
What happens to my Medicare card if I join an advantage?
You will know if you have Original Medicare or a Medicare Advantage plan by checking your enrollment status. Your enrollment status shows the name of your plan, what type of coverage you have, and how long you’ve had it. You can check your status online at www.mymedicare.gov or call Medicare at 1-800-633-4227. Continue Learning about Medicare
How do I join a Medicare Advantage plan?
Nov 29, 2021 · Fill out the requested information, including your zip code, Medicare number, name, date of birth and your effective date for Medicare Part A coverage or Part B coverage. Click “Continue,” and you should be taken to a page that shows the the coverage that you have. If you just recently enrolled, it may not be immediately reflected online.
How do I know if I have Medicare or Medicare Advantage?
The best way to find out if one has Medicare is to apply. The main websites for Medicare and Social Security have short and simple online application pages. One can apply and get an official answer very quickly. The sites state the qualifications needed, and they process moves quickly for most applicants. The Medicare system requires choices.
How do Medicare Advantage plans work?
If you join a Medicare Advantage Plan, you’ll still have Medicare but you’ll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. You must use the card from your Medicare Advantage Plan to get your Medicare-covered services. Keep your red, white and blue Medicare card in a safe place
What is the difference between Medicare and a Medicare Advantage Plan?
Medicare Advantage is an “all in one” alternative to Original Medicare. These “bundled” plans include Part A, Part B, and usually Part D. Plans may have lower out-of- pocket costs than Original Medicare. In many cases, you'll need to use doctors who are in the plan's network.
What defines a Medicare Advantage Plan?
Medicare Advantage is a type of Medicare health plan offered by private companies that are Medicare-approved. They are considered an alternative to Original Medicare and cover all the expenses incurred under Medicare. They include the same Part A hospital and Part B medical coverage, but not hospice care.
What is the biggest difference between Medicare and Medicare Advantage?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.Oct 1, 2020
What are 4 types of Medicare Advantage plans?
Medicare Advantage PlansHealth Maintenance Organization (HMO) Plans.Preferred Provider Organization (PPO) Plans.Private Fee-for-Service (PFFS) Plans.Special Needs Plans (SNPs)
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
Can you switch back and forth between Medicare and Medicare Advantage?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
What are the disadvantages of a Medicare Advantage plan?
Cons of Medicare AdvantageRestrictive plans can limit covered services and medical providers.May have higher copays, deductibles and other out-of-pocket costs.Beneficiaries required to pay the Part B deductible.Costs of health care are not always apparent up front.Type of plan availability varies by region.More items...•Dec 9, 2021
Is Medicare Advantage cheaper than original Medicare?
The costs of providing benefits to enrollees in private Medicare Advantage (MA) plans are slightly less, on average, than what traditional Medicare spends per beneficiary in the same county. However, MA plans that are able to keep their costs comparatively low are concentrated in a fairly small number of U.S. counties.Jan 28, 2016
What are the benefits of Medicare Advantage?
Most Medicare Advantage plans offer additional benefits not covered by Original Medicare, such as dental, vision and prescription drug coverage. Medicare Part D provides coverage for prescription medications, which is something not typically covered by Original Medicare.
How long does Medicare AEP last?
The Medicare AEP lasts from October 15 to December 7 every year. During this time, Medicare beneficiaries may do any of the following: Change from Original Medicare to a Medicare Advantage plan. Change from Medicare Advantage back to Original Medicare. Switch from one Medicare Advantage plan to another.
What is an annual review of Medicare?
An annual review of your Medicare coverage can help you determine if your plan combination is right for your needs. For example, if you’re spending a considerable amount of money on prescription drugs, a Medicare Part D plan or a Medicare Advantage plan with prescription drug coverage may be something to consider.
What is Medicare Part B?
Medicare Part B is medical insurance and provides coverage for outpatient appointments and durable medical equipment. Part B is optional, but is required for anyone wanting to enroll in Medicare Part C, Part D or Medicare Supplement Insurance. Part A and Part B are known together as “Original ...
Is Medicare Part A and Part B the same?
Part A and Part B are known together as “Original Medicare.”. Medicare Part C, also known as Medicare Advantage, provides all the same benefits as Medicare Part A and Part B combined into a single plan sold by a private insurance company.
What is Medicare.gov?
Medicare is the agency that runs Medicare. It has many regional contractors that support the systems for payments, processing claims, and durable medical equipment. It oversees the performance of private insurance providers that sell Medicare Advantage, Medigap, and Prescription Drug plans. Medicare.gov is the ideal place to find ...
What is comparison shopping in Medicare?
Comparison shopping is the ideal tool for making selections of private health, prescription drug, and gap insurance plans.
What is Medicare and Social Security?
Medicare and Social Security provide tools for determining eligibility and benefits. Medicare is the national health care program for older Americans. The start date for Medicare coverage is important; many other features depend on the date of enrollment. Medicare has four parts that cover hospital insurance, medical insurance, ...
How long does it take to get Medicare referrals?
