How is Centene’s Medicare Advantage Business performing?
Our acquisitions of Health Net and Wellcare paved the way for us to offer consumers a 4-star Medicare Advantage product and expand our geographical footprint to 31 states. In 2020, Centene and Ascension have partnered in Florida, Kansas, and Illinois to offer a Medicare Advantage plan, Ascension Complete. The joint venture is a Medicare Advantage plan shaped …
Where is Centene expanding Medicare coverage in 2020?
Oct 04, 2021 · ST. LOUIS, Oct. 4, 2021 /PRNewswire/ -- Centene Corporation (NYSE: CNC) announced today it plans to expand its Medicare Advantage offerings, offering its wide range of Medicare Advantage plans in 1,575 counties across 36 states during the 2022 Medicare Annual Enrollment Period (AEP). "At a time when many seniors and their families are still ...
Why did Centene focus on Medicaid?
Oct 01, 2021 · Allwell Medicare Advantage from SilverSummit HealthPlan. Introducing Wellcare. Our health plans are getting a new look & name: Wellcare. The same great benefits and coverage you expect with a fresh new feel. ... Wellcare is the Medicare brand for Centene Corporation, an HMO. PPO, PFFS, PDP plan with a Medicare contract and is an approved Part D ...
Will Centene expand Medicare coverage in Nevada?
Oct 07, 2019 · "Offering Medicare allows SilverSummit Healthplan to further deliver on our commitment to improve access to quality healthcare in the communities that we serve." Medicare is a government health...
Who owns SilverSummit healthplan?
Centene CorporationSilverSummit Healthplan is a wholly-owned subsidiary of Centene Corporation, a Fortune 500 company.
What is Nevada Check Up program?
Nevada Check Up is the state of Nevada's Children's Health Insurance Program. It provides low-cost, comprehensive health care coverage to low income, uninsured children 0-19 years of age who are not covered by private insurance or Medicaid.
What are the different Medicaid plans in Nevada?
If you're looking to enroll in Nevada Medicaid to access a variety of medical or wellness benefits, then you'll need to sign for a Medicaid health insurance plan in NV....Anthem Blue Cross and Blue Shield. Website: https://mss.anthem.com/nevada-medicaid/home.html. ... Health Plan of Nevada (HPN) ... SilverSummit Health Plan.Jan 1, 2021
What is straight Medicaid in Nevada?
Nevada Medicaid is a program which provides quality health care services to low-income Nevadans who qualify based on federal and state law. Nevada Medicaid does not reimburse an individual for medical services; rather, payments are sent directly to the health care providers for services provided to Medicaid recipients.
Is my Nevada Medicaid active?
If you need to manage your Medicaid or Nevada Check Up plan, you can call 1-877-543-7669, visit Access Nevada, or visit the Division of Welfare and Supportive Services for a list of local numbers.
What is the Medicaid income limit in Nevada?
In Nevada, households with annual incomes of up to 138% of the federal poverty level may qualify for Medicaid. This is $16,753 per year for an individual, or $34,638 per year for a family of four. For more information on Medicaid in Nevada and to see if you're eligible, visit Access Nevada.
What Medicaid plan is best?
Kaiser Foundation Health Plan of the Mid-Atlantic States, Inc. attained the highest overall rating among Medicaid plans for HPR 2021. The plan demonstrated high-quality preventive care, with five stars for nearly every prevention measure for which it provided data.Mar 1, 2022
Is Health Plan of Nevada Medicaid?
