Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
How do I get Medicaid or Medicare?
Feb 11, 2022 · For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses.
What does Medicaid pay for?
Nov 18, 2021 · There are several ways that low-income people with both Medicare and Medicaid benefits can get extra help with their prescriptions. The first and most important way is to apply for the Social Security Administration’s Extra Help program. This program provides low-income subsidies ( LIS ) to those who need them.
Does Medicaid pay for Medicare Part A?
Feb 10, 2020 · Medicaid can give you assistance in paying your Medicare premiums. In most instances, if you have dual coverage through Medicare and Medicaid, you’ll automatically enroll in a Medicare Savings Program (MSP). These savings programs will pay for your Medicare Part B premium cost, and they can offer additional payment assistance in other areas. Cost Sharing …
How do I combine Medicare and Medicaid benefits?
Nov 13, 2018 · Depending on your finances, you could qualify to become what is called a “dual eligible,” someone who can enroll in both Medicare and Medicaid. Even if your income is not low enough for you to qualify for full Medicaid benefits, you may be eligible for one of the four Medicare Savings Programs that can help you pay for all or some of those costly out-of-pocket …

How are Medicare premiums paid?
Premiums are typically paid on a monthly basis. In the federal Medicare program, there are four different types of premiums. ... , deductibles, copays, and more. Medicaid assists with these costs, but you may be required to use an approved Medicaid health plan.
What is the difference between Medicare and Medicaid?
The benefit is the plan will have very low copays and very few additional fees. Medicare is for those aged 65 and older or those with disabilities or specific medical conditions. Medicaid is for people of any age, with or without medical conditions, so long as they meet the state’s economic conditions.
What percentage of Medicare beneficiaries are eligible for Medicaid?
Around 20 percent of Medicare beneficiaries are also eligible for Medicaid. They are called dual-eligible. You would need to apply for each one separately to determine if you can qualify for both. Dual-eligibles are categorized based on whether they receive full or partial Medicaid benefits.
What percentage of Medicare is covered by deductible?
In fact, from the beginning, Medicare was designed to cover only about 80 percent of a beneficiary’s major medical expenses. All other costs, typically in the form of deductibles. A deductible is an amount a beneficiary must pay for their health care expenses before the health insurance policy begins to pay its share....
What is Medicare Part B?
If not, you will pay a monthly premium for Part A. With Part B. Medicare Part B is medical coverage for people with Original Medicare. It covers doctor visits, specialists, lab tests and diagnostics, and durable medical equipment. Part A is for hospital inpatient care....
How can low income people get help with prescriptions?
The first and most important way is to apply for the Social Security Administration’s Extra Help program . This program provides low-income subsidies (LIS) to those who need them.
How old do you have to be to get Medicare?
Since Medicare is a government insurance program, anyone aged 65 or older can apply and receive insurance through this program.
What is the difference between Medicare and Medicaid?
When you have dual enrollment, Medicare is your primary insurance that covers any costs first. Medicaid is your secondary payer. Every state has different benefits for people who qualify under dual eligibility, so it’s important that you check with your local Medicaid office.
Does Medicaid cover dental care?
Medicaid can cover a large variety of healthcare services like behavioral health for substance abuse and mental health or dental care. Medicaid also has a robust cost-sharing program that helps cover any out of pocket costs for economically disadvantaged participants.
Can seniors get medicaid?
Many seniors in the United States have dual eligibility for Medicare and Medicaid benefits. Generally, this means that you have enrolled in Medicare, but that you qualify for Medicaid as well due to your income.
Is Medicaid a secondary insurance?
Secondary Insurance. Medicaid can fill in the gap as a secondary insurance to Medicare. Any services you have that Medicare pays for like hospital care, doctor’s visits, skilled nursing facility care, or home care, Medicare will pay for as the primary payer.
Does Medicaid pay cost sharing?
Medicaid can pay any cost-sharing charges you have. This help will depend on your income level. If the level is low enough, you could qualify for the Qualified Medicare Beneficiary (QMB) Medicare Savings Program. If you enroll in QMB, you won’t have to pay Medicare cost-sharing fees.
