
How to bill Medicare for home health services. Medicare costs must be billed directly through Medicare. Providers must send the claim directly to Medicare, and then Medicare will reimburse directly to the service provider. The individual receiving the service will generally never see a bill from their provider.
Full Answer
How do I bill Medicare for home health care services?
Billing Medicare for Home Health Care Have the home health agency submit your claims to Medicare for payment. As with most other types of medical insurance, claims for payment for services rendered must be directly submitted to Medicare by the home health agency. Understand the bill/charges.
How does home health care work with Medicare?
Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home. Homemaker services. Custodial or personal care (like bathing, dressing, or using the bathroom), when this is the only care you need.
What is home health billing overview Biller?
1 Home Health Billing Overview biller has an important role in homecare: to ensure that the information submitted on claims is precise and appropriate. Medical billing translates all of the healthcare service provided to a patient into a billing
What is home health care?
What's home health care? Home health care is a wide range of health care services that can be given in your home for an illness or injury. Home health care is usually less expensive, more convenient, and just as effective as care you get in a hospital or skilled nursing facility (SNF). Examples of skilled home health services include:
What is the basic unit of payment for Medicare home health reimbursement?
ELEMENTS OF THE HH PPS The unit of payment under the HH PPS is a 60-day episode of care.
How does Medicare decide what to pay?
For most payment systems in traditional Medicare, Medicare determines a base rate for a specified unit of service, and then makes adjustments based on patients' clinical severity, selected policies, and geographic market area differences.
Does Medicare pay all your bills?
In most instances, Medicare pays 80% of the approved amount of doctor bills; you or your medigap plan pay the remaining 20%, if your doctor accepts assignment of that amount as the full amount of your bill. Most doctors who treat Medicare patients will accept assignment.
Who handles billing for Medicare?
Medicare Administrative Contractor (MAC)Billing for Medicare When a claim is sent to Medicare, it's processed by a Medicare Administrative Contractor (MAC). The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
Who determines Medicare reimbursement?
The Centers for Medicare and Medicaid Services (CMS) determines the final relative value unit (RVU) for each code, which is then multiplied by the annual conversion factor (a dollar amount) to yield the national average fee. Rates are adjusted according to geographic indices based on provider locality.
What is the 3 day rule for Medicare?
The 3-day rule requires the patient have a medically necessary 3-day-consecutive inpatient hospital stay. The 3-day-consecutive stay count doesn't include the day of discharge, or any pre-admission time spent in the ER or outpatient observation.
Does Medicare only pay 80%?
You will pay the Medicare Part B premium and share part of costs with Medicare for covered Part B health care services. Medicare Part B pays 80% of the cost for most outpatient care and services, and you pay 20%. For 2022, the standard monthly Part B premium is $170.10.
Can a doctor charge more than Medicare allows?
A doctor is allowed to charge up to 15% more than the allowed Medicare rate and STILL remain "in-network" with Medicare. Some doctors accept the Medicare rate while others choose to charge up to the 15% additional amount.
Can a Medicare patient be billed?
Balance billing is prohibited for Medicare-covered services in the Medicare Advantage program, except in the case of private fee-for-service plans. In traditional Medicare, the maximum that non-participating providers may charge for a Medicare-covered service is 115 percent of the discounted fee-schedule amount.
Can a patient bill Medicare directly?
If you have Original Medicare and a participating provider refuses to submit a claim, you can file a complaint with 1-800-MEDICARE. Regardless of whether or not the provider is required to file claims, you can submit the healthcare claims yourself.
How do I process a Medicare claim?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
Home Health Services Covered By Original Medicare
If youre eligible for Medicare-covered home health care, services covered may include:4
Additional Medicare Payment For Home Health Content
Beginning in January 2022, payment for Medicare Part B services provided by PTAs will be reduced by 15% due to a provision in the Balanced Budget Act of 2018.
What Does Homebound Mean
If a practice is considering seeing patients in their home instead of the clinic then you must be sure the patient meets the definition of homebound.
Split Percentage Payments And Requests For Anticipated Payments
Except for low utilization home health agencies, providers must submit an initial claim, also called a Request for Anticipated Payment or “no-pay RAP,” for periods of care on or after Jan. 1, 2021. This establishes the home health period of care and is required every 30 days thereafter.
A Home Health Agency Is An Agency Or Organization Which
Is primarily engaged in providing skilled nursing services and other therapeutic services Has policies established by a group of professionals , including one or more physicians and one or more registered professional nurses, to govern the services which it provides
Range Of Home Health Benefits
Either element of original Medicare Part A hospital insurance and/or Part B doctor visits and outpatient treatment might cover home care. Services include these:
Billing And Coding For Physician Home Visits
Physician home visits have begun making a comeback, according to a recent report from the Association of American Medical Colleges . With 80% of U.S. adults age 65+ having one or more chronic diseases, this is a welcome development.