Welcome to Health Plan of Nevada's Medicaid Plan.
Does Nevada have managed Medicaid?
Nevada has been operating a mandatory managed care program in two counties in the state (Clark and Washoe Counties) since 1998.
How does Medicare work in Nevada?
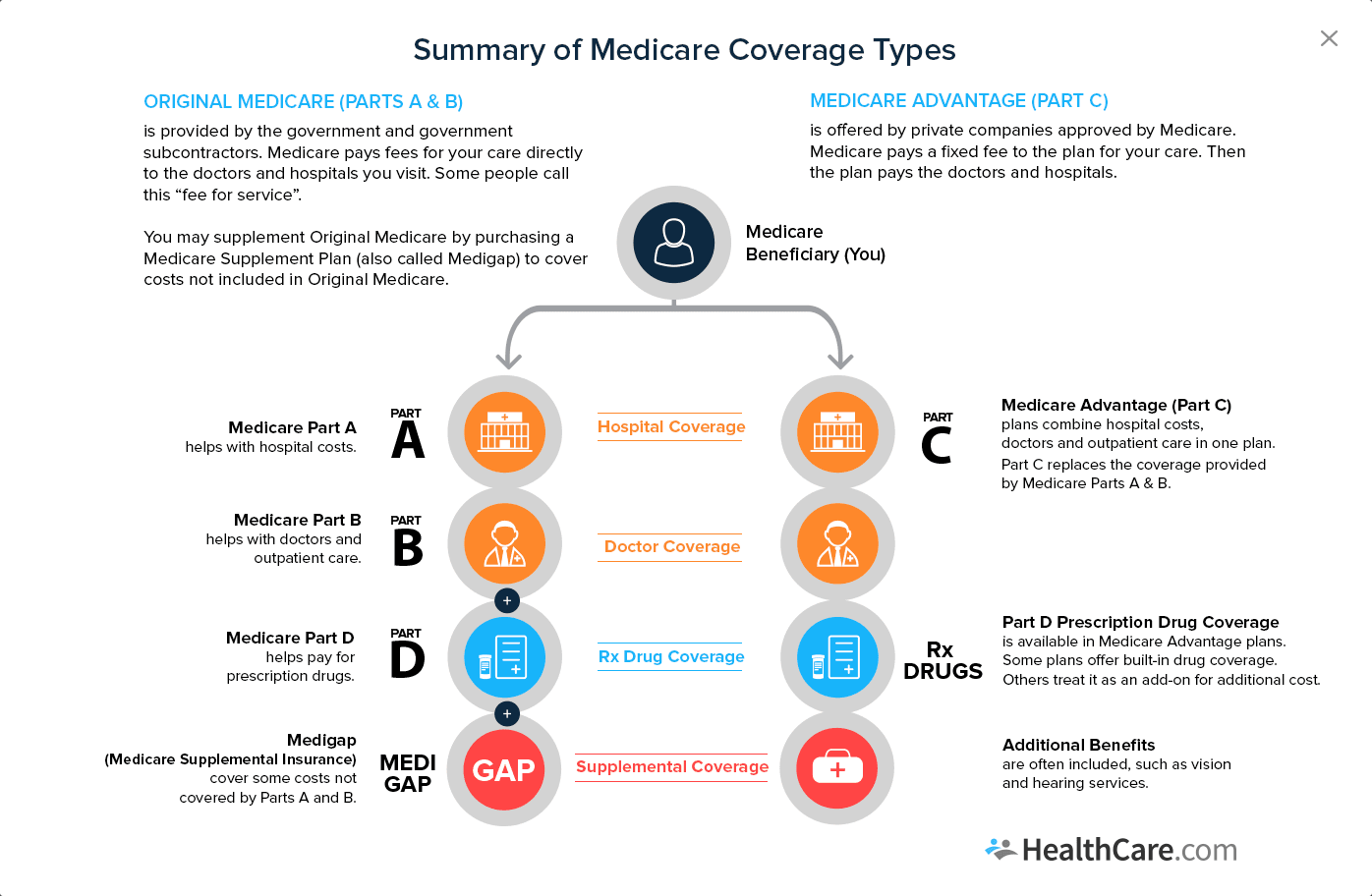
Original Medicare (Parts A and B) It has two parts: Part A hospital insurance and Part B medical insurance. Part A covers hospital stays and periods spent at skilled nursing facilities, lab tests an individual has performed, and hospice care. Part B covers doctor's office visits and home health care services.
Is there a copay with Medicaid Nevada?
There are no copays for covered services. Maintaining good health is important.
Can I use my Nevada Medicaid out of state?
Out-of-State Medical Coverage Medicaid/NCU will cover emergency services if you or your family are temporarily outside of the state, if the care provider agrees to participate in Medicaid/NCU and to bill us. Medicaid does not make payments directly to recipients for any services.
What is Medicare Advantage Plan?
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
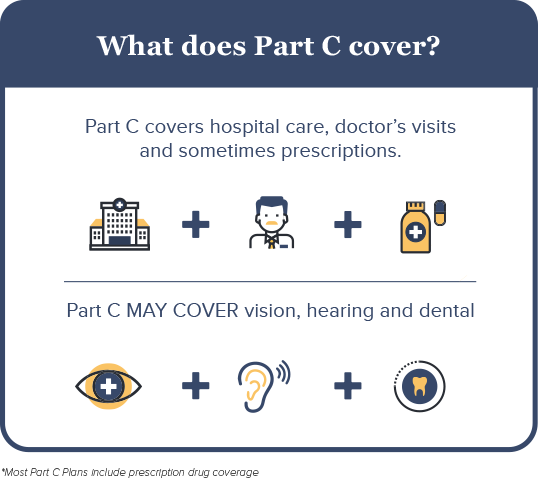
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Why is Medicare Advantage so popular?
Medicare Advantage is a popular health insurance option because it works like private health insurance for Medicare beneficiaries. In fact, according to the Centers for Medicare & Medicaid Services, more than 60 million Americans enrolled in Medicare in 2019. Of these Medicare enrollees, more than 37 percent were enrolled in a Medicare Advantage ...
How long does it take to sign up for Medicare?
Initial enrollment period. This is a 7-month window around your 65th birthday when you can sign up for Medicare. It begins 3 months before your birth month, includes the month of your birthday, and then extends 3 months after your birthday. During this time, you can enroll for all parts of Medicare without a penalty.
When is the open enrollment period for Medicare?
Open enrollment period (October 15–December 7). During this time, you can switch from original Medicare (parts A and B) to Part C (Medicare Advantage), or from Part C back to original Medicare. You can also switch Part C plans or add, remove, or change a Part D plan. General enrollment period (January 1–March 31).
Does Medicare Advantage cover prescription drugs?
Most Medicare Advantage plans include this coverage, which helps pay for the cost of your medications. Only certain types of prescription drugs are required to be covered under Part D, however — so you’ll want to make sure to check for coverage of your medications before enrolling in an Advantage plan.
Does Medicare Advantage have coinsurance?
Most Medicare Advantage plans charge a copayment or coinsurance amount for services rendered. These services could include a doctor’s office visit, specialist’s office visit, or even a prescription drug refill. Specific coinsurance and copayment amounts are set by the plan you’re enrolled in.
Does Medicare Advantage charge a premium?
Medicare Advantage plan costs. Medicare Advantage plans can charge a monthly premium that’s separate from the Part B premium. Other Advantage plans may be premium-free.
Does Medicare Advantage cover hospital services?
This includes any hospital services covered under Medicare Part A and any medical services covered under Medicare Part B. Some Medicare Advantage plans also cover additional healthcare needs, including: However, this coverage varies by plan, and each Medicare Advantage plan can choose what additional coverage to offer.