Recipients under age 65 get an automatic referral for Medicare after 24 months of payments. Persons with end-stage renal disease or ALS get automatic eligibility when diagnosed.
How old do you have to be to get Medicare?
Medicare has four parts that cover hospital insurance, medical insurance, private all-in-one plans, and prescription drug benefits. Everyone age 65 or older can get Medicare. Disabled persons can get it while under age 65. Those who paid FICA taxes for ten years can get premium-free Medicare.
How long is the initial enrollment period for Medicare?
The Initial Enrollment Period is the seven-month period that includes the month of the 65th birthday. The period runs from three months before the birthday month, and for three months afterward . This is the ideal time to review options and make choices for Medicare coverage.
Does Medicare have gap insurance?
Medicare has private insurance plans for health, prescription drugs, and gap insurance. Comparison shopping is an excellent method for finding the best fit. Comparison shopping is an excellent method for finding the best fit. Find and compare private Medicare health plans for free by entering your zip code above!
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
Can't offer drug coverage?
Can’t offer drug coverage (like Medicare Medical Savings Account plans) Choose not to offer drug coverage (like some Private Fee-for-Service plans) You’ll be disenrolled from your Medicare Advantage Plan and returned to Original Medicare if both of these apply: You’re in a Medicare Advantage HMO or PPO.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What is Medicare Part A?
Parts of Medicare. Part A – Covers time spent in a health facility such as a hospital, hospice care, or home health agency. Part B – Covers health expenses such as doctor visits, surgery, medical supplies, lab work, and test screenings. Part C – A combination of Part A and B that can also include dental, vision, prescriptions, ...
How do I know if I have medicaid?
The best way to know which one you have is to call the number on the back of your insurance card.
What is QMB in Medicare?
Qualified Medicare Beneficiary Only (QMB) is a Medicaid-funded program that provides financial assistance to cover Medicare Part A and Part B premiums. It also covers Medicare deductibles, coinsurances, and copays.
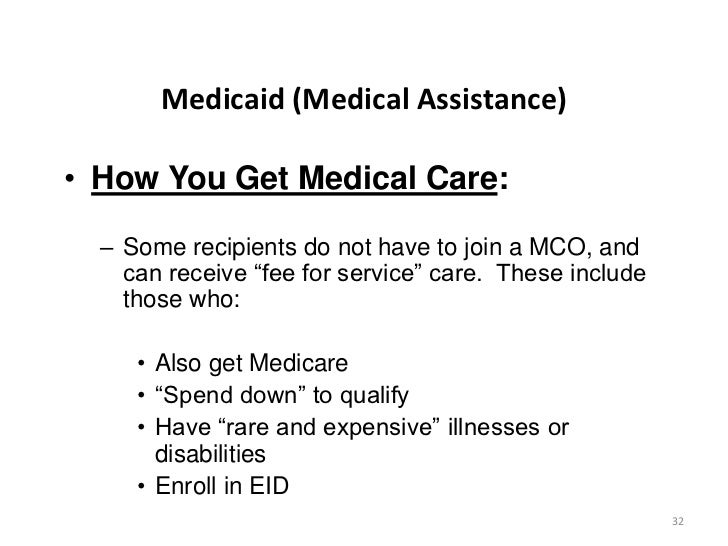
What is managed care plan?
Managed Medicaid (Managed Care Plan) – The state contracts with a private insurance company to manage and administer Medicaid benefits. Member benefits will be similar to fee-for-service, but could vary depending on the plan.
What is Medicaid in the US?
Medicaid is a health program provided by individual state governments to people who meet at least one of the income or disability requirements. Nobody is automatically enrolled in Medicaid. To receive it, you must apply through your state’s Medicaid office.
What are the two types of medicaid?
There are two basic types of Medicaid: Fee-For-Service and Managed Medicaid. Fee-For-Service – Medicaid pays doctors, hospitals, and other healthcare providers for the individual services or products received by the Medicaid member. Managed Medicaid (Managed Care Plan) – The state contracts with a private insurance company to manage ...
How many parts are there in Medicare?
About Medicare. Medicare is a national health program provided by the US government. It’s divided into 4 parts: Part A, Part B, Part C, and Part D. Every American who paid into Medicare is automatically enrolled in Part A and Part B when they turn 65. People under 65 with certain disabilities may also apply to enroll.
What is Medicare Advantage?
Medicare Advantage (MA), also known as Medicare Part C, are health plans from private insurance companies that are available to people eligible for Original Medicare (Medi care Part A and Medicare Part B).... work. In this MedicareWire article, we’ll explain what you need to know to stay out of trouble.
When will Medicare Advantage be available in 2021?
May 6, 2021. If you have ever had a Health Maintenance Organization (HMO) plan or a Preferred Provider Organization (PPO) plan through an employer or the Healthcare Exchange, you already have a pretty good idea about how Medicare Advantage plans. Medicare Advantage (MA), also known as Medicare Part C, are health plans from private insurance ...
How many types of Medicare Advantage Plans are there?
Currently, there are seven types of Medicare Advantage plans: HMO — HMOs deliver care through a network of doctors, hospitals, and other medical professionals that you must use to be covered for your care. PPO — PPO plans have provider networks, like HMOs.
