To be eligible for Medicaid Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…Medicaid
- Pregnant, or.
- Be responsible for a child 18 years of age or younger, or.
- Blind, or.
- Have a disability or a family member in your household with a disability, or.
- Be 65 years of age or older.
How to verify eligibility of Medicaid plan members in Florida?
eligibility for these recipients. Providers can check eligibility for the displaced Florida Medicaid recipients that are being serviced by calling the Florida Medicaid Automated Voice Response System (AVRS) at the following phone number: 1-800-239-7560. The AVRS requires the use of a nine-digit active Florida Medicaid provider identification (ID) number to verify recipient eligibility. Providers servicing displaced Florida Medicaid recipients who do
What are the rules for Medicaid in Florida?
Florida Medicaid Eligibility Requirements
- Medicaid Basics. Medicaid is a federal and state program designed to supplement the income of persons who need medical and/or nursing home treatment.
- Basic Medicaid Eligibility. ...
- Income Requirements for Florida Residents. ...
- Florida Codes and Legal Research Options
- Talk to an Experienced Attorney About Medicaid Eligibility. ...
What is the age requirement for Medicaid in Florida?
- Low-income families (must care for a child age 18 and under)
- Pregnant women
- Children
- Individuals receiving disability benefits
What are the qualifications for Florida Medicaid?
