There are 2 general eligibility requirements to qualify for a Medicare Advantage plan (Medicare Part C):
- You must be enrolled in Original Medicare (Medicare Part A and Part B).
- You must live in the service area of a Medicare Advantage insurance provider that is accepting new users during your...
Full Answer
How do I know if I have Medicare Advantage?
Nov 18, 2021 · There are 2 general eligibility requirements to qualify for a Medicare Advantage plan (Medicare Part C): 1. You must be enrolled in Original Medicare (Medicare Part A and Part B). 2. You must live in the service area of a Medicare Advantage insurance provider that is accepting new users during ...
How to switch from Original Medicare to Medicare Advantage?
To enroll in a Medicare Advantage plan, you must be eligible for, or already have, Medicare Part A (hospital insurance) and Medicare Part B (medical insurance) coverage. Most people qualify for Medicare Part A and Part B when they turn age 65 or have received disability benefits from the Social Security Administration or Railroad Retirement Board for 24 months.
How much can you make to qualify for Medicare?
Oct 13, 2021 · In most cases, here’s all you need to qualify for a Medicare Advantage plan. You must: Be enrolled in Medicare Part A and Part B, or be eligible for them; Live within the plan’s service area. That means that when you find a plan you’d like to sign up for, make sure the plan serves the county where you live. Read more on this later in this article. Good news about …
How do I enroll in Medicare Advantage?
How to join a Medicare Advantage Plan. Use Medicare's Plan Finder. Visit the plan's website to see if you can join online. Fill out a paper enrollment form. Contact the plan to get an enrollment form, fill it out, and return it to the plan. All plans must offer …
Is Medicare Advantage available to everyone?
Anyone who is eligible for Part A and Part B can enroll in a Medicare Advantage plan. MA plans are offered by private insurance companies who contract with Medicare.
Can I be turned down for a Medicare Advantage plan?
Generally, if you're eligible for Original Medicare (Part A and Part B), you can't be denied enrollment into a Medicare Advantage plan. If a Medicare Advantage plan gave you prior approval for a medical service, it can't deny you coverage later due to lack of medical necessity.
What is the difference between basic Medicare and Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
Why is Medicare Advantage being pushed so hard?
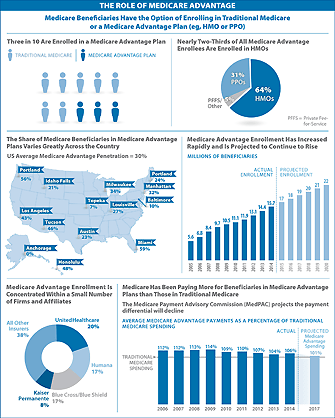
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.Feb 24, 2021
What pre-existing conditions are not covered?
Health insurers can no longer charge more or deny coverage to you or your child because of a pre-existing health condition like asthma, diabetes, or cancer, as well as pregnancy. They cannot limit benefits for that condition either.
Why can you be denied Medicare?
Medicare can deny coverage if a person has exhausted their benefits or if they do not cover the item or service. When Medicare denies coverage, they will send a denial letter. A person can appeal the decision, and the denial letter usually includes details on how to file an appeal.Aug 20, 2020
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.Feb 16, 2022
Can you switch back and forth between Medicare and Medicare Advantage?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
Is Medicare Advantage more expensive than Medicare?
Abstract. The costs of providing benefits to enrollees in private Medicare Advantage (MA) plans are slightly less, on average, than what traditional Medicare spends per beneficiary in the same county.Jan 28, 2016
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.Dec 21, 2021
How can Medicare Advantage plans charge no premium?
Medicare Advantage plans are provided by private insurance companies. These companies are in business to make a profit. To offer $0 premium plans, they must make up their costs in other ways. They do this through the deductibles, copays and coinsurance.
What age do you have to be to get Medicare Advantage?
Most people qualify for Medicare Part A and Part B when they turn age 65 or have received disability benefits from the Social Security Administration or Railroad Retirement Board ...