What do you need to use for Medicare supplement?
It’s worth mentioning that when you have a Medicare supplement, you need to use healthcare providers that are approved by Medicare. This includes hospitals, nursing facilities, home health agencies, hospice care, and doctors. Most primary care doctors accept Medicare patients.
What is the CMS rating system?
The Centers for Medicare & Medicaid. Medicaid is a public health insurance program that provides health care coverage to low-income families and individuals in the United States.... Services (CMS) grades each plan annually with a 5-star rating system making it easier to compare Medicare Advantage plans in your area so you can find ...
Does Medicare Advantage cover the same as Medicare?
Key Takeaways. Medicare Advantage plans must cover the same benefits as Original Medicare. Original Medicare is private fee-for-service health insurance for people on Medicare. It has two parts. Part A is hospital coverage. Part B is medical coverage.... , but how they cover the benefits may be different.
Can Medicare Supplements be added to Medicare Advantage?
For this reason, Medicare supplements can’t offer additional benefits. They are strictly an insurance plan to pick up the gap in coverage in Medicare’s traditional fee-for-service system. However, private insurance companies that offer Medicare Advantage plans can bundle extra benefits.
How much does Medicare Advantage pay for doctor visits?
Medicare Advantage enrollees usually pay a copayment when they get healthcare. This is usually between $10 and $20 for doctor visits and up to $75 for emergency room and urgent care visits. There is often a tiered copayment system for prescription drugs.
What is the difference between Medicare Advantage and Original?
There is one very important difference between Original Medicare vs Medicare Advantage, however. Medicare Advantage plans have a maximum out-of-pocket limit or MOOP. Once you hit your MOOP, you pay nothing for covered healthcare for the rest of that calendar year.
What is the MOOP for Medicare Advantage 2021?
In 2021, the mandatory MOOP for Medicare Advantage is $7,550, although many plans choose to set theirs much lower. In 2021, only about 20% of Medicare Advantage had the mandatory MOOP of $7,550. This means that many plans offer a lower MOOP, which is good for you.
Why is it so hard to give a snapshot of your Medicare Advantage plan?
It’s difficult to give a snapshot of your costs with a Medicare Advantage plan because each one is different . Each company that offers a plan can choose what to charge for premiums, deductibles, and copayment amounts.
How much is a MOOP with Medicare?
Some people like the security of a MOOP with Medicare Advantage. However, even with a MOOP below $7,550, you’d have some heavy spending before you reach that cap.
What are the two parts of Medicare?
Original Medicare benefits include two parts, Part A and Part B , that provide your hospital and medical insurance. If you have a qualifying work history, your Part A benefits are premium-free. Medicare Part B premiums are set each year by the federal government and most people pay the same standard rate.
Is Medicare deductible in 2021?
This article has been updated for 2021. For many people, costs are a major concern when it comes to choosing your health insurance. Besides premiums, there are deductibles, coinsurance, and copayments to consider in calculating your total Medicare spending.
How to disenroll from Medicare Advantage?
Visit your local Social Security Office and ask to be disenrolled from Medicare Advantage ; Call 1-800-MEDICARE (1-800-633-4227) and process your disenrollment over the phone; or. Contact your Medicare Advantage insurer directly and request a disenrollment form.
How long can you switch to Medicare Advantage?
If you wait to tell your Medicare Advantage plan about your move, then you can switch to Original Medicare for up to two full months after the month that you inform your plan.
What is Medicare Supplement Plan?
This kind of plan, also known as a Medigap policy, pays for gaps in Medicare’s coverage. For instance, Medicare Part B pays 80% of covered costs after you pay your annual deductible. A Medigap policy would pay the remaining 20% ...
How long does it take to switch from Medicare Advantage to Original Medicare?
If you’re covered by both Medicare and Medicaid and then you lose eligibility for Medicaid, you can switch from Medicare Advantage to Original Medicare up to three months from the date you lose Medicaid eligibility, or the date you’re notified, whichever is later.
When does Medicare open enrollment end?
Medicare Advantage Open Enrollment Period. This special opportunity to leave Medicare Advantage lasts from January 1 through March 31 each year. If you disenroll during January, your changes will be effective on February 1. If you disenroll during February, your changes will be effective on March 1. If you disenroll during March, your changes will ...
What are institutional care facilities?
Facilities that qualify as institutional care include: 1.) long-term hospitals, 2.) skilled nursing facilities (SNFs), 3.) rehabilitation hospitals and units, 4.) psychiatric hospitals and units, 5.) care facilities for the intellectually disabled, and 6.) and swing bed hospitals. You can move from Medicare Advantage to Original Medicare ...
Can you switch to Original Medicare if you are eligible for medicaid?
If You Become Eligible for Medicaid. Once you become eligible for Medicaid benefits, then you can drop your Medicare Advantage plan and switch to Original Medicare. While you’re covered under Medicare and Medicaid, you can change that coverage once a quarter during the first three quarters of the year ...