Lawmakers also advanced a measure altering step therapy rules. On Monday, a House health care panel quickly approved bills that expand Florida’s telehealth law, delete certain reporting ...
Who is eligible for Medicare and Medicaid in Florida?
Be legal Florida residents, Be a minimum of 65 years of age OR between 18 and 64 years old and designated as disabled by the Social Security Administration, Need “nursing facility level of care”, and. Meet the financial requirements for Florida Medicaid.
What is the income level to qualify for Medicaid in Florida?
Effective Jan 1, 2022, the applicant's gross monthly income may not exceed $2,523.00 (up from $2,382.00). The applicant may retain $130 per month for personal expenses. However, even having excess income is not necessarily a deal-breaker in terms of Medicaid eligibility.
Who is not eligible for Medicaid in Florida?
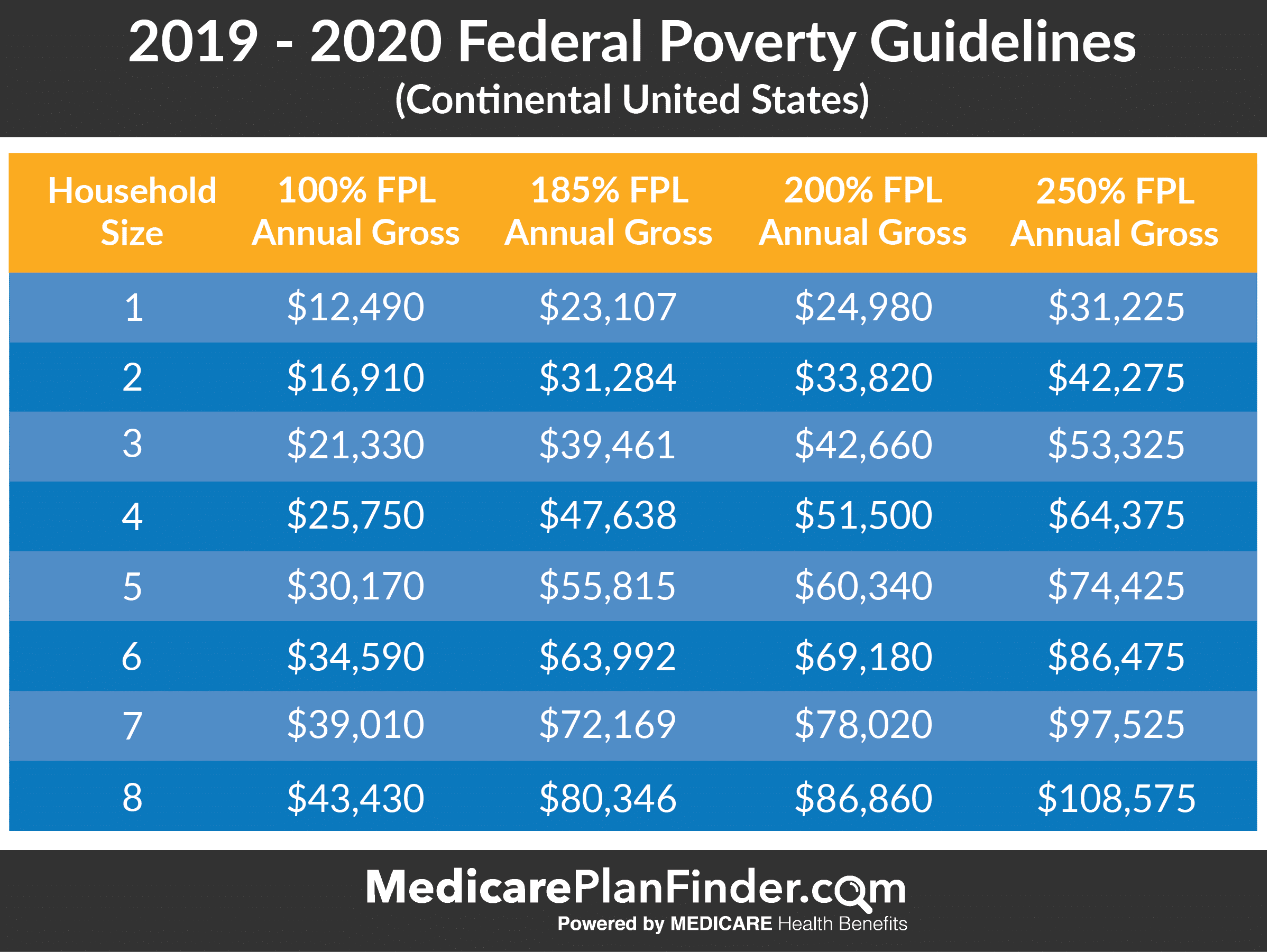
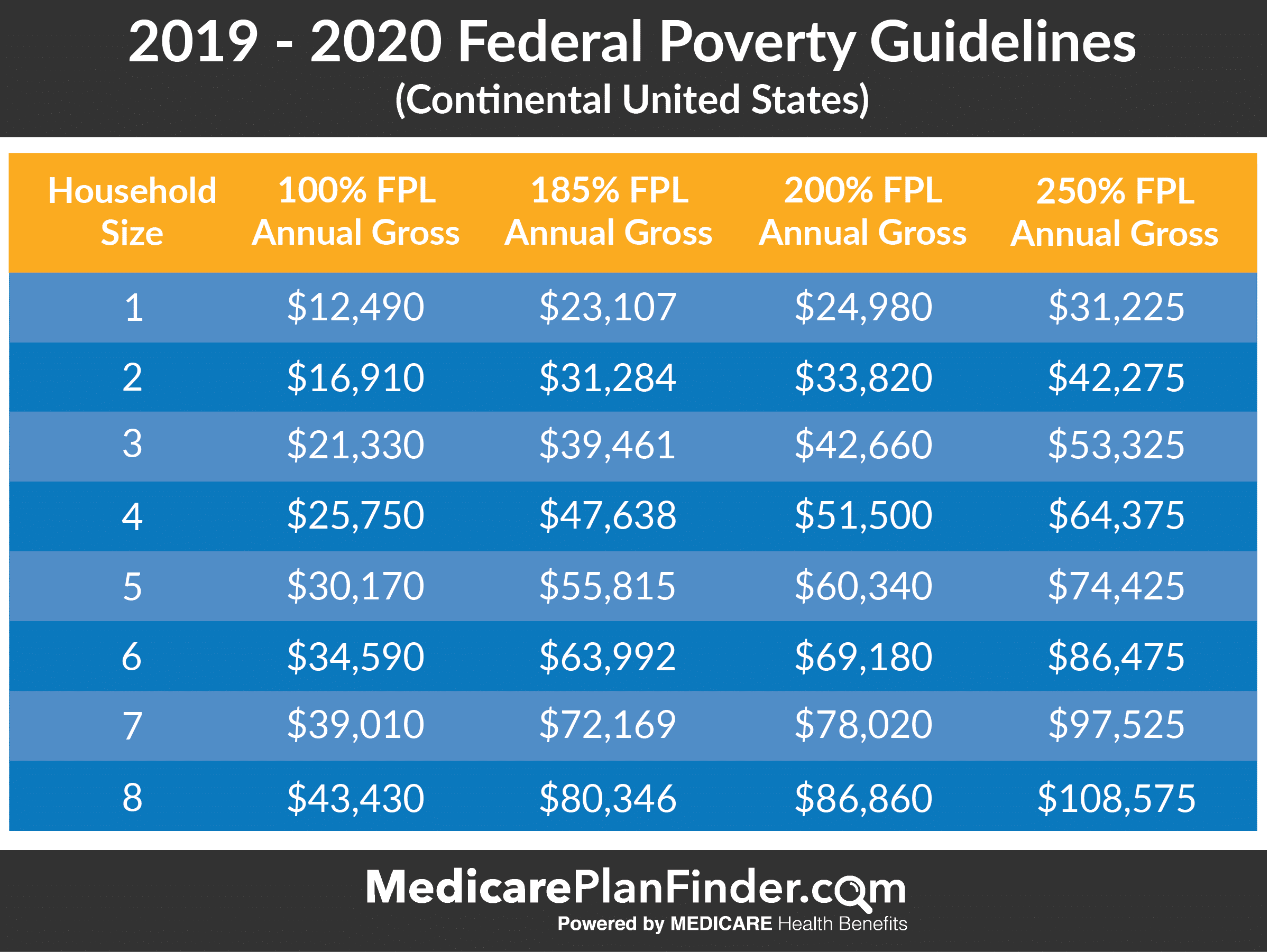
Able-bodied, non-elderly adults who don't have dependents are not eligible for Medicaid in Florida, regardless of how low their income is. Florida's eligibility standards are: Children up to 1 year old: 206% of the federal poverty level (FPL)
Can you have Medicare and Medicaid in Florida?
If you are dual eligible, you are can enroll in a dual eligible special needs plan (D-SNP) that covers both Medicare and Medicaid benefits. These plans may also pay for expenses that Medicare and Medicaid don't over individually, including over-the-counter items, hearing aids, and vision or dental care.
Who is eligible for Medicare in Florida?
Medicare is health insurance for people 65 or older. You're first eligible to sign up for Medicare 3 months before you turn 65. You may be eligible to get Medicare earlier if you have a disability, End-Stage Renal Disease (ESRD), or ALS (also called Lou Gehrig's disease).
How do I get free insurance in Florida?
Florida Health Insurance Overview You can also get low-cost or free Florida health insurance through public programs like Medicaid and the Children's Health Insurance Program (CHIP). Health insurance through Medicare is also a big deal in Florida.
What is considered low income in Florida?
As of 2022, the federal poverty line, which applies to Florida, is $13,590 for one person. That number increases by $4,720 for each additional family member, making $27,750 the 2022 federal poverty line for a family of four, according to HealthCare.gov.
How can I be eligible for Medicaid?
Medicaid beneficiaries generally must be residents of the state in which they are receiving Medicaid. They must be either citizens of the United States or certain qualified non-citizens, such as lawful permanent residents. In addition, some eligibility groups are limited by age, or by pregnancy or parenting status.
What is the lowest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
Is Medicare free in Florida?
