
Agents selling Medicare Advantage and Part D plans get a flat dollar amount of money per application. This comes to them in the form of initial commissions and renewal commissions. Carriers pay out initial commissions when an agent makes a new sale or when the beneficiary enrolls in a new, “unlike” plan (different type).
How do agents get paid for selling Medicare plans?
Medicare agents get paid A commission that’s build into the product pricing. Generally there are ‘ first year ‘ amounts and ‘ renewal ‘ payments. Insurance premiums are set, agents can offer a better deal. Commissions are set by the insurance company. Sometimes additional monies may …
How does Medicare Advantage insurance work?
Mar 30, 2021 · An agent places a case and gets paid the amount for the state they are selling in. It is not actually that easy. The amount and timing of the payment will be influenced by a number of factors. New to Medicare: This one is easy. If the sale is someone new to Medicare, there will be a full payment without any pro rata reduction.
How much Commission do insurance providers make on Medicare Advantage plans?
Apr 29, 2021 · Generally, agents/brokers receive an initial payment in the first year of the policy (or when there is an “unlike plan type” enrollment change) and half as much for years two (2) and beyond if the member remains enrolled in the plan or make a “like plan type” enrollment change. Agents/brokers must be licensed in the State in which they do business, annually complete …
How do 2021 Medicare Advantage agent compensation levels work?
Mar 11, 2021 · If you sell 10 policies per month, that’s $6,070. Multiply that by 12 and you’ll earn $72,880 your first year. The best part about Medicare sales is the renewals. Renewals are lifetime with most companies Advantage plans. They are half of the initial commission. Using this same example an agent would get $36,440 in renewals in year 2.
How do you make money selling Medicare Advantage plans?
5 Tips for Selling Medicare Advantage Plans5 Tips for Selling Medicare Advantage Plans. ... Get Certified and “Ready-to-Sell” Next Year's Plans ASAP. ... Offer Different Types of Plans and Different Carriers. ... Have Your Own Lead-Generating, Direct Enroll Website. ... Stay Up to Date on the Rules.More items...•Aug 21, 2020
What are Medicare Advantage commissions for 2022?
The maximum commission for a Medicare Advantage (MA) sale in 2022 will be $573, a 6.3 percent increase over 2021. Some states have different levels. For example in California and New Jersey, the initial MA commissions increased from to $715-per-year, a 6.4% increase over 2021.
How do a Medicare Advantage plans make money with 0 premium?
Medicare Advantage plans are provided by private insurance companies. These companies are in business to make a profit. To offer $0 premium plans, they must make up their costs in other ways. They do this through the deductibles, copays and coinsurance.Oct 6, 2021
Are Medicare commissions prorated?
Any case that is not new to Medicare will be subject to a pro- rated payment amount. This means you will get paid based on the month the person become effective in the new policy. A case with a 6-1 effective date will be 50% pro-rated. In other words, the commission will be half of the initial/new commission.Mar 30, 2021
What is the commission for Medicare?
The commission for subsequent years (i.e., the renewal commission) is set at 10 percent of the premium. Based on our analysis, the average premium in 2020 for Medigap was $1,660, meaning an agent would be paid $322 for the first year and $166 as a renewal commission.Oct 12, 2021
What are the disadvantages to a Medicare Advantage Plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Why is Medicare Advantage being pushed so hard?
Advantage plans are heavily advertised because of how they are funded. These plans' premiums are low or nonexistent because Medicare pays the carrier whenever someone enrolls. It benefits insurance companies to encourage enrollment in Advantage plans because of the money they receive from Medicare.Feb 24, 2021
What is a Ga override?
GA contract overrides vary by company GAs receive override payments directly. The street compensation is paid directly to the sub producer, or the GA (for their own production) Insurance carriers have initial and ongoing requirements that they must meet to obtain and keep a GA contract.
Is selling Medicare lucrative?
Is Selling Medicare Lucrative? In short, yes. The average Medicare Advantage policy pays around $287 a year in commission if the purchase replaces an existing plan. However, you can get approximately double that — $573— if you write up a new Medicare Advantage plan for someone who hasn't had one before.Feb 22, 2022
What is a Medicare MSA account?
The Medicare MSA Plan deposits money in a special savings account for you to use to pay health care expenses. The amount of the deposit varies by plan. You can use this money to pay your Medicare-covered costs before you meet the deductible.
What is agent broker compensation?
Below is a link to a file containing the amounts that companies pay independent agents/brokers to sell their Medicare drug and health plans. Companies that contract with Medicare to provide health care coverage or prescription drugs typically use agents/brokers to sell their Medicare plans to Medicare beneficiaries.
What happens to a broker if they don't comply with Medicare?