Does Medicare help with prescription drugs?
Prescription drugs are some of the biggest expenses people on Medicare face, and Medicaid can help. People who meet the eligibility requirements for dual enrollment in Medicare and Medicaid automatically get enrolled in the Extra Help program.
How much is Medicare Part A deductible?
The Medicare Part A (hospital insurance) deductible, which for 2019 will be $1,364 for hospital stays. Both Medicare Part A and Part B copays and coinsurance. The Medicare Part D premium, deductibles and copays for prescription drugs. Coverage for those costs is available through the Extra Help program, which Medicaid and Medicare Savings Program ...
Who can answer Medicaid questions?
SHIP counselors can answer some of your Medicaid questions and refer you to local Medicaid officials to help with others. The National Council on Aging has a benefits checkup website that has information on Medicare, Medicaid and other programs that help older Americans.
What is QDWI in Medicare?
The Qualified Disabled and Working Individuals (QDWI) program only helps pay for Medicare Part A (hospital insurance) premiums. This program is designed for individuals with disabilities, under age 65, who are currently working and lost their premium-free Part A benefit when they began to work.
Does Medicare cover dual eligible?
While there are some national eligibility and benefit requirements, each state has its own Medicaid eligibility standards and decides which optional services it will cover and how much it is willing to pay for health care that Medicare doesn’t cover. Here’s what you need to know about the dual eligible programs:
Does Medicaid cover nursing home care?
Nursing home care and home- and community-based long-term services and supports. In some states, Medicaid will cover benefits that Medicare does not , such as dental care, transportation to and from doctor visits, eyeglasses, physical therapy and other services.
Does full medicaid have higher thresholds?
As with full Medicaid, some states have higher resource thresholds. Casey Schwarz at the Medicare Rights Center says that “one of the biggest problems we see is that people assume they aren’t eligible and don’t apply. People should look into what the income and asset guidelines are for their state.”.
Can I qualify for extra help for prescription drugs?
You also automatically qualify for Extra Help for prescription drugs. The Qualifying Individual (QI) program only helps pay for Part B premiums and no other cost sharing. If your income is too high for you to qualify for the QMB or SLMB programs, you might qualify for the QI program.
How much is Medicare Part A deductible?
Medicare Part A, which pays for hospitalizations and inpatient care, has a $1,288 deductible in 2016 plus co-insurance costs for stays exceeding 60 days. Those who want outpatient care, covered by Part B, have additional deductible and coinsurance costs, plus they typically pay a $104.90 premium each month.
What is a qualified Medicare beneficiary?
Qualified Medicare beneficiary. Offering the highest level of coverage, these beneficiaries may pay for Part A and Part B premiums, deductibles, co-insurance and co-pay ments. Specified low-income Medicare beneficiary. People in this category receive Medicaid coverage for their Part B premiums. Qualifying individual.
Does Medicare Advantage have supplemental services?
Medicare Advantage plans that offer supplemental services may have higher premiums, but Medicaid beneficiaries don't pay extra for a managed care plan.
Do you have to apply for medicaid once?
What's more, while Medicare beneficiaries only have to apply for benefits once, most Medicaid programs require recipients to submit documentation on a regular basis to remain eligible. There are several levels of Medicaid coverage. Not everyone who is eligible for Medicaid will get the same level of coverage.
Can you get Medicaid with limited income?
Those with limited income and assets may be eligible for Medicaid to pay the monthly premium and other out-of-pocket costs associated with Medicare. Here are five things you should know about getting dual coverage. [See: 10 Things You Need to Know About Medicare .] Your Medicaid and Medicare eligibility is determined separately.
Can seniors apply for medicaid in advance?
Seniors and their relatives may want to contact their state's social services department in advance to learn more about Medicaid eligibility requirements. Then, when and if a person reaches that income and asset level, an application can be submitted to begin benefits as quickly as possible.
Is Medicare and Medicaid separately determined?