How Much Does Medicare Cost in Florida? The cost of Original Medicare in Florida will be the same as the rest of the nation. With qualifying work history, most people are eligible for premium-free Part A coverage. Part B premiums for most people are $148.50 in 2021, but those with higher incomes will pay more.
Is everyone entitled to Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
About Medicare in Florida
Medicare beneficiaries in Florida may choose to receive their coverage from Original Medicare, Part A and Part B, or through a Medicare-approved in...
Types of Medicare Coverage in Florida
Original Medicare, Part A and Part B, is federally funded health insurance available to all eligible Medicare beneficiaries. Part A provides inpati...
Local Resources For Medicare in Florida
Medicare Savings Programs in Florida: For residents whose income falls below a certain limit, there are various programs that can assist with payin...
How to Apply For Medicare in Florida
The Medicare enrollment process is the same no matter what state you live in. To qualify for Medicare, you must be either a United States citizen o...
What is Medicaid in Florida?
Medicaid in Florida is sometimes referred to as the Statewide Medicaid Managed Care (SMMC) program. The Medicaid managed care program for long-term care services for the elderly and disabled is called the Long-term Care (LTC) program. All other health care services outside of long-term care are provided via the Managed Medical Assistance (MMA) ...
What is the exemption for Medicaid?
Exemptions include personal belongings, household furnishings, an automobile, irrevocable burial trusts, and one’s primary home, given the Medicaid applicant either resides in the home or has “intent” to return to it, and his / her equity interest in the home is not greater than $603,000 (in 2021).
How much is the spousal allowance for Medicaid in 2021?
That said, this spousal allowance may be as high as $3,260.00 / month (effective January 2021 through December 2021) and is based on one’s shelter and utility costs. This rule allows the Medicaid applicant to transfer income to the non-applicant spouse to ensure he or she has sufficient funds with which to live.
How long is the look back period for medicaid in Florida?
One should be aware that Florida has a Medicaid Look-Back Period, which is a period of 60 months that immediately precedes one’s Medicaid application date. During this time frame, Medicaid checks to ensure no assets were sold or given away under fair market value. If one is found to be in violation of the look-back period, a penalty period of Medicaid ineligibility will ensue.
Does Florida have Medicaid managed care?
Like many states, Florida has replaced their Medica id HCBS Waivers with a Medicaid managed care program. Former waivers, such as the Alzheimer’s Disease Waiver, Nursing Home Diversion Waiver, Assisted Living for the Elderly (ALE) Waiver, and the Consumer Directed Care Plus (CDC+) Waiver, have all been discontinued and replaced with the Statewide Medicaid Managed Care – Long Term Care (SMMC-LTC) program. To be clear, most but not all of the services and benefits that were available under the older waiver system have been preserved with the new Medicaid managed care model. Benefits may include adult day health care, meal delivery, respite care, personal emergency response systems, and personal care assistance, to name a few. More on the SMMC-LTC program.
Does Medicaid count stimulus?
Examples include employment wages, alimony payments, pension payments, Social Security Disability Income, Social Security Income, IRA withdrawals, and stock dividends. Medicaid does not count Covid-19 stimulus checks as income, which means they do not impact eligibility.
Can you take the Medicaid Eligibility Test in Florida?
Alternatively, one may opt to take the Medicaid Eligibility Test.
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is Medicare the first payer?
For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid ...
Can you be disqualified from Medicaid if you have assets?
Please note that income and assets over the Medicaid limit (s) in one’s state is not cause for automatic disqualification. This is because there are Medicaid-compliant planning strategies intended to lower one’s countable income and / or assets in order to meet the limit (s). A word of caution: It is vital that assets not be given away a minimum of 5 years (2.5 years in California) prior to the date of one’s Medicaid application. (New York is in the process of implementing a 2.5 year look back for long-term home and community based services). This is because Medicaid has a look-back period in which past transfers are reviewed to ensure an applicant (and / or an applicant’s spouse) has not gifted assets or sold them under fair market value. If this rule has been violated, it is assumed the assets were transferred in order to meet Medicaid’s asset limit and a penalty period of Medicaid disqualification will be calculated.