How long does it take for a home health aide to be certified?
After a physician or allowed practitioner prescribes a home health plan of care, the HHA assesses the patient's condition and determines the skilled nursing care, therapy, medical social services and home health aide service needs, at the beginning of the 60-day certification period. The assessment must be done for each subsequent 60-day certification. A nurse or therapist from the HHA uses the Outcome and Assessment Information Set (OASIS) instrument to assess the patient's condition. (All HHAs have been using OASIS since July 19, 1999.)
When did the Home Health PPS rule become effective?
Effective October 1, 2000, the home health PPS (HH PPS) replaced the IPS for all home health agencies (HHAs). The PPS proposed rule was published on October 28, 1999, with a 60-day public comment period, and the final rule was published on July 3, 2000. Beginning in October 2000, HHAs were paid under the HH PPS for 60-day episodes ...
How are HHAs paid?
Beginning on January 1 2020, HHAs are paid a national, standardized 30-day period payment rate if a period of care meets a certain threshold of home health visits. This payment rate is adjusted for case-mix and geographic differences in wages. 30-day periods of care that do not meet the visit threshold are paid a per-visit payment rate for the discipline providing care. While the unit of payment for home health services is currently a 30-day period payment rate, there are no changes to timeframes for re-certifying eligibility and reviewing the home health plan of care, both of which will occur every 60-days (or in the case of updates to the plan of care, more often as the patient’s condition warrants).
What is included in the HH PPS?
For individuals under a home health plan of care, payment for all services (nursing, therapy, home health aides and medical social services) and routine and non-routine medical supplies, with the exception of certain injectable osteoporosis drugs, DME, and furnishing negative pressure wound therapy (NPWT) using a disposable device is included in the HH PPS base payment rates. HHAs must provide the covered home health services (except DME) either directly or under arrangement, and must bill for such covered home health services.
What is PPS in home health?
The Balanced Budget Act (BBA) of 1997, as amended by the Omnibus Consolidated and Emergency Supplemental Appropriations Act (OCESAA) of 1999, called for the development and implementation of a prospective payment system (PPS) for Medicare home health services.
Is telecommunications technology included in a home health plan?
In response CMS amended § 409.43 (a), allowing the use of telecommunications technology to be included as part of the home health plan of care, as long as the use of such technology does not substitute for an in-person visit ordered on the plan of care.
What is Medicare home health care?
One of the important provisions in Medicare coverage is home health care. This provision is intended to allow seniors to remain independent as long as possible. One study indicated that 90% of older Americans want to stay in their home as long as possible.
How to get home health insurance?
Before you can be approved for home health care coverage, your doctor must decide that you need home care whereby a plan for care is prepared. If your doctor doesn’t determine that home care is necessary for you, Medicare won’t pay for it.
What is Medicare for seniors?
Medicare was enacted in 1965 to expand the Social Security Act by providing a hospital insurance program with supplemental medical benefits and extended medical assistance for the aged, survivors, and disabled, in addition to improving state public assistance programs. The insurance program is for people who have reached the age of 65 or have particular disabilities and those in the end stages of renal disease. Today, older Americans rely on it to pay for about half of all of their medical costs. One of the important provisions in Medicare coverage is home health care. This provision is intended to allow seniors to remain independent as long as possible. One study indicated that 90% of older Americans want to stay in their home as long as possible. Home treatment has been found to be less expensive, convenient, and often as successful as nursing home or hospital care. With the high financial costs of medical care, it is important to know how Medicare is billed for home health services.
What age does Medicare cover home health?
The insurance program is for people who have reached the age of 65 or have particular disabilities and those in the end stages of renal disease. Today, older Americans rely on it to pay for about half of all of their medical costs. One of the important provisions in Medicare coverage is home health care.
What does it mean to be homebound on Medicare?
Being “homebound” means that you require help from another person or some type of medical equipment (like a wheelchair, walker, or crutches) to leave your home or that your doctor thinks your health might worsen if you leave your home.
What happens if you don't enroll in Medicare Part B?
If you do not choose to enroll in Medicare Part B when eligible, then the cost of enrolling later will increase.
How many parts does Medicare have?
Understand the types of Medicare coverage. Medicare has four parts, although Parts C and D are optional and are run through private insurance companies. Most people receive Medicare Part A upon reaching the age of 65.
What is home health records?
the medical records of the physician (at the acute or post-acute care facility) that recommended home health care (should the patient have been recommended for home health in this manner). these records must contain information showing the need for skilled services and the patient’s homebound status.
How often do you need to recertify for home health?
In order for patients to continue home health care, recertification is required every 60 days. Certification must: be signed and dated. indicate the need for further skilled home health services. estimate how much longer home health services will be needed. Note: A face-to-face encounter is NOT required for recertification.
What is the medical name for a patient who is under the care of a physician?
