Does Medicare cover routine blood work?
Original Medicare (Medicare Part A and Part B) does not cover routine blood work as part of a general physical examination or screening. Did you know that there may be Medicare Advantage plans available where you live that can cover blood tests better than Original Medicare?
How do I know if my treatment requires approval from Medicare?
Refer to your plan documents, including the drug formulary, to see if your treatment requires approval. This information should be on your plan’s website. The Medicare & You handbook also contains more information. Your provider is responsible for requesting permissions.
How much do blood tests cost with Medicare?
Tests can run from a few dollars to thousands of dollars. That’s why it’s important to check that your test is covered before you have it done. Here are some of the blood test costs you can expect with the different parts of Medicare. In-hospital blood work ordered by your doctor is generally fully covered under Medicare Part A.
What services require prior approval from Medicare Advantage?
The services most often requiring prior approval are durable medical equipment, skilled nursing facility stays, and Part B drugs. But, each Advantage plan is different. If you have an Advantage plan, contact your plan provider to determine if or when prior authorization is necessary.

Does Medicare cover routine blood work?
Does Medicare Cover Blood Tests? Medicare covers medically necessary blood tests ordered by a physician based on Medicare guidelines. Medicare Advantage (Part C) plans may cover more tests, depending on the plan. There is no separate fee for blood tests under original Medicare.
Does Medicare require pre authorization?
Traditional Medicare, in contrast, does not require prior authorization for the vast majority of services, except under limited circumstances, although some think expanding use of prior authorization could help traditional Medicare reduce inappropriate service use and related costs.
How do I submit an authorization to Medicare?
To do so, you can print out and complete this Medicare Part D prior authorization form, known as a Coverage Determination Request Form, and mail or fax it to your plan's office. You should get assistance from your doctor when filling out the form, and be sure to get their required signature on the form.
How often can you get bloodwork with Medicare?
If a person has Medicare Part A and Part B, also known as Original Medicare, they can get a cholesterol screening every 5 years . The coverage is 100% as long as their doctor accepts Medicare. However, there may be a copayment for the doctor's visit. For some people, a doctor may recommend more frequent screenings.
What is the prior authorization process?
Prior authorization is a process by which a medical provider (or the patient, in some scenarios) must obtain approval from a patient's health plan before moving ahead with a particular treatment, procedure, or medication. Different health plans have different rules in terms of when prior authorization is required.
What does prior authorization required mean?
What is a Prior Authorization? A prior authorization (PA), sometimes referred to as a “pre-authorization,” is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine, medical device or procedure.
What services does not require prior authorization?
No pre-authorization is required for outpatient emergency services as well as Post-stabilization Care Services (services that the treating physician views as medically necessary after the emergency medical condition has been stabilized to maintain the patient's stabilized condition) provided in any Emergency Department ...
How long is a prior authorization good for?
A PA for a health care service shall be valid for a period of time that is reasonable and customary for the specific service, but no less than 60 days from the date the health care provider receives the PA, subject to confirmation of continued coverage and eligibility and to policy changes validly delivered.
Who is responsible for obtaining precertification for a referral to another physician or specialist?
The patientAkin to an official recommendation, referrals are made from one physician to another. The patient is usually responsible for obtaining the original referral from their doctor. Following the request, the physician may simply write a script for treatment that references a specific doctor, such as a specialist.
Does Medicare cover blood work at Labcorp?
Insured Patients Labcorp will file claims directly to Medicare, Medicaid, and many insurance companies and managed care plans. Before you have lab tests performed, please make sure: Your insurance information is up to date. Your insurance company accepts claims from Labcorp.
How often will Medicare cover a lipid panel?
Every 5 years, Medicare will cover costs to test your cholesterol, lipid, and triglyceride levels. These tests can help determine your risk level for cardiovascular disease, stroke, or heart attack.
Does Medicare use labcorp or quest?
