Blue Cross ® Medicare Supplement
Medigap
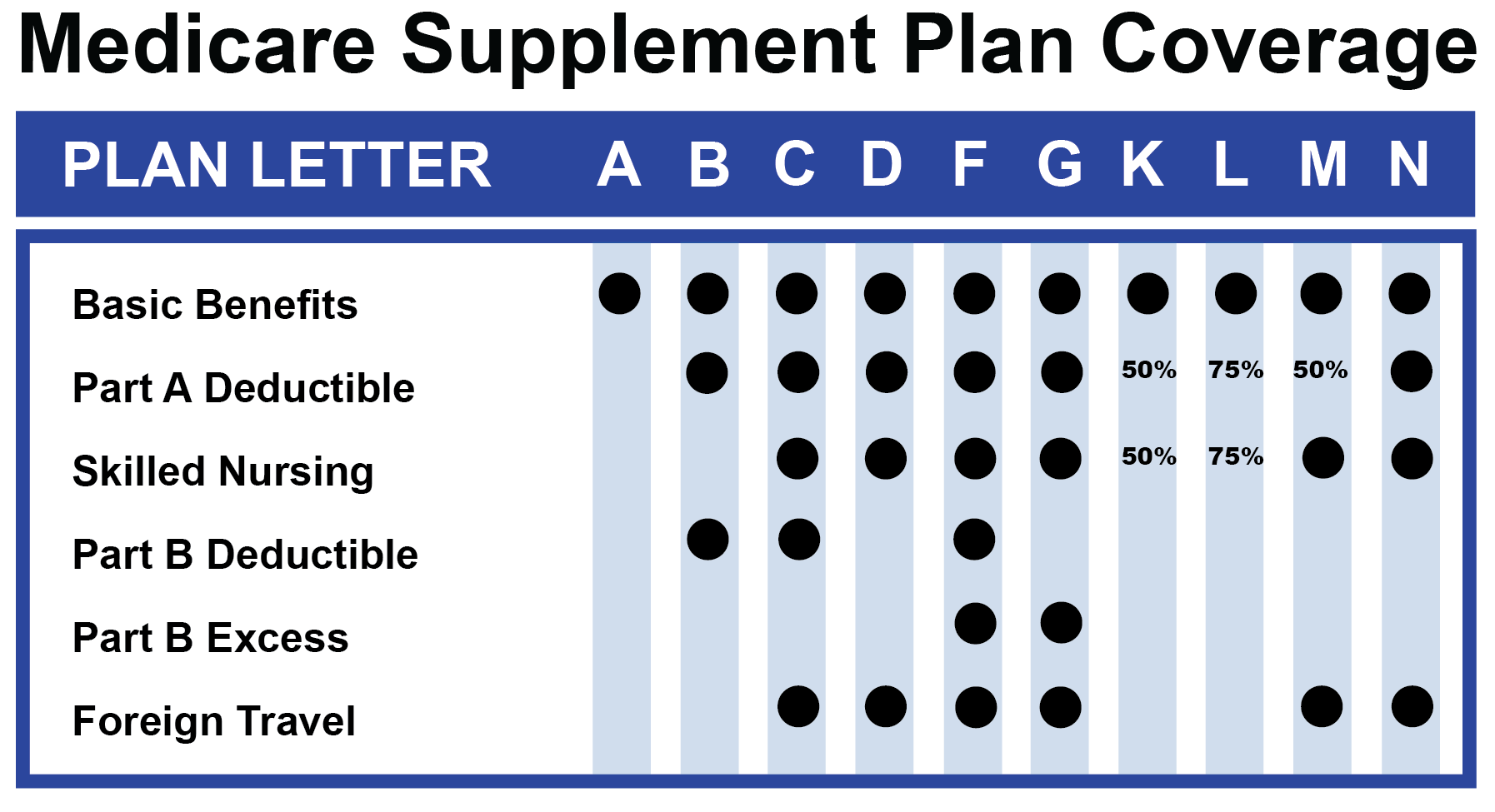
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
What is the Blue Cross Medicare plan?
What Medicare Advantage Plans Does Blue Cross Blue Shield Offer in 2022?
- Blue Cross offers a variety of Medicare Advantage plans.
- Many plans include prescription drug coverage, or you can purchase a separate Part D plan.
- Many of the Blue Cross Medicare Advantage plans offer $0 monthly premiums along with prescription drug coverage.
How to become a Blue Cross?
These are some of the tools you’ll have access to:
- Electronic Funds Transfer (EFT): for sending payments to your choice of financial accounts
- Electronic Connectivity: exchange information with us electronically
- web-DENIS: for verifying patient eligibility and benefits and tracking claims
- e-referral: for submitting and reviewing patient authorizations
Does Blue Cross Blue Shield have a Medicare Advantage plan?