What is Medicare Advantage Plan?
Medicare Advantage plans are an alternative way for people to receive their Medicare Part A (hospital) and Part B (medical) benefits from private insurance companies approved by Medicare.
Do I have to pay Medicare Part B premium?
You must pay the Medicare Part B premium. Typically, you are still responsible for paying your Medicare Part B premium when you enroll in a Medicare Advantage plan. An exception may exist for people with limited incomes that qualify them for a Part B premium government subsidy. In addition to the Medicare Part B premium, ...
How old do you have to be to qualify for Medicare?
To qualify for Original Medicare, you must be: An American citizen or permanent legal resident of at least 5 years in a row. Aged 65 or older, or eligible due to disability.
Is Medicare Advantage different from Original Medicare?
Qualifying for a Medicare Advantage plan is actually not too different from qualifying for Original Medicare, Part A and Part B.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
Does Medicare cover dental?
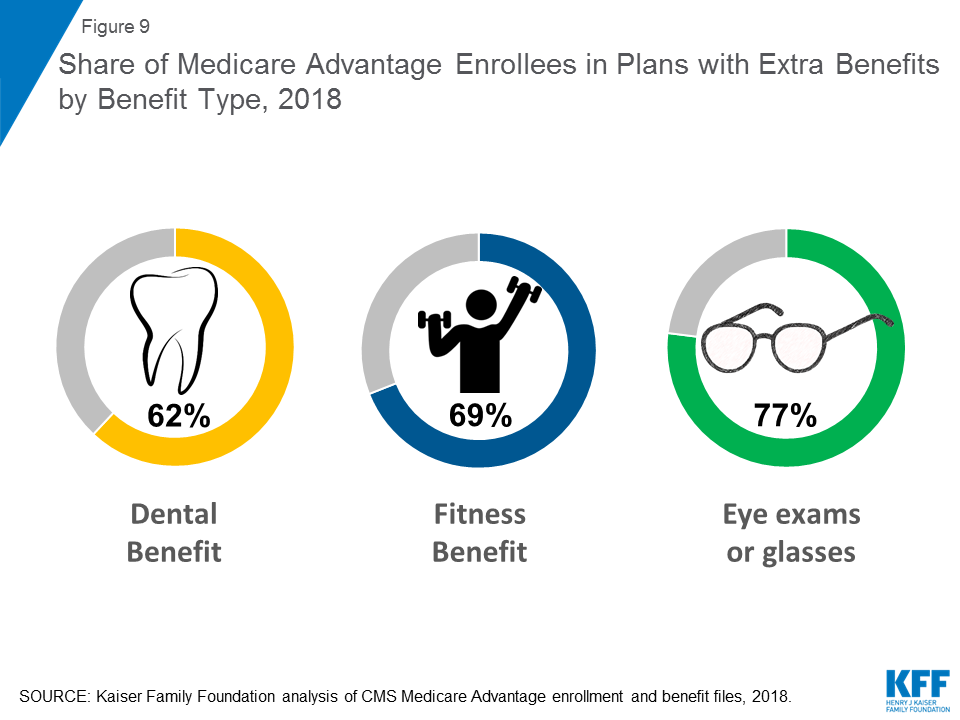
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What are the requirements for Medicare?
You must typically meet two requirements to receive Medicare benefits: 1 You are at least 65 years old 2 You are a U.S. citizen or a legal resident for at least five years
How long do you have to be a resident to qualify for Medicare?
Medicare eligibility chart - by age. - Typically eligible for Medicare if you're a U.S. citizen or legal resident for at least 5 years. - If you won't be automatically enrolled when you turn 65, your Initial Enrollment Period begins 3 months before your 65th birthday.
How much is Medicare Part A 2020?
In 2020, the Medicare Part A premium can be as high as $458 per month. Let’s say Gerald’s wife, Jessica, reaches age 62 and has worked for the required number of years to qualify for premium-free Part A once she turns 65. Because Jessica is now 62 years old and has met the working requirement, Gerald may now receive premium-free Part A.
