Medicare Advantage enrollees don’t have to pay a Part A or Part B deductible, but they do typically have to pay a separate deductible for prescription drugs if this coverage is included. Medicare Advantage plans vary widely in terms of what they cover and what they cost. Generally, the higher a plan’s monthly premium, the lower its deductible.
Full Answer
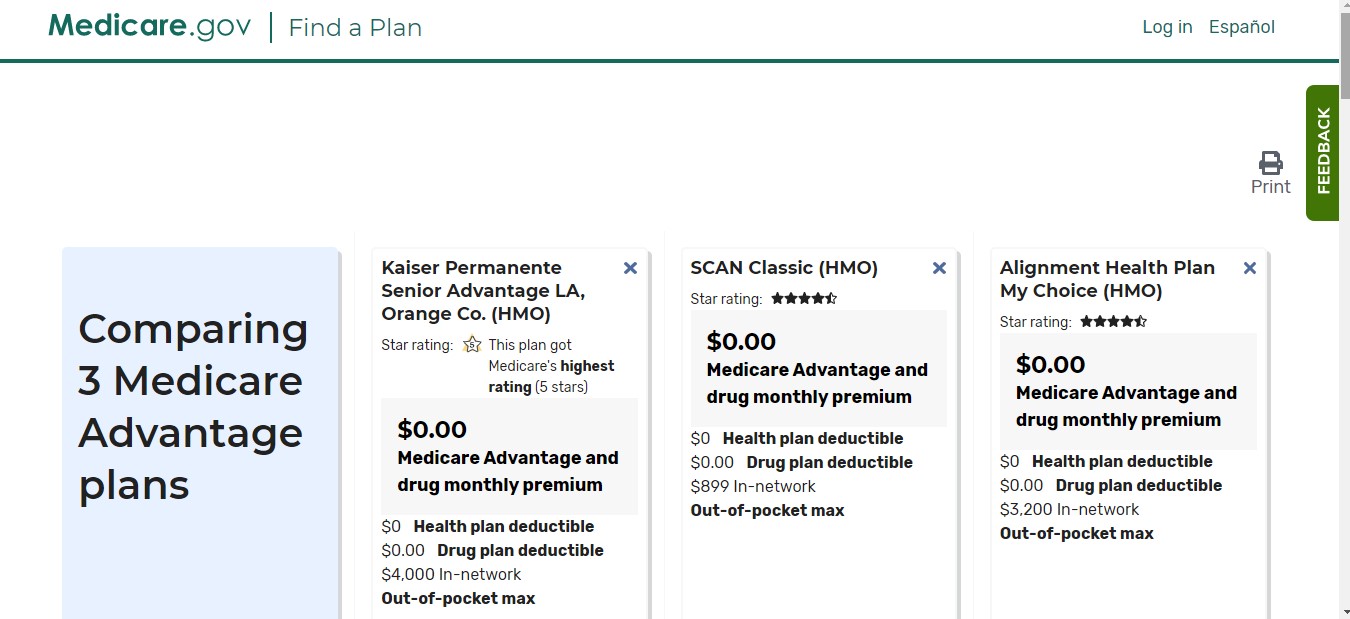
Does Medicare Advantage have deductible?
Yes, both Medicare Part A and Medicare Part B each come with a deductible. Medicare Advantage (Part C) and Medicare Prescription Drug Plans (Part D) may also include deductibles as well, although the costs associated with these plans are not standardized like they are in Original Medicare (Part A and Part B).
What do you pay in a Medicare Advantage plan?
- Complete a new Medicare enrollment (unless you are in your initial or special enrollment period)
- Switch from Original Medicare to Medicare Advantage
- Enroll in a stand-alone Part D prescription drug plan (unless you are moving to Original Medicare from Medicare Advantage)
How much does Medicare Advantage plan cost?