Medicare Advantage plans offer all the coverage of Original Medicare — plus benefits not covered by Medicare or most Medicare Supplement insurance plans, including built-in prescription drug coverage and extra health and wellness options. Blue Cross and Blue Shield of Montana (BCBSMT) offers both individual and group Medicare Advantage plans.
Is Blue Cross Blue Shield good insurance?
Blue Cross Blue Shield is one of the giants and is still a trustworthy health insurance provider. Blue Cross Blue Shield is one of the best overall health insurance companies: it has a comprehensive range of policies available in many locations and discounts to health and wellness programs.

How do I get my $800 back from Medicare?
All you have to do is provide proof that you pay Medicare Part B premiums. Each eligible active or retired member on a contract with Medicare Part A and Part B, including covered spouses, can get their own $800 reimbursement.
Which is better BCBS standard or basic?
BCBS Basic in many ways has lower cost-sharing (copays/coinsurance) than Standard. In addition, it has lower premiums.
What is the difference between basic Medicare and Medicare Advantage?
With Original Medicare, you can go to any doctor or facility that accepts Medicare. Medicare Advantage plans have fixed networks of doctors and hospitals. Your plan will have rules about whether or not you can get care outside your network. But with any plan, you'll pay more for care you get outside your network.
Is Medicare the same as Blue Cross?
BCBS is an iconic health insurance brand represented by numerous independent affiliated companies. BCBS companies have been part of the Medicare program since it began in 1966 and now offers multiple Medicare insurance options.
What is the difference between BCBS basic and FEP blue focus?
Basic Option provides coverage for preventive dental care services only, while Standard Option provides coverage for preventive dental care and some other non-routine services. FEP Blue Focus does not offer dental benefits.
What does no deductible mean?
Having zero-deductible car insurance means you selected coverage options that don't require you to pay any amount up front toward a covered claim. For example, say you opted for collision coverage with no deductible. If you have a covered claim for $1,500 in repairs, your insurer would reimburse you the full $1,500.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Is it necessary to have supplemental insurance with Medicare?
For many low-income Medicare beneficiaries, there's no need for private supplemental coverage. Only 19% of Original Medicare beneficiaries have no supplemental coverage. Supplemental coverage can help prevent major expenses.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Does Medicare have a yearly deductible?
Yes, you have to pay a deductible if you have Medicare. You will have separate deductibles to meet for Part A, which covers hospital stays, and Part B, which covers outpatient care and treatments. What is the Medicare deductible for 2022? The Part A deductible for 2022 is $1,556 for each benefit period.
What plan provides both Medicare and Medicaid coverage?
UnitedHealthcare Connected® for One Care (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
Is Blue Anthem Medicare?
Anthem Blue Cross is an HMO plan with a Medicare contract. Enrollment in Anthem Blue Cross depends on contract renewal.
What is a Medigap plan?
Medigap (Medicare Supplement) is an option for those with Original Medicare. It covers the out-of-pocket costs for the health expenses not typically covered by Medicare Parts A and B (Original Medicare). Individuals enrolled in Medicare Advantage do not need to purchase a Medigap plan.
Does Medicare Advantage cover emergency services?
On the other hand, Medicare Advantage plans typically have a network but will cover urgent and emergency services anywhere in the country. FAQ Item Question. Limited Coverage. FAQ Item Answer.
How much does Medicare pay for coinsurance?
When you have Original Medicare, you pay 20 percent of the cost, or 20 percent coinsurance, for most medical services covered under Part B. Medicare Advantage plans use copays more than coinsurance. Which means you pay a fixed cost. You might have a $15 copay for doctor office visits, for example.
What is Medicare Advantage?
You buy Medicare Advantage plans from private health insurance companies that contract with the government. They work with Original Medicare coverage. Part D covers prescription drugs. Many Medicare Advantage plans combine Parts A, B and D in one plan. And each Medicare plan only covers one person.
What is Medicare Part D coverage?
Medicare Part D prescription coverage has something called the coverage gap , or donut hole. The coverage gap is a stage in which you pay much more out of pocket for your prescription drugs. It's not based on a time period.
What is the difference between Medicare Supplement and Medicare Advantage?
Medicare supplement, or Medigap, plans are another option. In a way, Medicare Advantage replaces Original Medicare and connects all the pieces together on one plan. Supplement plans don't replace Original Medicare. It's more like an extra you can add on top of Original Medicare.
Why are Medicare Advantage plans so popular?
Medicare Advantage plans are popular because of their convenience. Most plans combine medical and prescription coverage on one card. Some offer dental and vision coverage, too. And you're able to predict your out-of-pocket costs better than you can with Original Medicare.
Does Medicare have a cap?
That means once you spend a certain amount of money on health care each year, your plan pays 100 percent of the cost of services it covers. Original Medicare doesn't have this cap. So if you get really sick, you'll end up paying a lot.
Do Medicare supplement plans come with dental?
