficiaries on file for each two-year period. Follow the below links to learn more about opting out. Providers who do not wish to enroll in the Medicare program, may opt-out.
Full Answer
What does it mean when doctors “opt out” of Medicare?
An opt-out doctor is one who doesn't accept Medicare. Doctors who have opted out of Medicare can charge their Medicare patients whatever fees the physicians choose. These doctors don't submit any health care claims to Medicare. In addition, opt-out doctors aren't subject to Medicare laws that limit the amount they can charge their patients.
Can You unenroll from Medicare?
You can unenroll from Medicare Part D during the standard Open Enrollment Period, or during one of the following special circumstances: You moved to a new address that’s outside your plan’s service area. You moved to an address that’s still in your plan’s service area, but you have new plan options in your new location.
How to disenroll from Medicare?
To disenroll from a Part D plan, you can:
- Call Medicare directly
- Get in contact with your Part D plan provider
- Submit a disenrollment request from your provider
- Mail a signed letter to your provider
How do I find out if I have Medicare?
- ZIP code
- Medicare number
- last name
- date of birth
- Medicare Part A effective date
How can you opt out of Medicare?
In order to opt out you must file an opt-out affidavit with the Medicare Administrative Contractor (MAC) or Carrier that administers any jurisdiction you practice in. A template for this affidavit that conforms to Medicare rules follows.
Why would a physician opt out of Medicare?
There are several reasons doctors opt out of Medicare. The biggest are less stress, less risk of regulation and litigation trouble, more time with patients, more free time for themselves, greater efficiency, and ultimately, higher take home pay.
What is a Medicare opt out form?
Opt out is a contract between a provider, beneficiary and Medicare where the provider or beneficiary does not file a claim to Medicare. The physician or practitioner bills the beneficiary directly and is not required to follow the fee-for-service charges determined by Medicare.
Can PTs opt out of Medicare?
Unlike many other types of practitioners, physical therapists cannot “opt out” of Medicare. In fact, the closest thing PTs have to “opting out” is simply not having any type of relationship with Medicare.
Can a provider refuse to bill Medicare?
In summary, a provider, whether participating or nonparticipating in Medicare, is required to bill Medicare for all covered services provided. If the provider has reason to believe that a covered service may be excluded because it may be found not to be reasonable and necessary the patient should be provided an ABN.
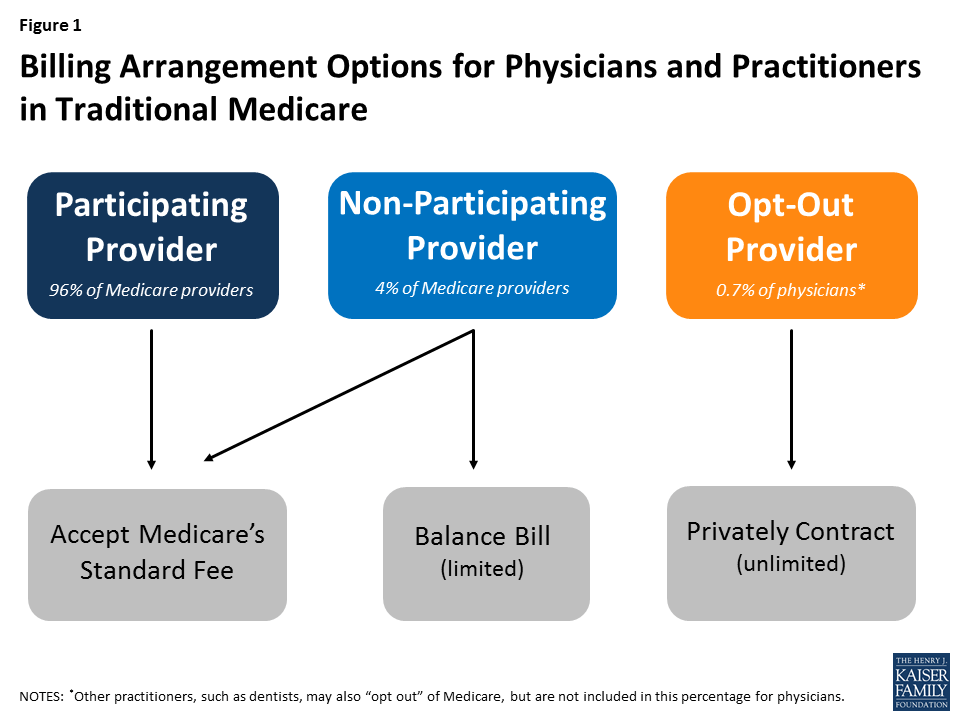
What does it mean if a doctor does not accept Medicare assignment?