- $1,484 ($1,556 in 2022) deductible for each benefit period
- Days 1-60: $0 coinsurance for each benefit period
- Days 61-90: $371 ($389 in 2022) coinsurance per day of each benefit period
- Days 91 and beyond: $742 ($778 for 2022) coinsurance per each "lifetime reserve day" after day 90 for each benefit period (up to 60 days over your lifetime)
Is there a copay with Medicare?
What Is a Medicare Copayment? There are generally no copayments with Original Medicare — Medicare Part A and Part B — but you may have coinsurance costs. You may have a copayment if you have a Medicare Advantage plan or Medicare Part D prescription drug plan. The amount of your copayment in those cases varies from plan to plan.

Do Medicare Advantage plans have deductibles?
Medicare plans have deductibles just like individual or employer health insurance plans do. Both Original Medicare and, typically, Medicare Advantage Plans, require you to meet a deductible—an amount you pay for healthcare or for prescriptions—before your healthcare plan begins to pay.
What does the deductible mean in Medicare Advantage plans?
A deductible is the amount you must pay before your plan begins to pay. Some Medicare Advantage plans have separate deductibles for medical care and prescription drugs. If your Medicare Advantage plan has a network, only in-network care may apply towards the deductible.
What are the negatives to a Medicare Advantage Plan?
The takeaway There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling. Whether you choose original Medicare or Medicare Advantage, it's important to review healthcare needs and Medicare options before choosing your coverage.
Do you pay more out-of-pocket with Medicare Advantage?
Medicare Advantage plans, like most other private insurance plans, come with an annual out-of-pocket maximum. This is the maxium amount you will spend in a year on covered services.
How do you qualify for $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
What is the 2022 deductible for Medicare?
$233The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What is the highest rated Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Jun 22, 2022
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.
Does Medicare Advantage pay 100 percent?
Medicare Advantage plans must limit how much their members pay out-of-pocket for covered Medicare expenses. Medicare set the maximum but some plans voluntarily establish lower limits. After reaching the limit, Medicare Advantage plans pay 100% of eligible expenses.
What is the Medicare deductible for 2021?
$203 inThe standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.
How much should I expect to pay for a Medicare Advantage plan?
The average premium for a Medicare Advantage plan in 2021 was $21.22 per month. For 2022 it will be $19 per month. Although this is the average, some premiums cost $0, and others cost well over $100. For more resources to help guide you through the complex world of medical insurance, visit our Medicare hub.
How does Medicare deductible work?
How Medicare Deductibles Work. Before your Medicare coverage fully kicks in, most plans require that you pay a deductible—a set amount of money you have to pay, out of pocket, toward health-care expenses before your plan begins paying its share of costs . Deductibles aren’t your only Medicare cost —premiums and copayments are other costs ...
What is the Medicare Part B deductible?
The Part B deductible. Medicare Part B covers most of your regular medical expenses, such as doctor visits, preventative care, and lab work. Most people expect to use Part B more often than Part A, which is good because the Part B deductible is much lower and more straightforward. The Part B deductible resets annually on January 1, ...
What is Medicare Supplement?
Medicare Supplement —also known as Medigap—is an optional plan that covers costs Original Medicare doesn’t cover. Unlike other parts of Medicare, Medigap doesn't have a deductible.
What is Medicare Part D?
Medicare Part D is optional coverage you can buy to help pay for prescription drugs. Like the Part B deductible, this one resets annually too. Part D deductibles vary by plan, but by law must be $435 or lower (in 2020). 3
How many Medigap plans are there?
There are 10 Medigap plans currently available for purchase. Nine of these plans cover some or all of the Part A deductible, and seven of them pay 100% of that deductible. Finding a Medigap plan that covers the Part B deductible is more challenging.
How much is the 2020 Part B deductible?
The Part B deductible resets annually on January 1, so you’ll only ever pay it once per year. And, in 2020, the Part B deductible is just $198. 2. After you meet the Part B deductible, you'll pay a 20% coinsurance for covered services.
Do you have to pay a deductible for Medicare Advantage?