Agents/brokers are subject to rigorous oversight by their contracted health or drug plans and face the risk of loss of licensure with their State and termination with their contracted health or drug plans if they don't comply with strict rules related to selling to and enrolling Medicare beneficiar ies in Medicare plans.
When do brokers receive initial payment?
Generally, agents/brokers receive an initial payment in the first year of the policy (or when there is an “unlike plan type” enrollment change) and half as much for years two (2) and beyond if the member remains enrolled in the plan or make a “like plan type” enrollment change.
How do insurance agents make money?
Payment from Initial Enrollment. One of the primary ways how insurance agents earn money is when a consumer enrolls in a new plan. For instance, this can be when you enroll in your very first plan or if you enroll in a new plan that’s unlike what you were previously enrolled in. The maximum amounts of commission for Medicare Advantage ...
How long does Medicare have to renew?
Depending on the insurance carrier and Medicare plan type, there may be a lifetime renewal commission or they may be capped after five or six years. Luckily, by that time, it may be a good idea to review your plan to make sure it still matches your health care needs anyway.
What is captive agent insurance?
Captive agents are employed directly by a specific company to sell their insurance plans. They usually receive a salary like any other employee, though may also earn commission for the plans they sell. Don’t worry, even though they’re tied to only one company, they’re still required to follow the rigorous regulations set forth by CMS.
Do independent agents have to be contracted with CMS?
Instead of being employed by the carriers, independent agents need to be contracted with individual plans to sell them.
What is Medicare Advantage?
Medicare Advantage plans are managed care, which means you might need prior authorization for a medication, you may need a referral to see a specialist, and you may have to try a cheaper treatment plan before your plan will approve a more expensive one. That’s how Medicare Advantage plans manage their costs.
Is Medicare Advantage a low premium?
Most Medicare Advantage plans are paid enough by the government to offer very low – sometimes even $0 premium plans – in addition to extra benefits that go above and beyond what Medicare regularly covers. For example, you might get some dental, vision, and fitness benefits.
How does Medicare Advantage work?
Agents selling Medicare Advantage and Part D plans get a flat dollar amount of money per application. This comes to them in the form of initial commissions and renewal commissions. Carriers pay out initial commissions when an agent makes a new sale or when the beneficiary enrolls in a new, “unlike” plan (different type). Each year and beyond, carriers pay out renewal commissions to the agent if the beneficiary remains enrolled in the plan or enrolls in a new, “like” plan (same type).
What does it mean when you assign commissions to the FMO?
When you assign your commissions to the FMO, this means the carrier will pay the FMO, who will then pay you . Agents signing an Assignment of Commissions contract must be careful, because depending on their contract, their upline could keep their renewals should they choose to leave.
Do carriers pay agents?
It’s important for agents to know that carriers pay agents and FMOs separately. Your relationship with an FMO is comparable to your clients’ relationship with you.
Do insurance carriers have to pay Medicare Advantage commissions?
The Centers for Medicare & Medicaid Services (CMS) set the maximum broker commissions for Medicare Advantage and Medicare Part D annually; however, insurance carriers aren’t required to pay these amounts. What you earn for Medicare Advantage and PDP sales could be less, depending on the carrier and your contract with them.
What is Medicare Advantage?
Medicare Advantage (Medicare Part C) is an alternative way to get your benefits under Original Medicare (Part A and Part B). By law, Medicare Advantage plans must cover everything that is covered under Original Medicare, except for hospice care, which is still covered by Original Medicare Part A.
Does Medicare Advantage have a lower cost?
In return, however, Medicare Advantage plans tend to have lower out-of-pocket costs than Original Medicare, and unlike Original Medicare, Medicare Advantage plans also have annual limits on what you have to pay out-of-pocket before the plan covers all your costs.
Does Medicare Advantage charge a monthly premium?
In addition to the Part B premium, which you must continue to pay when you enroll in Medicare Advantage, some Medicare Advantage plans also charge a separate monthly premium.
Can I enroll in a zero premium Medicare Advantage plan?
You may be able to enroll in a zero-premium Medicare Advantage plan (although, remember, you still have to pay your regular Part B premium) and you may have other costs, such as copayments and coinsurance.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
What is the difference between Medicare Advantage and Original Medicare?
Medicare Advantage plans are provided by private health insurance companies and group healthcare providers whereas Original Medicare coverage comes from the federal government’s Medicare program. Both have their pros and cons.
Why is Medicare Advantage so bad?
These are the 7 most common reasons we’ve documented that make people feel Medicare Advantage plans are terrible: Free plans are not really free. Hospitalization costs more, not less. They make you pay multiple copays for the same issue. You are more likely to see a nurse practitioner than a doctor.