Your Medicaid and Medicare eligibility is determined separately. The first thing to understand is that Medicaid and Medicare eligibility and enrollment are handled separately. "Everyone who is eligible for retirement [Social Security benefits] is entitled to Medicare," says Ginalisa Monterroso, CEO of Medicaid Advisory Group.
Who are the dual-eligible recipients?
People who are dual-eligible for Medicare and Medicaid are referred to as dual-eligible beneficiaries. Moreover, each state determines Medicaid coverage, and as a result, Medicaid benefits may differ.
Medicare Ineligibility
The Medicare eligibility requirement is that you must be 65 years old or older. If you or your spouse are 65 years old or older and have paid enough Medicare taxes through previous employment, you or your spouse may be eligible for premium-free Part A of the Medicare program (hospital coverage).
Medicaid Ineligibility
Medicaid eligibility varies depending on where a person resides, as various states have different qualifications.
Dual eligibility
A person must qualify for either partial-dual or full-dual coverage to be eligible for both Medicare and Medicaid.
Variations in geography
Medicaid benefits and coverage vary from one state to the next, and there are differences between them. Depending on the state, Medicaid coverage may be available to those who earn more than the standard income limits.
Medicare Part D Extra Assistance Program
Aside from Medicaid, many other programs assist with medical expenses, and government sponsors them. Extra Help, a program that assists Medicare Part D enrollees with their prescription drug costs, can be applied for by a qualified individual.
Summary
A person’s health and income level may qualify them for both Medicare and Medicaid.
What is Medicaid insurance?
Medicaid is a health insurance program providing financial assistance to individuals and families with a low income or limited financial resources. The federal government sets rules and regulations regarding Medicaid, and individual states are responsible for operating Medicaid programs.
How many people are dually eligible for medicaid?
If a person qualifies for both, the government refers to them as dually eligible. An estimated 12 million people in the United States are dually eligible for Medicare and Medicaid, according to Medicaid.gov. In this article, we discuss eligibility for Medicare and Medicaid, as well as what to know about each program.
What is dual eligible for medicaid?
Dual-eligible beneficiaries are people who have both Medicare and Medicaid. Each state is responsible for determining Medicaid coverage, and, as such, Medicaid benefits may vary. Receiving both Medicare and Medicaid can help decrease healthcare costs for those who are often most in need of treatment. As a general rule, Medicare will usually first ...
What is the age limit for Medicare?
Medicare. Medicare is an insurance plan for people at or over the age of 65 and for others with qualifying medical concerns. A person must meet eligibility criteria based on their work history or that of their spouse. They can qualify for premium-free hospital coverage and pay a premium for medical and prescription drug coverage.
How often does medicaid change?
Medicaid standards can change every year. If a person was unsuccessful in a prior application, they might qualify at a later date. One of the most important factors for Medicaid eligibility is where a person falls on the Federal Poverty Level (FPL).
How old do you have to be to qualify for Medicare?