Medicare Advantage enrollees don’t have to pay a Part A or Part B deductible, but they do typically have to pay a separate deductible for prescription drugs if this coverage is included. Medicare Advantage plans vary widely in terms of what they cover and what they cost.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). .
What is Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. . Many Medicare Advantage Plans have a $0 premium. If you enroll in a plan that does charge a premium, you pay this in addition to the Part B premium. Whether the plan pays any of your monthly.
What is out of network Medicare?
out-of-network. A benefit that may be provided by your Medicare Advantage plan. Generally, this benefit gives you the choice to get plan services from outside of the plan's network of health care providers. In some cases, your out-of-pocket costs may be higher for an out-of-network benefit. .
What is covered benefits?
benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. and if the plan charges for it. The plan's yearly limit on your out-of-pocket costs for all medical services. Whether you have.
Who accepts Medicare?
who accepts. assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. if: You're in a PPO, PFFS, or MSA plan.
What is a medicaid?
Whether you have. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid.
What is Medicare Advantage Reimbursement?
Understanding Medicare Advantage Reimbursement. The amount the insurance company receives from the government for you as a beneficiary is dependent upon your individual circumstances. As a beneficiary of a Medicare Advantage plan, if your monthly health care costs are less than what your insurance carrier receives as your capitation amount, ...
Where does Medicare Advantage money come from?
The money that the government pays to Medicare Advantage providers for capitation comes from two U.S. Treasury funds.
What is the second fund in Medicare?
The second fund is the Supplementary Medical Insurance Trust which pays for what is covered in Part B, Part D, and more. As a beneficiary enrolled in a Medicare Advantage plan, you will also be responsible for some of the costs of your healthcare.
How old do you have to be to get Medicare Advantage?
How Does Medicare Advantage Reimbursement Work? In the United States, you are eligible to enroll in a Medicare Advantage plan if you are either 65 years of age or older, are under 65 with certain disabilities.
Does Medicare Advantage cover dental?
Medicare Advantage plans must provide the same coverage as Parts A and B, but many offer additional benefits, such as vision and dental care, hearing exams, wellness programs, and Part D, prescription drug coverage.
Is Medicare Part C required?
Having a Medicare Part C plan is not a requirement for Medicare coverage, it is strictly an option many beneficiaries choose. If you decide to enroll in a Medicare Advantage plan, you are still enrolled in Medicare and have the same rights and protection that all Medicare beneficiaries have.
What is the deductible for Medicare?
Each part of Medicare carries its own deductible. The Part A and Part B deductibles are standard for each beneficiary of Original Medicare. The Part C (Medicare Advantage) and Part D (prescription drug plan) deductibles will vary from plan to plan. Some Part C and Part D plans may have a $0 deductible. Some Medicare Advantage plans also feature $0 ...
How much is Medicare Part B deductible in 2021?
The Medicare Part B deductible in 2021 is $203 per year, and the Part A deductible is $1,484 per benefit period. Learn more about these costs and what you can expect.
How much is Medicare Part A 2021?
The Medicare Part A deductible for 2021 is $1,484 per benefit period . Unlike the deductible for Part B that operates on an annual basis, the Part A deductible starts and stops with each benefit period. A benefit period begins the day you are admitted for inpatient care at a hospital or skilled nursing facility, ...
What is the deductible for Part D?
Medicare defines a deductible as: “The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.”.
What percentage of Medicare coinsurance is 20 percent?
A 20 percent coinsurance means you (the beneficiary) would be responsible for 20 percent of a medical bill, while Medicare would pay the remaining 80 percent. It’s worth noting that the 20 percent you will pay as coinsurance is 20 percent of the Medicare-approved amount.
What is the coinsurance for Medicare Part B?
Coinsurance is the amount of the total bill that you must pay. A 20 percent coinsurance means you (the beneficiary) would be responsible for 20 percent ...
What is Medicare Supplement?
Medicare Supplement Insurance (also called Medigap) is a type of privately-sold insurance plan that is used in conjunction with Medicare Part A and Part B.