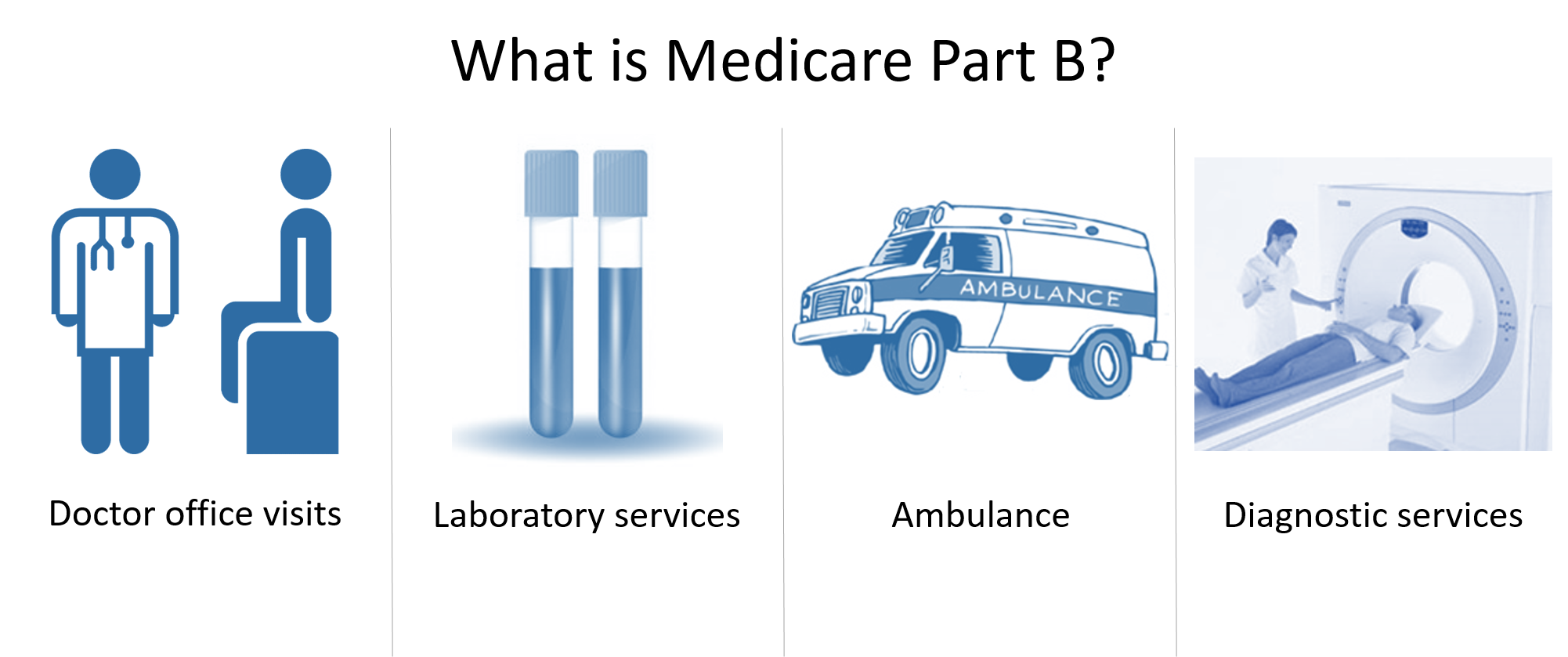
What is Medicare Part B rebate?
ALSO: Some zero-dollar premium Advantage health plans can rebate all or a portion of your Medicare Part B. Medicare Part B is medical coverage for people with Original Medicare. It covers doctor visits, specialists, lab tests and diagnostics, and durable medical equipment. Part A is for hospital inpatient care....
What is Medicare premium?
A premium is an amount that an insurance policyholder must pay for coverage. Premiums are typically paid on a monthly basis. In the federal Medicare program, there are four different types of premiums. ... , but pay virtually nothing when you use healthcare services once the annual Part B premium is paid.
How many standardized plans are there for Medigap?
With Medigap, there are ten standardized plans (A, B, C, D, F, G, K, L, M, and N). Regardless of which insurance company you get a plan from, its benefits and coverage are the same. Only the monthly premium is different. With Medicare Advantage plans, your costs and coverage aren’t as clear-cut.
When does Medicare enroll?
It occurs every Fall from October 15 to December 7.
Does Medicare Advantage cover vision?
In addition to the fact that Medicare Advantage plan insurance carriers are generally obligated to sell you a plan, they also bundle additional benefits, such as vision, dental, hearing, and a prescription drug plan (Part D). These are valuable benefits that Original Medicare does not cover.