Eligibility for Medicare. The usual way to qualify for Medicare is to be 65 years of age. A person can receive premium-free Part A (hospital coverage) benefits if they or their spouse is 65 or older and has paid sufficient Medicare taxes through previous employment.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
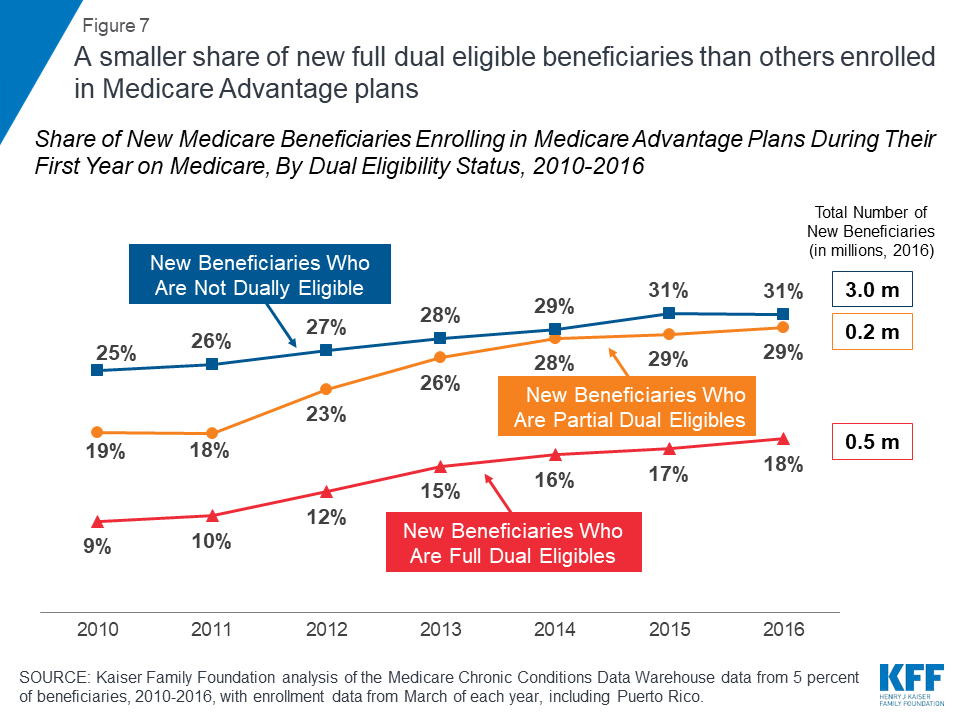
What is dual eligible Medicare?
Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (12.1 million people). Dual eligibles are categorized based on whether they receive partial or full Medicaid benefits. Full-benefit dual eligibles have comprehensive Medicaid coverage, ...
Does Medicare cover long term care?
But this is not the case for things Medicare doesn’t cover, like long-term care . If Medicaid is covering a beneficiary’s long-term care, Medicare will still be the primary payer for any Medicare-covered services – like skilled nursing care or physical therapy.
Do seniors qualify for medicaid?
Many seniors who live in nursing homes are dual eligible: they qualify for Medicare based on their age, and Medicaid because of their financial circumstances.
Is Medicare the same as Medicaid?
The federal government oversees Medicare eligi bility – meaning it is the same in each state. But states set their own eligibility rules for Medicaid and the MSPs (within federal guidelines) – and income limits for these programs vary widely.
Who can receive medicaid?
Others besides seniors can receive Medicaid benefits In all states, Medicaid provides health coverage for some low-income people, families and children, pregnant women, the elderly, and people with disabilities. In some states the program covers all low-income adults below a certain income level. People with a disability or certain medical ...
What is the funding source for medicaid?
Medicaid has two funding sources: the state and the federal government. Therefore, the money to operate Medicaid is split between the federal government’s contribution and the taxes a state collects. Keep in mind that annual income limits for Medicaid are indexed to the federal poverty level.
What is QMB in medicaid?
Qualifying Medicaid Beneficiary (QMB) Only. This is for people who are not eligible to receive full Medicaid benefits. Medicaid will pay the recipient’s Medicare Part A premiums (if any). It will also pay their Medicare Part B premium for them.
What is the maximum amount of money you can make on Medicare in 2021?
QI is another category in which Medicaid will only pay your Medicare Part B premium. In 2021, the maximum monthly income is $1,469 for an individual and $1,980 for a couple. For 2021, QI recipients, the maximum asset level allowed is $7,970 for an individual and $11,960 for couples.
What is the maximum income for Medicare Part B 2021?
If you’re an SLMB recipient, Medicaid will pay your Medicare Part B premium. In 2021, the maximum monthly income is $1,308 for an individual and $1,762 for a couple. For 2021, the maximum asset level is $7,970 for an individual and $11,960 for a couple.
How much is Medicare Part B in 2021?
Everybody must pay a Medicare Part B premium of $148.50 monthly in 2021, regardless of income. Can’t afford it? If you qualify for Medicaid, it may pay the premium for you.
What is the income limit for Medicaid in 2021?
In 2021, the limit in the continental U.S. was $12,880 for an individual and $17,420 for a couple.