Who can help you compare Medicare Advantage plans?
If you have further questions about Medicare eligibility, contact a licensed insurance agent today. A licensed agent can help answer your questions and help you compare Medicare Advantage plans (Medicare Part C) that are available where you live.
Is Medicaid based on income?
Yes. Medicaid qualification is based on income, not age. While Medicaid eligibility differs from one state to another, it is typically available to people of lower incomes and resources including pregnant women, the disabled, the elderly and children. Learn more about the difference between Medicare and Medicaid.
How old do you have to be to get Medicare?
Medicare eligibility at age 65. You must typically meet two requirements to receive Medicare benefits: You are at least 65 years old. You are a U.S. citizen or a legal resident for at least five years. In order to receive premium-free Part A of Medicare, you must meet both of the above requirements and qualify for full Social Security ...
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
How old do you have to be to apply for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old.
What is Medicare dual eligible?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program for seniors and disabled persons, Medicaid is a state and federal medical assistance program for financially needy persons of all ages. Both programs offer a variety of benefits, including physician visits and hospitalization, but only Medicaid provides long-term nursing home care. Particularly relevant for the purposes of this article, Medicaid also pays for long-term care and supports in home and community based settings, which may include one’s home, an adult foster care home, or an assisted living residence. That said, in 2019, Medicare Advantage plans (Medicare Part C) began offering some long-term home and community based benefits.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
Does Medicare provide long term care?
Long-Term Care Benefits. Medicaid provides a wide variety of long-term care benefits and supports to allow persons to age at home or in their community. Medicare does not provide these benefits, but some Medicare Advantage began offering various long term home and community based services in 2019. Benefits for long term care may include ...
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
Is there an age limit for Medicare?
Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
What is Medicare Advantage?
Medicare Advantage plans are private insurance health plans that provide all Part A and Part B services. Many also offer prescription drug coverage and other supplemental benefits. Similar to how Medicaid works with Original Medicare, Medicaid wraps around the services provided by the Medicare Advantage plan andserves as a payer of last resort.
What is dual eligible for medicaid?
Qualifications for Medicaid vary by state, but, generally, people who qualify for full dual eligible coverage are recipients of Supplemental Security Income (SSI). The SSI program provides cash assistance to people who are aged, blind, or disabled to help them meet basic food and housing needs.
What is dual eligible?
The term “full dual eligible” refers to individuals who are enrolled in Medicare and receive full Medicaid benefits. Individuals who receive assistance from Medicaid to pay for Medicare premiums or cost sharing* are known as “partial dual eligible.”.
Is Medicaid a payer of last resort?
Medicaid is known as the “payer of last resort.”. As a result, any health care services that a dual eligible beneficiary receives are paid first by Medicare, and then by Medicaid.
What is Medicaid managed care?
Medicaid managed care is similar to Medicare Advantage, in that states contract with private insurance health plans to manage and deliver the care. In some states, the Medicaid managed care plan is responsible for coordinating the Medicare and Medicaid services and payments.
Does Medicare cover Part A and Part B?
Some Medicare beneficiaries may choose to receive their services through the Original Medicare Program. In this case, they receive the Part A and Part B services directly through a plan administered by the federal government, which pays providers on a fee-for-service (FFS) basis. In this case, Medicaid would “wrap around” Medicare coverage by paying for services not covered by Medicare or by covering premium and cost-sharing payments, depending on whether the beneficiary is a full or partial dual eligible.
What is a PACE plan?
Similar to D-SNPs, PACE plans provide medical and social services to frail and elderly individuals (most of whom are dual eligible). PACE operates through a “health home”-type model, where an interdisciplinary team of health care physicians and other providers work together to provide coordinated care to the patient. PACE plans also focus on helping enrollees receive care in their homes or in the community, with the goal of avoiding placement in nursing homes or other long-term care institutions.