To claim a refund of Social Security and Medicare taxes, you will need to complete and submit IRS Form 843. When you apply for a refund from the IRS, include either: A letter from your employer stating how much you were reimbursed
How do I claim a social security or Medicare tax refund?
When filing a claim, fill out and submit your Patient Request for Medical Payment form, along with: An itemized bill from your healthcare provider. The bill should include: The date of service. A description of each service. The charge for each service. The place of …
How do I apply for Medicare?
In order to apply for this “Financial Hardship” waiver, the Medicare beneficiary must file form SSA-632-BK with MSPRC which documents their financial situation. Synergy also includes in this request a letter drafted by the Medicare beneficiary (not their attorney) explaining the undue hardship that repaying Medicare would cause.
How do I apply for a refund from the IRS?
Jan 31, 2007 · You must complete and submit IRS Form 843 to claim a refund of Social Security and Medicare taxes. When you apply for a refund from the IRS, include either: A letter from your employer stating how much you were reimbursed
How do I request Medicare reimbursement for my care?
If you fail to pay in full, you get an ITR letter 60–90 days after the initial demand letter. The ITR letter . advises you to refund the overpayment or establish an ERS. If you don’t comply, your MAC refers the debt for collection. We refer the overpayment debt to the Treasury or to a Treasury-designated Debt Collection Center (DCC).
How do you qualify to get $144 back from Medicare?
- Are enrolled in Part A and Part B.
- Do not rely on government or other assistance for your Part B premium.
- Live in the zip code service area of a plan that offers this program.
- Enroll in an MA plan that provides a giveback benefit.
How do I get my Medicare premium refund?
Who qualifies for Medicare B refund?
How does the Medicare Give Back program work?
How long does it take to get a refund from Medicare?
How long does it take Medicare to reimburse?
How much is the Medicare Part B reimbursement?
What is Medicare buyback?
What is the Medicare Part B deductible for 2021?
Can I get Medicare Part B for free?
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
What is the form called for medical payment?
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
Do you have to file a claim with Medicare Advantage?
Medicare services aren’t paid for by Original Medicare. Most Medicare Advantage Plans offer prescription drug coverage. , these plans don’t have to file claims because Medicare pays these private insurance companies a set amount each month.
What is Medicare conditional payment?
Repaying Medicare for conditional payments is a necessary but unpleasant process which can result in a greatly reduced net recovery or no recovery at all for an injured Medicare beneficiary. The Medicare Secondary Payer Statute has a repayment formula that is designed to maximize the return of funds to Medicare and provides no consideration for the future well-being of the Medicare beneficiary. The only consideration that Medicare makes in applying its repayment formula is whether or not the amount of the Medicare Conditional Payments is less than, equal to or greater than the gross settlement. (42 C.F.R. 411.37 (c); 42 C.F.R. 411.37 (d)). Despite Medicare’s blind application of the repayment regulations, there is a way for the injured Medicare beneficiary to increase his/her net recovery. This is by way of obtaining a refund from Medicare which sounds crazy, but it works.
What happens if Medicare conditional payment exceeds gross settlement?
In the worst case scenario where the amount of Medicare Conditional Payments is equal to or exceeds the gross settlement, the injured Medicare beneficiary experiences the harshest treatment. In that circumstance, the Medicare beneficiary must return all of their net settlement (after attorney fees and costs) to Medicare, resulting in a zero net recovery to the plaintiff. The regulations provide:
What is Medicare Secondary Payer Manual?
The Medicare Secondary Payer Manual compiles the statutory and regulatory sources, articulating the criteria in a straight forward manner as follows :
Does Synergy have a waiver for Medicare?
In addition to a request made to MSPRC for a “Financial Hardship” waiver under §1870 (c) of the Social Security Act, Synergy requests a “Best Interest of the Program” waiver direct from CMS under §1870 (b) of the Social Security Act. Requests for a waiver under this statute are often overlooked by even the most seasoned attorneys and lien resolution companies. Synergy however understands that the settlement proceeds for which the Medicare beneficiary is fighting to retain is the only source of a recovery for the injuries sustained and must provide for their future needs. Therefore, Synergy vigorously pursues every avenue that can be used to obtain a refund from Medicare. CMS has authority to waive in full or in part Medicare’s claim for repayment when it is “in the best interest of the program.” This rather vague criteria is nowhere further defined and lies completely at the discretion of CMS.