And supplement plans don't come with the extra benefits you often get with Medicare Advantage, like dental and vision coverage. The triangles to the right show how supplement plans sit on top of Medicare Parts A, B and D. You can get complete coverage, but you still have to coordinate all those pieces on your own.
Get money back
There are no restrictions on how you can use your $800 reimbursement. Most claims will be reviewed within one to two business days after they have been received. Upon approval, you will receive reimbursement by direct deposit or check, depending on how you set up your account.
Submit your claim
You can submit proof of premium payments through the online portal, EZ Receipts mobile app (available at the App Store® and Google Play™) or by mail or fax. You have until December 31 of the following benefit year to submit your claim for reimbursement.
What happens when you retire with Medicare?
When you retire and have Medicare, it typically becomes your primary coverage and they pay first. If you decide to combine your Medicare and Service Benefit Plan coverage, we’ll pay for covered services not covered by Medicare. When you receive care, you should show your providers both your Service Benefit Plan member ID card ...
What is the service benefit plan?
When you’re an active federal employee, the Service Benefit Plan is typically your primary coverage, which means we pay for your healthcare services first.
Does Medicare pay for its own network?
Medicare has its own network of Participating providers who accept Medicare’s assignment or payment. When you visit a provider (regardless of if they accept Medicare’s assignment), we’ll pay the difference between what Medicare pays and what you owe the provider.*.
How to change Medicare plan?
The Medicare Open Enrollment Period provides an annual opportunity to review, and if necessary, change your Medicare coverage options. Coverage becomes effective on January 1. During Open Enrollment, some examples of changes that you can make include: 1 Join a Medicare Advantage (Part C) plan. 2 Discontinue your Medicare Advantage plan and return to Original Medicare (Part A and Part B). 3 Change from one Medicare Advantage plan to another. 4 Add or Change your Prescription Drug Coverage (Part D) plan if you are in Original Medicare.
What is the initial enrollment period for Medicare?
The Initial Enrollment Period is a limited window of time when you can enroll in Original Medicare (Part A and/or Part B) when you are first eligible. After you are enrolled in Medicare Part A and Part B, you can select other coverage options like a Medicare Advantage plan from approved private insurers.
What is a copayment in Medicare?
Copays. A copayment may apply to specific services, such as doctor office visits. Coinsurance. Cost sharing amounts may apply to specific services. Out-of-Pocket Expenses. All Medicare Advantage plans have an annual limit on your out-of-pocket expenses, which is a feature not available through Original Medicare.
Does Medicare Advantage have copayments?
Medicare Advantage plans may have copayments or cost sharing amounts on Medicare covered services that differ from the cost sharing amounts in Original Medicare. Medicare Advantage plans may change their monthly premiums and benefits each year. This also occurs in Original Medicare, as Part B premiums, standard deductibles ...
Does Medicare Advantage have geographic service areas?
Limits. Medicare Advantage plans have defined geographic service areas and most have networks of physicians and hospitals where you can receive care. Ask your physicians if they participate in your health insurance plan’s Medicare Advantage network.
Do you have to enroll in Medicare before joining a Medicare Advantage plan?
You must first enroll in Medicare Part A and Part B before joining a Medicare Advantage plan. Contact your local Blue Cross Blue Shield company for help choosing a Medicare Advantage plan and getting enrolled.
Why combine Medicare Part A and B?
Another reason to combine your coverage is to get access to benefits not covered by Medicare.
What is Blue365 for Blue Cross?
Blue365 is a discount program exclusively for Blue Cross and Blue Shield members. Through the program, you can get discounts on different products and services that can help you live a healthy lifestyle, such as diet and exercise plans, gym shoes and athletic apparel, hearing aids and more.
What is Medicare for people over 65?
GET TO KNOW MEDICARE. Medicare is a health insurance program provided by the federal government, available to people: • 65 and older • Under 65 with certain disabilities • With permanent kidney failure who need dialysis treatment or a transplant (End-Stage Renal Disease) .
What is Blue365 discount?
Through the program, you can get discounts on different products and services that can help you live a healthy lifestyle, such as diet and exercise plans, gym shoes and athletic apparel, hearing aids and more. View all the current available deals at
How to contact Medicare for service benefits?
or call 1-800-MEDICARE (TTY: 1-877-486-2048) . << Previous Next >>. 3. Combining your Service Benefit Plan coverage with Medicare is a choice. Here are some things to know that can help you decide: Keep your future healthcare needs in mind before making a decision.
What is the penalty for late enrollment in Medicare?
The penalty is a 10% premium increase for each year you choose to delay your enrollment.
How much is the penalty for delay in Medicare?
The penalty is a 10% premium increase for each year you choose to delay your enrollment. So, if you decide to enroll five years after you’re first eligible, your premium would be 50% higher than it would be if you had taken Medicare initially. There is an exception to this.