Medicare covers tests performed at Quest, as long they're medically necessary and the specific facility accepts Medicare. Medicare Part B or Medicare Advantage (Part C) will cover the cost of your tests. Most tests will come at no cost to you once you've met your plan's deductible.
What part of Medicare covers blood tests?
If the blood test is ordered while receiving inpatient care at a hospital or skilled nursing facility, it will be covered under Medicare Part A (ho...
How much does a blood test cost?
If conducted in an inpatient care setting, the cost of the testing is subject to the Medicare Part A deductible, which is $1,364 per benefit period...
What blood tests are covered under Medicare?
Some of the more common types of blood tests that are covered by Original Medicare include Diabetes, Prostate cancer, Cardiovascular disease, Hepat...
Does Medicare Cover LabCorp or Quest?
Medicare covers medically necessary lab tests from LabCorp and Quest. These are two large laboratories that provide outpatient laboratory testing.
Why would my doctor order a blood test?
Blood tests help doctors check for specific diseases and conditions. They also help check the function of your organs and show how well treatments...
What Screening Laboratory Tests Does Medicare Cover?
Medicare covers several laboratory tests, providing a doctor deems the test medically necessary. This means a doctor is screening or looking for a...
What are some common blood tests and laboratory tests?
Blood tests and lab work are helpful to prevent disease, assess risk and diagnose illnesses. Medicare covers several types of tests as long as they...
How Often Does Medicare Pay for Blood Work?
Medicare pays for medically necessary blood work a doctor orders, as well as screening laboratory testing. Medicare may limit how often you can hav...
How Much Does Medicare Pay for Blood Work?
Providing the test is medically necessary and covered under Medicare, you will pay nothing for Medicare-approved services once you have met your Pa...
Does Medicare offer coverage for routine blood work?
Medicare covers “medically necessary” blood work. This means a doctor orders the test because they are trying to make a diagnosis. Routine blood wo...
Does Medicare Advantage cover blood tests?
Medicare requires that Medicare Advantage cover all the tests that Original Medicare does. However, Medicare Advantage plans can cover additional t...
Does Medicare Part B Cover Lab Tests?
Medicare Part B will cover medically necessary laboratory tests, provided your doctor orders the test, and a Medicare-approved lab runs the test. P...
What laboratory tests besides blood work does Medicare cover?
