Some people are dual eligible for Medicare Advantage and Medicaid. If you’re enrolled in a Medicare Advantage plan that provides coverage for a treatment, service, or prescription drugs, your Medicare Advantage plan will cover it rather than Medicaid. Medicaid may also cover your Medicare Advantage premium if you have one.
Full Answer
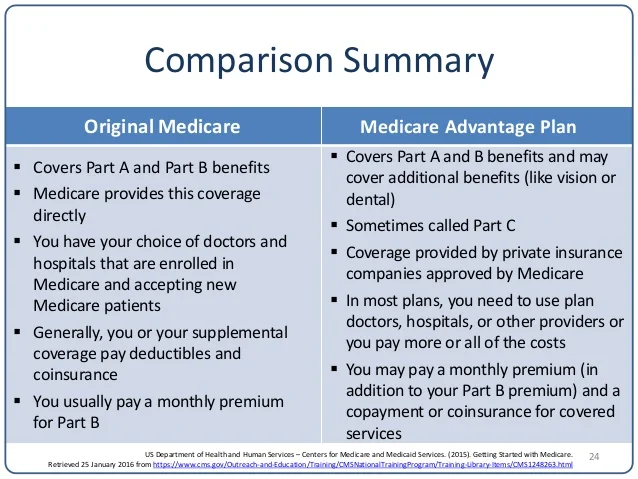
Does Medicare Advantage cost less than traditional Medicare?
UnitedHealth Group, for example, discovered that Medicare Advantage costs beneficiaries 40 percent less than traditional Medicare does.
Are prescription drugs covered in Medicare Advantage plans?
• Most Medicare Advantage Plans offer prescription drug coverage. Generally, a plan offered by a private company that contracts with Medicare to provide Part A and Part B benefits to people with Medicare who enroll in the plan. Medicare health plans include all Medicare Advantage Plans, Medicare Cost Plans, and Demonstration/Pilot Programs.
Do I need a Medicare supplement plan and Medicare Advantage?
You do not need and it is actually unethical and against Medicare guidelines to sell you a Medicare Supplement with a Medicare Advantage Plan. There are some policies that will help pay some of the out of pocket costs of a Medicare Advantage and in some cases they may be a good option. These are not Medicare Supplements.
Are Medicare Advantage plans the same as Medicare supplements?
No. Medicare Advantage plans are not the same as Medicare Supplements or Medigap policies. And here are a few key differences between the plans: Medigap policy design
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Can Medicare Advantage plans have a secondary?
When you have two types of health insurance – for example, a Medicare Advantage plan and an employer plan – generally one will be the primary payer and the other will be the secondary payer.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What is the highest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
Can you have Medicare and Medicaid at the same time?
Yes. A person can be eligible for both Medicaid and Medicare and receive benefits from both programs at the same time.
When a patient has Medicaid coverage in addition to other third party payer coverage Medicaid is always considered the?
For individuals who have Medicaid in addition to one or more commercial policy, Medicaid is, again, always the secondary payer.
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
Do Medicare Advantage plans cover prescription drugs?
Most Medicare Advantage Plans include prescription drug coverage (Part D). You can join a separate Medicare Prescription Drug Plan with certain types of plans that: Can't offer drug coverage (like Medicare Medical Savings Account plans) Choose not to offer drug coverage (like some Private Fee-for-Service plans)
Does Medicare Advantage cover dialysis?
Medicare Advantage, or Part C, is the alternative to original Medicare. This plan also covers dialysis, but many people will not qualify for this option.
Does Medicare Advantage change?
Medicare Advantage laws change from time to time. For instance, in September 2016, the House of Representatives passed a bill that allowed end-stage renal disease patients to participate in Part C.
Can you be a dual eligible for Medicare?
You may be a dual eligible, or someone who qualifies for Part C and Medicaid . In this case, the Medicaid may cover items that Medicare excludes. For example, most Part C plans also include Medicare Part D, or prescription drug coverage.
Does medicaid cover nursing home?
It can cover services like personal care or stays in a nursing home even if Medicare doesn’t. Medicaid will never pay first for services that other plans also cover.
Does medicaid pay first for services?
Medicaid will never pay first for services that other plans also cover. For instance, if your Medicare or employer-provided health insurance plan covers a specialist consultation that Medicaid includes, Medicaid won’t offset that cost.
Is Medicare Advantage still a form of Medicare?
Medicare Advantage Plans are still a form of Medicare. This means that they come complete with the rights you’d enjoy with Part A or Part B coverage. When you’re searching for quotes, you have to remember that Medicare Advantage enrollment is resetricted.
Does Medicaid cover cost sharing?
If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays.
Does Medicare cover medicaid?
If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover.
Is medicaid the primary or secondary insurance?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Does Medicaid offer care coordination?
Medicaid can offer care coordination: Some states require certain Medicaid beneficiaries to enroll in Medicaid private health plans, also known as Medicaid Managed Care (MMC) plans. These plans may offer optional enrollment into a Medicare Advantage Plan designed to better coordinate Medicare and Medicaid benefits.
What is the difference between Medicare and Medicaid?
When you have dual enrollment, Medicare is your primary insurance that covers any costs first. Medicaid is your secondary payer. Every state has different benefits for people who qualify under dual eligibility, so it’s important that you check with your local Medicaid office.
Does Medicaid cover dental care?
Medicaid can cover a large variety of healthcare services like behavioral health for substance abuse and mental health or dental care. Medicaid also has a robust cost-sharing program that helps cover any out of pocket costs for economically disadvantaged participants.
Can seniors get medicaid?
Many seniors in the United States have dual eligibility for Medicare and Medicaid benefits. Generally, this means that you have enrolled in Medicare, but that you qualify for Medicaid as well due to your income.
Is Medicaid a secondary insurance?
Secondary Insurance. Medicaid can fill in the gap as a secondary insurance to Medicare. Any services you have that Medicare pays for like hospital care, doctor’s visits, skilled nursing facility care, or home care, Medicare will pay for as the primary payer.
Does Medicaid pay cost sharing?
Medicaid can pay any cost-sharing charges you have. This help will depend on your income level. If the level is low enough, you could qualify for the Qualified Medicare Beneficiary (QMB) Medicare Savings Program. If you enroll in QMB, you won’t have to pay Medicare cost-sharing fees.
Does Medicare help with prescription drugs?
Prescription drugs are some of the biggest expenses people on Medicare face, and Medicaid can help. People who meet the eligibility requirements for dual enrollment in Medicare and Medicaid automatically get enrolled in the Extra Help program.
Which pays first, Medicare or Medicaid?
Medicare pays first, and. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid. pays second.
What is original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). or a.
Does Medicare have demonstration plans?
Medicare is working with some states and health plans to offer demonstration plans for certain people who have both Medicare and Medicaid and make it easier for them to get the services they need. They’re called Medicare-Medicaid Plans. These plans include drug coverage and are only in certain states.
Does Medicare Advantage cover hospice?
Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Most Medicare Advantage Plans offer prescription drug coverage. . If you have Medicare and full Medicaid, you'll get your Part D prescription drugs through Medicare.
Can you get medicaid if you have too much income?
Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid. The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid. In this case, you're eligible for Medicaid because you're considered "medically needy."
Can you spend down on medicaid?
Medicaid spenddown. Even if you have too much income to qualify, some states let you "spend down" to become eligible for Medicaid . The "spend down" process lets you subtract your medical expenses from your income to become eligible for Medicaid.
Does Medicare cover prescription drugs?
. Medicaid may still cover some drugs and other care that Medicare doesn’t cover.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.