The patient must be under the care of a physician: MD (medical) DO (osteopathy), OR. Doctor of Pediatric Medicine. 2. The patient must be recommended for home health care by a physician.
Can home health information be incorporated into a comprehensive assessment?
Note: Information from the home heath agency can be incorporated (such as the patient’s comprehensive assessment), but it must be corroborated by other medical records.
Can a home health physician have a financial relationship with a recommending physician?
The home health physician cannot have a financial relationship with the home health recommending physician (i.e. the acute care, post-acute care, or certifying physician, nurse, or physician’s assistant)
What is the first step in home health billing?
The first step in home health billing is to discover if you can receive payments for your client. You need to get approved to receive payments from your client’s payer. Ex. Medicare, Medicaid, insurance companies, etc.
What is a contract for home health insurance?
A contract is a written agreement between a particular insurance company and a home health agency that outlines the covered services and the rates for which those services are covered. It also gives important information the agency needs on how to receive payments.
Why do you need to outsource billing?
Outsourcing can also help you to better manage the billing for your agency, allowing you to concentrate on patient care while leveraging the RCM partner’s talents and expertise.
What is clearinghouse in billing?
While agencies could log into each payer portal individually, a clearinghouse makes these transactions (and the follow up) easier on the biller.
What is EMR in healthcare?
Claims are sent to payers via an EMR/EHR. An EMR (electronic medical record) is software that keeps the patient’s medical record.
What happens after you get approved for home health insurance?
After becoming approved to receive payments, you will then begin the process of sending claims to the payers. Remember, claims are what you send to payers to bill for home health services rendered.
What is the term for tracking claims and receiving payments?
Keeping track of sending claims and receiving payments is known as revenue cycle management (RCM.)
What is the goal of home health care?
In general, the goal of home health care is to treat an illness or injury. Home health care helps you: Get better. Regain your independence. Become as self-sufficient as possible. Maintain your current condition or level of function. Slow decline. If you get your Medicare. benefits.
What does a home health agency do?
Once your doctor refers you for home health services, the home health agency will schedule an appointment and come to your home to talk to you about your needs and ask you some questions about your health. The home health agency staff will also talk to your doctor about your care and keep your doctor updated about your progress.
What to do if you have Medicare Supplement?
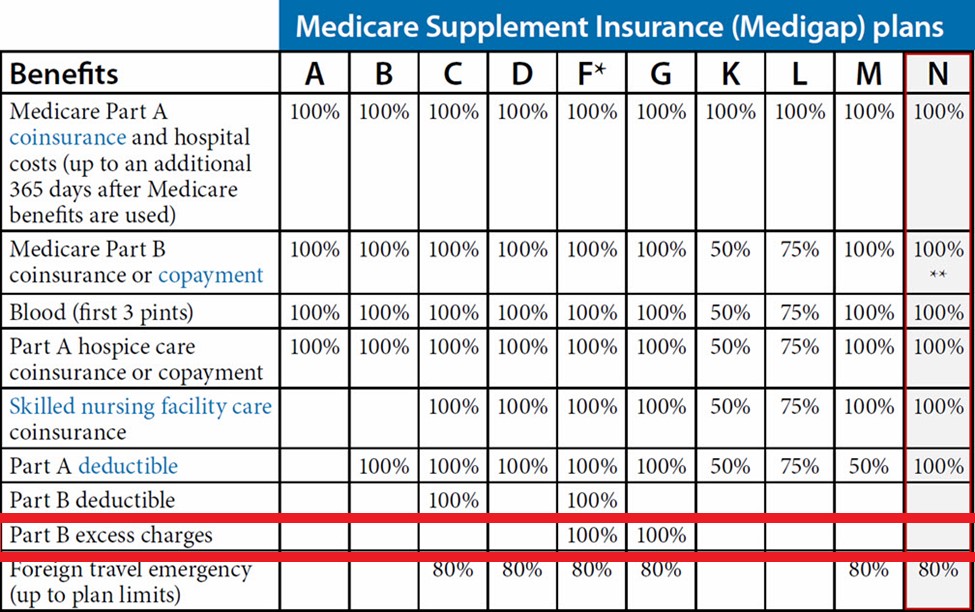
If you have a Medicare Supplement Insurance (Medigap) policy or other health insurance coverage, tell your doctor or other health care provider so your bills get paid correctly. If your doctor or referring health care provider decides you need home health care, they should give you a list of agencies that serve your area.
What are some examples of skilled home health services?
Examples of skilled home health services include: Wound care for pressure sores or a surgical wound. Patient and caregiver education. Intravenous or nutrition therapy . Injections. Monitoring serious illness and unstable health status. In general, the goal of home health care is to treat an illness or injury. Home health care helps you:
What does it mean to coordinate care?
Coordinate your care. This means they must communicate regularly with you, your doctor, and anyone else who gives you care.