What income do you need to get medicaid in Florida?
This is calculated by a specific system that is known as the Modified Adjusted Gross Income, or MAGI.
How to apply for medicaid in Florida?
Many people choose to apply online, due to the fact that it is quick and easy. You can do this at the website for Florida Medicaid. Be prepared to answer a list of questions that have to do with your health, where you live, your legal status, your income, and your household. You will also need your basic information such as your name, address, phone number, age, and SSN. If you work, you will need verification of your income. You will need this information for everyone in your household.
What services does Medicaid cover?
These services might include community behavioral health, prescription medications, visual, dental, transportation, hospice, nursing home, home health care, family planning, hospital, doctor visits, and more.
What is the Medicaid agency in Florida?
The agency responsible for Medicaid in Florida is the Agency for Health Care Administration , also known as simply the Agency. The Agency has successfully completed implementing the SMMC ( Statewide Medicaid Managed Care) program. Under this program, most of the recipients of Medicaid are enrolled into one of a variety of health plans.
What is Florida Medicaid?
Medicaid is a program for medical assistance that gives low-income individuals and families access to health care that they wouldn’t otherwise have. Medicaid also assists people with disabilities and the elderly with the costs of expenses like care in nursing facilities and other long-term medical bills.
Who is eligible for SSI in Florida?
Florida residents who receive SSI (Supplemental Security Income) through the Social Security Administration. Patients who are disabled or over the age of 65. Children under 21. Those who are eligible to receive Temporary Cash Assistance. People under age 26 who were in a foster home.
Do you have to be a resident of Florida to live in a nursing home?
People in nursing homes or those who receive community or home-based care. You also have to be a Florida resident who has a valid social security number and a citizen of the U.S.
How long do you have to be a resident of Florida to qualify for Medicare?
To qualify for Medicare, you must be either a United States citizen or a legal permanent resident of at least five continuous years. Florida residents may be enrolled automatically a few months before they reach age 65, provided they already receive benefits through the Social Security Administration (SSA) or the Railroad Retirement Board (RRB). Others may be enrolled sooner if they receive SSA disability benefits or certain disability benefits from the RRB for more than 24 consecutive months. If you have ALS – amyotrophic lateral sclerosis, also known as Lou Gehrig’s disease – you’ll be enrolled in Medicare the same month that you start receiving disability benefits. No action is generally required in these cases, and residents will receive their red, white, and blue Medicare cards in the mail a few months prior to their start dates.
What is Medicare Advantage Plan?
These plans are required to cover everything that Original Medicare does (except for hospice care), but may include additional benefits like vision, dental, hearing, and prescription drug coverage.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance, also known as Medigap, provides coverage for out-of-pocket costs that are not covered by Original Medicare, which includes deductibles, copayments and, in some cases, medical care when traveling outside of the United States .
Does Florida have Medicare?
Not every Medicare plan may be available everywhere in Florida.
How to apply for medicaid in Florida?
Here are two ways you can get a Medicaid application form: Go to the Florida Access website. Call the local state Medicaid office.
What to do if your medicaid isn't approved?
If your Medicaid application isn’t approved, you have the right to appeal. If your Medicaid application was turned down for missing information or documentation, get whatever is needed and follow the instructions on the denial letter to resubmit the application.
Why is my medicaid denied?
Medicaid applications are often denied because of incomplete information on the application form. Before you submit your Medicaid application, be sure to have all of the following documentation ready. Proof of age (birth certificate or driver’s license). Proof of citizenship or alien status.
How often do you need to renew your medicaid?
Renewing your Medicaid application. You must fill out a new Medicaid application every year to stay in the Medicaid program. The Medicaid application process may be easier each year. For example, if they already have your birth certificate on file, they may not ask for it again with your next application.