Can Medicare contractors waive a claim?
Each statute contains different criteria upon which decisions to waive or compromise Medicare’s claim are considered. Additionally, the authority to grant a waiver or compromise under each of these statutes is limited to specific entities. Medicare contractors have authority to consider beneficiary requests for waivers under §1870 (c) of the Act. Whereas, authority to waive Medicare claims under §1862 (b) and to compromise claims under FCCA, is reserved exclusively to the Center for Medicare and Medicaid Services (“CMS”).
Can Medicare waive attorney fees?
If the costs (including attorney fees) are not borne by Medicare beneficiary then under the above regulation Medicare would not have applied the reduction formula to their demand for repayment. Yet informing Medicare that the attorney has waived fees or costs will only result in Medicare increasing its repayment demand in the same amount, still leaving the injured plaintiff with nothing. This leaves the only option of “gifting” all or a portion of the attorney fees back to the client, which involves its own set of tax consequences and potential ethical quandaries.
Can Medicare see settlement funds?
The practical effect of this regulation is seen daily by the attorneys who represent injury victims as they wrestle with the equitable and ethical issues of resolving a policy limits case wherein only the attorneys/Medicare will see any portion of the settlement funds. It may even be the case that the only settlement funds come from the Medicare beneficiary’s own Uninsured Motorist coverage. In that case, the injured plaintiff has been paying premiums for insurance coverage just so Medicare and their attorney can be paid in the event they suffer massive injuries. (See 42 C.F.R. 411.50 (b) authorizing repayment to Medicare from UIM proceeds).
How to claim FICA tax refund?
How to Claim a FICA Tax Refund. To claim a refund of Social Security and Medicare taxes, you will need to complete and submit IRS Form 843 . When you apply for a refund from the IRS, include either: A letter from your employer stating how much you were reimbursed.
How long does it take to get a FICA refund?
Requesting a FICA refund isn't a very quick process. It can take the IRS three to four months to review your request and issue your refund.
What form do I need to file if I am a non-resident?
If you are a non-resident foreign worker on a visa, include a copy of the page from your passport that displays your visa stamp, as well as INS Form I-94 and documentation showing you have permission to work in the United States. You might also have to submit INS Form I-538 and IRS Form 8316. 9
How long does it take to get an ITR letter?
If you fail to pay in full, you get an ITR letter 60–90 days after the initial demand letter. The ITR letter advises you to refund the overpayment or establish an ERS. If you don’t comply, your MAC refers the debt for collection.
What happens if Medicare overpayment exceeds regulation?
Medicare overpayment exceeds regulation and statute properly payable amounts. When Medicare identifies an overpayment, the amount becomes a debt you owe the federal government. Federal law requires we recover all identified overpayments.
What is SSA 1893(f)(2)(A)?
SSA Section 1893(f)(2)(A) outlines Medicare overpayment recoupment limitations. When CMS and MACs get a valid first- or second-level overpayment appeal , subject to certain limitations , we can’t recoup the overpayment until there’s an appeal decision. This affects recoupment timeframes. Get more information about which overpayments we subject to recoupment limitation at
How long does it take to submit a rebuttal to a MAC?
Rebuttal: Submit a rebuttal within 15 calendar days from the date you get your MAC’s demand letter. Explain or provide evidence why no recoupment should occur. The MAC promptly evaluates your rebuttal statement.
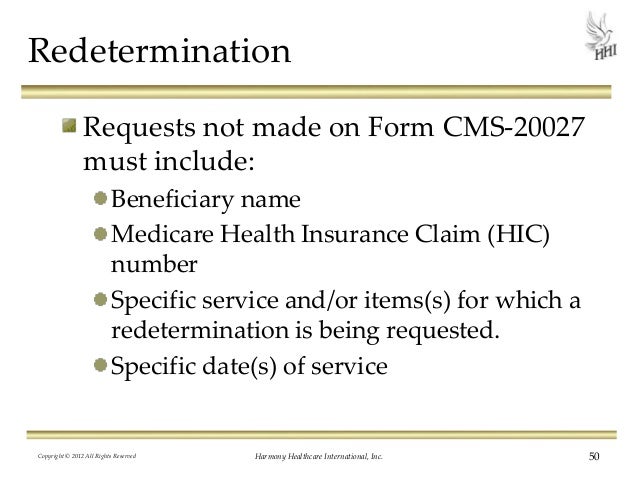
When must you file a redetermination?
