How does Aflac cancer policy pay?
First-Occurrence Benefit Aflac will pay $5,000 for the insured, $5,000 for the spouse, or $7,500 for children when a covered person is diagnosed with internal cancer. This benefit is payable only once for each covered person and will be paid in addition to any other benefit in this policy.
What all does Aflac cancer policy cover?
Aflac will pay $175 for each day a Covered Person receives and incurs a charge for blood and/ or plasma transfusions for the treatment of Internal Cancer or an Associated Cancerous Condition as an outpatient in a Physician's office, clinic, Hospital, or Ambulatory Surgical Center.
Does Medicare cover cancer treatment?
Medicare covers chemotherapy if you have cancer. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. covers it if you're a hospital inpatient. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Does Aflac pay for cancer death?
Aflac will pay $3,000 upon a covered person's onset date of carcinoma in situ. This benefit is payable once per covered person, per lifetime. Aflac will pay 25 percent of the Internal Cancer Benefit amount when a covered person suffers a cancer-related death. CANCER-RELATED DEATH: death as a result of internal cancer.
How much does Aflac pay for cancer screening?
No lifetime maximum. 3. NATIONAL CANCER INSTITUTE EVALUATION/CONSULTATION BENEFIT: Aflac will pay $500 when a Covered Person seeks evaluation or consultation at an NCI-Designated Cancer Center as a result of receiving a diagnosis of Internal Cancer or an Associated Cancerous Condition.
Does Aflac cancer policy cover mammograms?
MAMMOGRAPHY AND PAP SMEAR BENEFIT: Aflac will pay $100 per calendar year when a charge is incurred for an annual screening by low-dose mammography for the presence of occult breast cancer, and Aflac will pay $30 per calendar year when a charge is incurred for a ThinPrep or an annual Pap smear.
What is the Medicare approved amount for chemotherapy?
20%Medicare Part B usually covers 80% of outpatient cancer-related services, such as radiation therapy and chemotherapy, after a $203 deductible. The insured person is responsible for paying the remaining 20% of the costs.
What is the maximum out of pocket expense with Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
Does cancer qualify you for Medicare?
Part B covers many medically-necessary cancer-related outpatient services and treatments, but for some services, you must meet certain conditions. You may be in a hospital and still be considered an outpatient (observation status).
Is cancer insurance worth getting?
One shocking reason cancer insurance policies can be a waste of money is that most cancer insurance doesn't even cover skin cancer. And skin cancer is very common. Not only that, but cancer insurance most often doesn't cover outpatient expenses related to cancer treatment.
Does Aflac pay in one lump sum?
A lump sum benefit is paid directly to you upon diagnosis of having had a critical illness. Your dependent children are covered at no additional cost. We now offer the option of guaranteed-issue* lump sum critical illness coverage. That means no medical questionnaire is required.
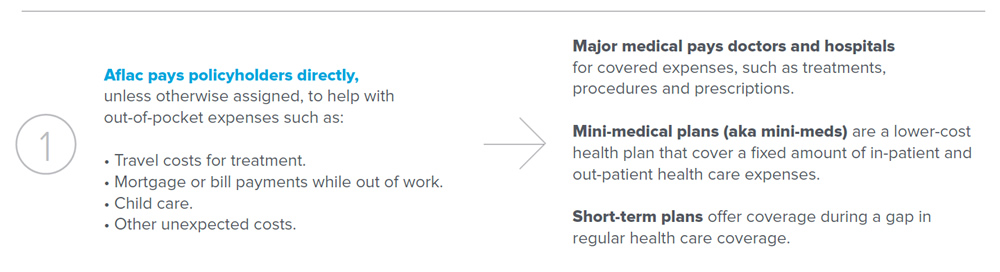
What does a cancer policy cover?
What does cancer insurance cover? Cancer insurance can help you handle medical plan deductibles, co-pays and other out-of-pocket costs; non-medical expenses such as transportation to treatment facilities; even everyday living expenses such as groceries, rent and mortgage payments.
What does a cancer policy cover?
What does cancer insurance cover? Cancer insurance can help you handle medical plan deductibles, co-pays and other out-of-pocket costs; non-medical expenses such as transportation to treatment facilities; even everyday living expenses such as groceries, rent and mortgage payments.
Is a cancer policy worth it?
One shocking reason cancer insurance policies can be a waste of money is that most cancer insurance doesn't even cover skin cancer. And skin cancer is very common. Not only that, but cancer insurance most often doesn't cover outpatient expenses related to cancer treatment.
Will Aflac cover surgery?
AFLAC will pay benefits according to the Schedule of Operations when a covered person has a surgical operation performed for a covered sickness in a hospital or ambulatory surgical center. Only one benefit is payable per 24-hour period for surgery even though more than one surgical procedure may be performed.
How much does Aflac pay for pap smear?
MAMMOGRAPHY AND PAP SMEAR BENEFIT: Aflac will pay $100 per calendar year when a charge is incurred for an annual screening by low-dose mammography for the presence of occult breast cancer, and Aflac will pay $30 per calendar year when a charge is incurred for a ThinPrep or an annual Pap smear.