There are other laboratory tests besides blood tests that Medicare covers. Examples include urinalysis, which involves analyzing urine for the pres...
What is Medicare Part A?
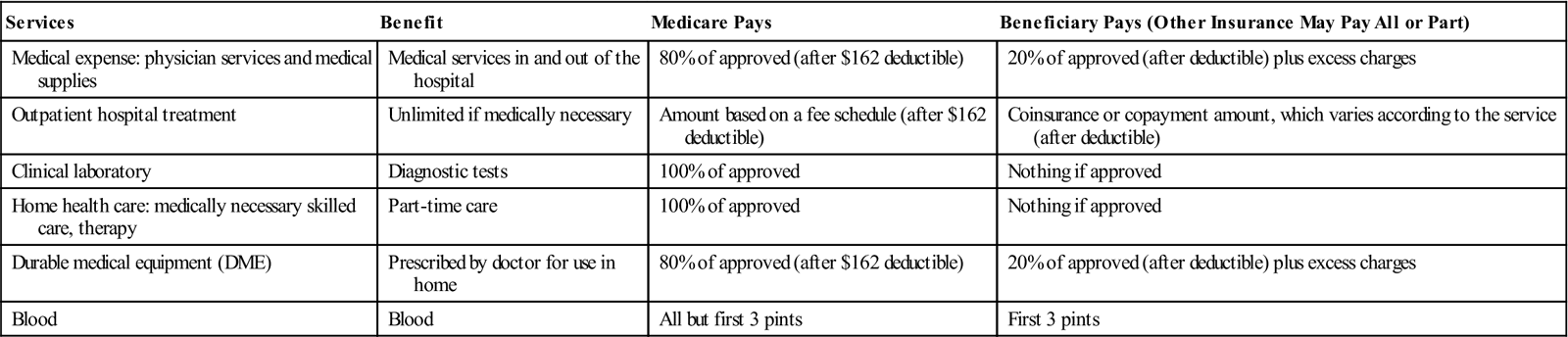
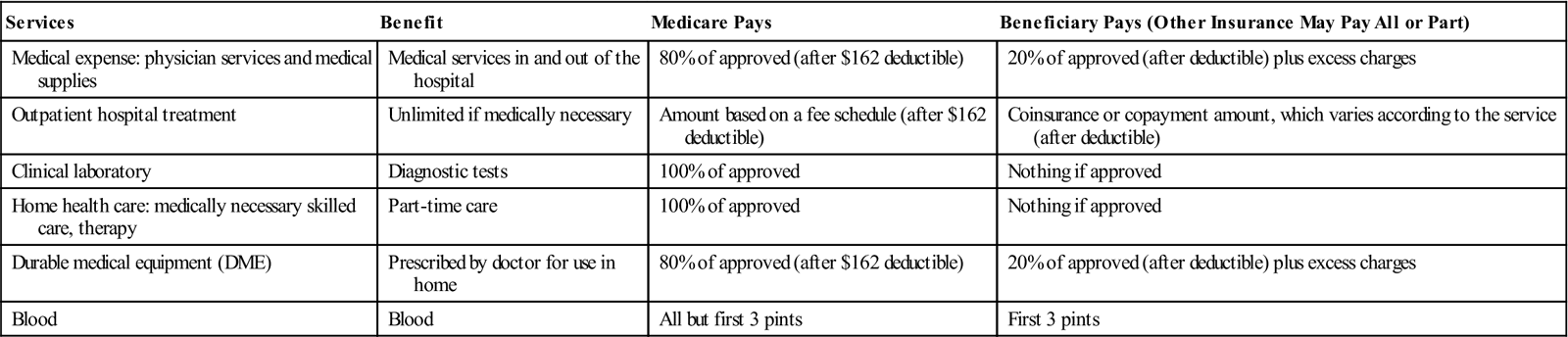
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
What is the purpose of blood test?
Blood tests are an important diagnostic tool doctors use to screen for risk factors and monitor health conditions. A blood test is generally a simple procedure to measure how your body is functioning and find any early warning signs. Medicare covers many types of blood tests. Trusted Source.
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
Does Medicare cover ABN?
Medicare offers a tool you can use to check which tests are covered. You can also go here to look through the list of covered tests from Medicare. You can look through lists of codes and items Medicare does not cover. Before signing an ABN, ask about the cost of the test and shop around.
Does Medicare Advantage cover blood work?
Medicare Advantage, or Part C, plans also cover blood tests. These plans may also cover additional tests not covered by original Medicare (parts A and B). Each Medicare Advantage plan offers different benefits, so check with your plan about specific blood tests. Also consider going to in-network doctors and labs to get the maximum benefits.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
Does Medicare require prior authorization?
Medicare Part A Prior Authorization. Medicare, including Part A, rarely requires prior authorization. If it does, you can obtain the forms to send to Medicare from your hospital or doctor. The list mostly includes durable hospital equipment and prosthetics.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Does Medicare cover CT scans?
If your CT scan is medically necessary and the provider (s) accept (s) Medicare assignment, Part B will cover it. Again, you might need prior authorization to see an out-of-network doctor if you have an Advantage plan.
What blood tests are covered by Medicare?
Some of the more common types of blood tests that are covered by Original Medicare include: Diabetes – Two screenings per year with a referral or by meeting qualifying risk factors (blood sugar test strips for people with diabetes are also covered by Part B) Prostate cancer – One screening per year as recommended by a doctor.
How much is a blood test for Medicare 2021?
The cost of the blood test will be applied to your annual Part B deductible, which is $203 in 2021. If the laboratory is not Medicare-approved, there may also be a coinsurance payment required by the beneficiary. A Medicare Supplement Insurance plan (also called Medigap) can help cover some of the cost of blood tests by providing coverage ...