When requesting a redetermination on an overpayment subject to the Recoupment Limitation provision, you must file the redetermination by Day 30 from the demand letter date to prevent recoupment on Day 41. If you file an appeal after Day 30 and by Day 120, the law requires your MAC to stop recoupment
Where do we refer overpayments to?
We refer the overpayment debt to the Treasury or to a Treasury-designated Debt Collection Center (DCC). Both work through the
Can Medicare overpayments be recouped?
outlines Medicare overpayment recoupment limitations. When CMS and MACs get a valid first- or second-level overpayment appeal, subject to certain limitations, we can’t recoup the overpayment until there’s an appeal decision. This affects recoupment timeframes. Get more information about which overpayments we subject to recoupment limitation at
Enrollment forms
I have Part A and want to apply for Part B (Application for Enrollment in Part B/CMS-40B).
Appeals forms
I want to appoint a representative to help me file an appeal (Appointment of Representative form/CMS-1696).
What is Medicare reimbursement form?
The Medicare reimbursement form, also known as the “Patient’s Request for Medical Payment, ” is available in both English and Spanish on the Medicare website.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What if my doctor doesn't bill Medicare?
If your doctor doesn’t bill Medicare directly, you can file a claim asking Medicare to reimburse you for costs that you had to pay.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
Does a waiver of recovery apply to a demand letter?
Note: The waiver of recovery provisions do not apply when the demand letter is issued directly to the insurer or WC entity. See Section 1870 of the Social Security Act (42 U.S.C. 1395gg).
Can Medicare waive recovery of demand?
The beneficiary has the right to request that the Medicare program waive recovery of the demand amount owed in full or in part. The right to request a waiver of recovery is separate from the right to appeal the demand letter, and both a waiver of recovery and an appeal may be requested at the same time. The Medicare program may waive recovery of the amount owed if the following conditions are met:
Does Medicare cover travel?
If you have Original Medicare and have a Medigap policy, it may provide coverage for foreign travel emergency health care. Learn more about Original Medicare outside the United States.
Can you voluntarily terminate Medicare Part B?
Voluntary Termination of Medicare Part B. You can voluntarily terminate your Medicare Part B (medical insurance). It is a serious decision. You must submit Form CMS-1763 ( PDF, Download Adobe Reader) to the Social Security Administration (SSA). Visit or call the SSA ( 1-800-772-1213) to get this form.
How much do you get back on a Medicare plan?
The amount you get back can range from $0.10 in some counties up to $148.50. Also, the amount you get back will depend on the options in your area. Further, sometimes the same plan name will have a different premium buy-down in different counties.
What is Medicare Part B give back?
Part B Premium Reduction Give Back Plans. The Medicare Part B give back plan, or premium reduction plan is a feature of Medicare Advantage. Yet, only some Medicare Advantage plans offer this benefit, and it isn’t available in all areas. Those with this plan may see a higher amount on their Social Security check, ...
What is a Part B premium reduction plan?
The Part B premium reduction plan is just like it sounds. You enroll in the policy, and the carrier pays either part or the whole premium for your outpatient coverage. In the summary of benefits or evidence of coverage , you’ll see a section that says Part B premium buy-down; this is where you can see how much of a reduction you’ll get.
How long does it take to get a Part B rebate?
It can take Social Security 1-3 months to begin your Part B premium rebate. After waiting, you can expect to see a regular increase in your checks.
Does Medigap cover Part B?
No, Medigap plans don’t cover Part B premiums because you need Part B to pay its portion of the claim. Medigap doesn’t replace Medicare.
Do you get reimbursed for Part B premium?
Beneficiaries are not reimbursed. You must pay the reduced premium amount. If your Part B premium comes out of your Social Security check, the reduced amount will reflect in your monthly check.
Can Medicare Advantage pay Part B?
The Medicare Advantage insurance company can pay either the whole or a portion of the Part B premium for enrollees. Since the Advantage plan handles your claim instead of Medicare, these plans make more sense than a standard Part C policy. How can Medicare Advantage plans give you back some of your Part B premium money?

When Do I Need to File A Claim?
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…