A: If your doctor doesn't “accept assignment,” (ie, is a non-participating provider) it means he or she might see Medicare patients and accept Medicare reimbursement as partial payment, but wants to be paid more than the amount that Medicare is willing to pay.
How do I refuse Medicare Part B?
Call the Social Security Administration at 800-772-1213 and ask if you can decline Part B without any penalties. Write down who you spoke with, when you spoke to them and what they said. should write a letter to the Social Security Administration declining Part B. Keep a copy of the letter for yourself.
How do you opt out of or disenroll from Medicare Part A?
If you want to disenroll from Medicare Part A, you can fill out CMS form 1763 and mail it to your local Social Security Administration Office. Remember, disenrolling from Part A would require you to pay back all the money you may have received from Social Security, as well as any Medicare benefits paid.
What happens if you don't want Medicare?
Will I get enrolled in Medicare if I don't want it? If you don't want Medicare, you still might get enrolled anyway. If you're already getting Social Security benefits when you become eligible for Medicare, you're enrolled automatically in most cases.
How often do you have to opt out of Medicare?
A silver lining in the Medicare Access and CHIP Reauthorization Act of 2015. which was signed into law in mid-April 2015 to repeal the sustainable growth rate (SGR), is a provision in the bill that also repeals the irritating requirement of having to renew an opt-out status every two years. Physicians opting out of Medicare after June 16, 2015 will need to file an affidavit to opt out of Medicare only once, and it will have permanent effect. The physician will no longer need to renew his opt-out every two years thereafter. However patients will still need to sign a private contract every two-years.
Why should doctors get out of Medicare?
Medicare endangers seniors, rations care and punishes the best doctors whose only aim is to give the best care. For the sake of patients and integrity of the profession , doctors should get out of Medicare. If playback doesn't begin shortly, try restarting your device.
How often do you have to renew a Medicare contract?
Step Six: Mark your calendar to have Medicare patients re-sign a new private contract every two year’s on the anniversary of your opt out effective date. While Physicians opting out on or after June 16, 2015 will no longer need to renew their opt out every two years, CMS currently still requires patients to renew the private contract every two years.
When does opt out become effective?
Participating physicians’ opt out status only becomes effective at the beginning of a calendar quarter, when the affidavit is sent in at least 30 days before the first day of the quarter.) Step One: Notify your patients that you are opting out of Medicare.
How long does a physician have to provide private contracting services?
Subsequent Steps: Follow the above Steps One through Six for a non-participating physician, except that the physician may not provide private contracting services until the first date of the next quarter that is at least 30 days after receipt of the notice by the carrier. For example, the carrier must receive the notice from the physician by Sept. 1 if the physician seeks to provide private contracting services beginning on Oct. 1.
What to do if playback doesn't begin?
If playback doesn't begin shortly, try restarting your device.
Can a patient submit a claim to Medicare?
Patient agrees not to submit a claim (or to request that Physician submit a claim) to the Medicare program with respect to the Services, even if covered by Medicare Part B. Patient is not currently in an emergency or urgent health care situation.
How much can non-participating providers charge for Medicare?
Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
What happens if you pay Medicare up front?
If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount.
What does it mean to take assignment with Medicare?
Taking assignment means that the provider accepts Medicare’s approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive.
How long does it take for a provider to bill Medicare?
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you.
Does Medicare charge 20% coinsurance?
However, they can still charge you a 20% coinsurance and any applicable deductible amount. Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Do opt out providers accept Medicare?
Opt-out providers do not accept Medicare at all and have signed an agreement to be excluded from the Medicare program. This means they can charge whatever they want for services but must follow certain rules to do so. Medicare will not pay for care you receive from an opt-out provider (except in emergencies).
Can you have Part B if you have original Medicare?
Register. If you have Original Medicare, your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare.
What happens if a provider opts out of Medicare?
Once a provider opts out of Medicare, they are opted out across the United States of America and territories. If the provider goes from one MAC to another, an additional opt out affidavit is required to be submitted to the new MAC.
What is opt out in Medicare?
Opt out is a contract between a provider, beneficiary and Medicare where the provider or beneficiary does not file a claim to Medicare. The physician or practitioner bills the beneficiary directly and is not required to follow the fee-for-service charges determined by Medicare.