Does Medicare cover blood work?
Original Medicare does cover blood tests when they are ordered by a doctor or other health care professional to test for, diagnose or monitor a disease or condition. The blood test must be deemed medically necessary in order to be covered by Medicare. Original Medicare (Medicare Part A and Part B) does not cover routine blood work as part ...
Does Medicare Cover LabCorp or Quest?
Medicare covers medically necessary lab tests from LabCorp and Quest. These are two large laboratories that provide outpatient laboratory testing.
What Screening Laboratory Tests Does Medicare Cover?
Medicare covers several laboratory tests, providing a doctor deems the test medically necessary. This means a doctor is screening or looking for a particular condition.
How Often Does Medicare Pay for Blood Work?
Medicare pays for medically necessary blood work a doctor orders, as well as screening laboratory testing. Medicare may limit how often you can have these tests and the amount they pay. Examples include:
How Much Does Medicare Pay for Blood Work?
Providing the test is medically necessary and covered under Medicare, you will pay nothing for Medicare-approved services once you have met your Part B deductible. For 2022, the Part B deductible is $233.
Does Medicare Part B Cover Lab Tests?
Medicare Part B will cover medically necessary laboratory tests, provided your doctor orders the test, and a Medicare-approved lab runs the test. Part B is the Medicare portion that covers medical services, including doctor’s visits.
How often does Medicare cover fecal occult blood test?
Fecal occult blood test. Medicare covers a fecal occult blood test once every 12 months for people aged 50 years or above. The test checks for blood in the stool that a person cannot see with the naked eye. If the result is positive, it may indicate that some part of the digestive tract is bleeding.
How often does Medicare cover a Pap?
Pap test. Medicare generally covers Pap tests every 2 years for females , though some situations may require more frequent tests. For example, if a person had an abnormal Pap test in the previous 3 years and is of child-bearing age or at high risk of certain cancers, Medicare covers a Pap test once per year.
What is Medicare Advantage?
Medicare Advantage, or Medicare Part C, offers an alternative to Medicare parts A, B, and D. Medicare Advantage consists of Medicare-approved, private insurance companies that must follow the guidelines and rules of Medicare. Like parts A and B, Medicare Advantage plans cover the costs of blood work and other tests.
What is a coinsurance for Medicare?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is the BMP test?
The blood chemistry test, also called a Basic Metabolic Panel (BMP), usually measures components of the fluid portion of the blood. These measurements give doctors information about how the muscles, bones, and certain organs, such as the kidneys, are working.
What is a complete blood count?
A complete blood count helps detect clotting problems, immune system disorders, blood cancers, and blood disorders such as anemia. It measures: red blood cells, which transport oxygen to all parts of the body. white blood cells, which fight infections. platelets, which are the fragments that enable the blood to clot.
Does Medicare cover blood work?
In some cases, Medicare Part A will cover the costs of blood work. Typically, a hospital or care facility will bill Part A when the person is staying within the facility. Medicare consists of three main parts: Part A: This is hospitalization insurance, which covers blood tests and other diagnostic laboratory tests that a doctor orders ...
What is prior authorization in Medicare?
Medicare Prior Authorization. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service. Prior Authorization is about cost-savings, not care. Under Prior Authorization, benefits are only paid if the medical care has been pre-approved by Medicare.
Do Medicare Advantage plans require prior authorization?
Private, for-profit plans often require Prior Authorization. Medicare Advantage (MA) plans also often require prior authorization to see specialists, get out-of-network care, get non-emergency hospital care, and more.
What is pre claim review?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submitting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical ...
What is CMS in Medicare?
The Centers for Medicare & Medicaid Services (CMS) runs a variety of programs that support efforts to safeguard beneficiaries’ access to medically necessary items and services while reducing improper Medicare billing and payments. Through prior authorization and pre-claim review initiatives, CMS helps ensure compliance with Medicare rules.