Is Medicaid a state program?
Medicaid is a state-administered program for low-income and disabled U.S. citizens and legal aliens. Although many of the coverage details are determined by individual states, each state must provide certain services, such as specific hospital and doctor services. It’s possible to be eligible for both Medicare and Medicaid.
Is it better to understand Medicare before signing up?
We understand that Medicare matters can get quite complicated. It is better to get help understanding Medicare before you sign up for a plan. With our help, you will have in-depth health insurance knowledge of the benefits offered by basic and supplement plans.
Was William the nurse at Florida Health Agency helpful?
I was so nervous about selecting my first Medicare and drug plan. The staff at Florida Health Agency was very helpful, but William was amazingly patient, knowledgeable,and kind. I've sent friends and relatives to him as well.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
What is not covered by Medicare?
Offers benefits not normally covered by Medicare, like nursing home care and personal care services
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare cover health care?
If you have Medicare and full Medicaid coverage, most of your health care costs are likely covered.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
How to prove financial eligibility for medicaid in Florida?
To prove financial eligibility to enroll in Medicaid, applicant’s income will need to be verified with items like a W-2 form or paystubs. The Florida Medicaid application form requires you to give a lot of details about yourself and your family. Regardless of how and where you apply to Medicaid, you will need to provide the following information: ...
What information is needed for Florida Medicaid?
Your income and employer’s information. Your existing health coverage or any health coverage available through your employer. If you are married or have children, the Florida Medicaid form will need similar information about your spouse or dependents.
What is Medicaid application in Florida?
The Medicaid application and associated paperwork helps officials determine who is eligible for Medicaid coverage. Prospective applicants wondering where to apply for Medicaid in FL may be surprised about the methods and locations available for signing up for government assistance.
How often do you have to reapply for medicaid?
Recipients will have to reapply for Medicaid every 12 months or another predetermined time period. To sign up for Medicaid online, petitioners must create an online account. This account allows you to apply for Medicaid benefits and to check your eligibility for the program. A paper Medicaid application form is available for applicants who prefer ...
What happens if you are denied Medicaid in Florida?
If you are denied Medicaid enrollment, you have the right to file an appeal with the Florida Medicaid program, which will require program officials to review your application. The appeal process does not promise acceptance into the program, but does give you a second opportunity to be enrolled.
Do you have to list your parents on Medicaid?
Likewise, adults older than 21 years of age will also not have to list any adult relatives including their parents on their Medicaid form if they are filing taxes separately. However, family members filing taxes with the applicant will need to be listed on the form.
Do you have to include your spouse's health information when applying for medicaid in Florida?
However, unmarried partners who sign up for Florida Medicaid will not have to include details about the other if he or she does not want health care.
How to get a replacement Medicare card?
Go to Sign In or Create an Account. Once you are logged in to your account, select the "Replacement Documents" tab. Then select “Mail my replacement Medicare card.”. Your Medicare card will arrive in the mail in about 30 days at the address on file with Social Security so be sure to make sure your mailing address is correct before completing ...
What is the number to call for medicare?
If you can’t or prefer not to use the online service, you can call 1-800-MEDICARE ( 1-800-633-4227 TTY 1-877-486-2048 ).
What happens if my Medicare card is stolen?
If your Medicare card was lost, stolen, or destroyed, you can request a replacement with your personal my Social Security account. If you don’t already have an account, you can create one online. Go to Sign In or Create an Account.
Summary
Healthcare
Services
Benefits
Programs
Funding
Components
Qualification
- For Florida residents, 65 and over who do not meet the eligibility requirements in the table above, there are other ways to qualify for Medicaid. 2) Qualified Income Trusts (QITs) Persons seeking long-term care in a nursing home facility or require services in a home and community based setting have the option of putting excess income into a QIT. ...
Example
Criticism
Cost