How often do opt out providers get renewed?
Current opt out providers are automatically renewed every two (2) years. If an affidavit has not been signed and received by the Medicare contract on/after June 16, 2015, a new affidavit must be submitted to start a new opt out period.
How long does it take for a provider to opt out of a program?
A providers opt out status may be voluntarily terminated within 90 days of the affidavit if a provider has not previously been in an opt out status.
How long do you have to keep a private contract with Medicare?
In order to opt-out, providers must submit an Opt Out Affidavit with Medicare and must keep a Private Contract with all beneficiaries on file for each two-year period. Follow the below links to learn more about opting out.
How long does it take to cancel Medicare?
If a provider wishes to end his/her opt out status and reenroll in Medicare, he/she must submit the cancellation request via a letter 30 days before the opt out is due to expire. If the cancellation letter is submitted after the 30 days , he/she will remain opted out for another 2-year cycle. This must be mailed in.
When is the opt out date for Medicare 2021?
Example: #2: If we received the affidavit on July 5, 2021; then the opt out effective date would be October 1, 2021. If the provider has been previously enrolled in Medicare and were set-up as a Non-PAR provider, then the affidavit can be submitted any time. The effective date would be the day the affidavit was signed.
What does it mean to opt out of Medicare?
Opting out of the Medicare program means that the given physician or practitioner does not bill or file claims to Medicare. Medicare beneficiaries can be seen under private contract. This means that the Medicare beneficiary pays the physician or practitioner under the terms of the contract. The Medicare beneficiary further agrees not ...
How long does it take to get an affidavit from Medicare?
An affidavit must be filed with a Medicare Administrative Contractor (MAC) first. There is then a two-year process, with the affidavit automatically renewing after two years unless the physician or practitioner intervenes. Opting out of the Medicare program means that the given physician or practitioner does not bill or file claims to Medicare.
Can an opt out physician file a claim with Medicare?
For instance, if an opt-out physician were to see a Medicare beneficiary in a hospital’s ER with whom the physician had no contract, then the physician would be able to file a claim with Medicare. If the encounter were for a laceration, then concern would be focused on the medical condition (that is, is it emergent or urgent?) This requires clinical judgement.
Is there a contract between a physician and a Medicare beneficiary?
Of course, this presumes that there is no private contract between the Medicare beneficiary and the physician. If there is a contract, then the urgent or emergent care falls under the contract. What is needed is a formal billing definition of emergent and urgent care.
Can a Medicare beneficiary opt out of Medicare?
The Medicare beneficiary further agrees not to file a claim with Medicare themselves. Opting out of Medicare is an all-or-nothing proposition. Either the physician enrolls (e.g., CMS-855-I, CMS-885-R, etc.) or the physician has nothing to do with the Medicare program.
Is opting out a contract?
Of course, this presumes that there is no private contract between the Medicare beneficiary and the physician. If there is a contract, then the urgent or emergent care falls under the contract.
Is an opt out physician a referring physician?
The answer to the latter question is that the opt-out physician may be a referring or ordering physician. This is a very short list of possible situations. Whether you are a hospital, clinic, or individual physician, the whole world of opt-out physicians and practitioners creates compliance issues, particularly for coding, billing, ...
How to cancel opt out on Mac?
To cancel your opt-out status, you’ll need to mail a cancellation request to your MAC at least 30 days before your opt-out period is set to expire. If you don’t submit your cancellation request before the 30-day period, your opt-out status will automatically renew for another two-year cycle.
How long does it take to terminate an opt out?
You can terminate your opt-out status within the first 90 days of submitting an initial opt-out affidavit. (Once an opt-out has been automatically renewed, you can no longer terminate early.)
What happens if you don't withdraw from Medicare?
Failing to withdraw could result in fraudulent billing or having your Medicare billing privileges revoked.
How long does it take to withdraw from Medicare?
Withdraw from Medicare. If you retire, surrender your license, or no longer want to participate in the Medicare program, you must officially withdraw within 90 days. DMEPOS suppliers must withdraw within 30 days.
How often does an opt out affidavit renew?
If you’re currently opted out, your opt-out status will automatically renew every two years. If you submitted an opt-out affidavit before June 16, 2015 and never renewed it, you’ll need to submit a new opt-out affidavit.
When does Medicare coverage apply?
Medicare coverage would apply when you order or certify items and services.
What is a private contract with Medicare?
This contract will reflect the agreement between you and your patients that they will pay out of pocket for services, and that nobody will submit the bill to Medicare for reimbursement.
What does it mean to opt out of Medicare?
Opting out of Medicare allows providers to see Medicare patients under private contract. Many providers, such as Dr. Phil Eskew, Dr. Erika Bliss, and Dr. Robert Lamberts, find this approach more convenient and free of the tangle of Medicare regulations or running afoul of False Claims Act laws.
What are the advantages of being a direct care provider?
For Dr. Lamberts, the advantage of being a Direct Care provider are increased access, more flexibility and power in running your practice. With Medicare, he laments that “You lose all of the advantages of Direct Primary Care if you don’t opt out.”
What are the advantages of direct care?
The advantages of the Direct Care model is the relationship with customers, and with Medicare, many doctors feel they lose that relationship. Doctor Rob Lamberts, sees opting out as the best way to preserve that relationship “unless you choose not to see Medicare patients.”.
Is a physician a Medicare participant?
Physicians may be Medicare participating, non-participating, or opted out. The non-participating status is all but extinct at this stage, as most physicians found it an unuseful category because the charges that can be levied with this status are still limited and controlled by Medicare rates.
Is legal counsel mandatory for Medicare?
If you choose to opt for a fee for non-covered services model (aka “concierge model”) and stay in Medicare, legal counsel is almost mandatory. MDVIP and other “concierge” groups operate in this manner and employ attorneys tasked with regularly following developments in this area. That’s another obstacle between you and your patient.
Is naming your services a violation of the False Claims Act?
Simply naming your services something new may not suffice and may in fact be in violation of the False Claims Act. Medicare auditors (such as RACs or ZPICs) could make the argument that services you believe are non-covered are in fact covered services.
Is there a one size fits all approach to Medicare?
While some may argue otherwise, there is no one size fits all approach to working with Medicare patients as a Direct Care provider. The key is finding a relationship that works for you based on the size and patient makeup of your practice. Give yourself time to make a decision that feels right to your practice, and talk to other practitioners who have opted out, as well as those who have stayed opted in.
What happens if a provider opts out of Medicare?
If a provider “opts-out” of Medicare, he is permitted to contract privately with Medicare patients or beneficiaries to provide covered services. The beneficiary agrees to pay fully out-of-pocket for a Medicare-covered service after signing a private contract between themselves and the provider/practitioner. They then agree not to submit a claim ...
How long does an opt out contract last?
However, the Opt Out effective date must be after the date the provider signs the affidavit. The Opt-Out contract lasts for a two-year period beginning the date the physician or practitioner files and signs an affidavit that he or she has opted out of Medicare. Then the physician or practitioner could decide to return to Medicare ...
Can a physician opt out of Medicare?
Certain physicians and practitioners can "opt out" of Medicare. For purposes of this provision, physicians include doctors of medicine, osteopathy, optometry, podiatric medicine and doctors of dental surgery. Practitioners permitted to opt out are physician assistants, nurse practitioners, clinical nurse specialists, ...
Can a physician treat Medicare beneficiaries?
When Medicare is the secondary payer, and the physician has opted out of Medicare , the physician has agreed to treat Medicare beneficiaries only through private contract. The physician or practitioner must therefore have a private contract with the Medicare beneficiary, notwithstanding that Medicare is the secondary payer. Under this circumstance, no Medicare secondary payments will be made for items and services furnished by the physician or practitioner under the private contract.
Can opt out physicians be on call?
“Opt out” physicians should not be listed on the “on call” list for Medicare patients since they are not billing the Medicare program. In rare circumstances, if the "opt out' physician or practitioner provided emergency care in the hospital emergency room and the critical situation continued after admission to the Intensive Care Unit (ICU) or Critical Care Unit (CCU), she/he could continue to care for the patient until it was no longer urgent.
Can a physician be paid by a beneficiary?
However, if the physician or practitioner continues to grant the organization with the right to bill and be paid for the services he or she furnishes to patients, the organization may bill and be paid by the beneficiary for the services that are provided under the private contract. The decision of a physician or practitioner to opt out ...
Can you get a private contract with Medicare?
No. Since Medicare rules do not apply for services not covered by Medicare, a private contract is not needed. A private contract is needed only for services that are covered by Medicare and where Medicare might make payment if a claim were submitted.
