To make matters worse, the Medicare Access and CHIP Reauthorization Act (MACRA) will shine an additional spotlight on coding accuracy and drive payments to physician practices. Denied Claims Denied claims put a major strain on revenue as they can delay or even stop payment to providers.
Full Answer
What happens when medical billing and coding errors affect reimbursement revenue?
When the government and insurance companies deny claims with medical billing and coding errors. Your EM group loses reimbursement revenue until you can correct and resubmit a clean claim.
Why is it so hard to be a medical code coder?
In healthcare, it’s a cause for angst throughout the revenue cycle, from patient care to billing and reimbursements. Medical coders have a never-ending task trying to keep up with changing laws, regulations, and medical codes, which makes it difficult to remain compliant.
What is medical coding and why is it important?
Medical coding is how your practice turns the services you provide into billable revenue. Each service corresponds to its own Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System codes. Claims for services are then submitted to insurance companies, Medicare, Medicaid, etc. with these codes.
How does medical coding impact revenue cycle performance?
In the new era of value-based reimbursements, never before has the process of medical coding had such a powerful impact on revenue cycle performance. Every stage of the healthcare revenue cycle has an impact on the next.

How does Medicare affect medical billing?
For the procedures they do accept assignment for, the billing is sent to Medicare just like full participants. However, for alternative procedures, the provider can bill up to 15 percent more than the Medicare approved amount, and the bill is sent directly to the patient who will seek reimbursement from Medicare.
Does Medicare require certified coders?
Yes, to be clear, Medicare does require its providers to hire certified coders.
How does Medicare affect reimbursement for healthcare services?
A: Medicare reimbursement refers to the payments that hospitals and physicians receive in return for services rendered to Medicare beneficiaries. The reimbursement rates for these services are set by Medicare, and are typically less than the amount billed or the amount that a private insurance company would pay.
How do medical billing and coding regulations affect reimbursement in a healthcare organization?
Affects Reimbursement: Improper coding leads to improper billing, which can directly impact a clinic's bottom line. Incorrectly down-coding a major procedure as something less accurate will result in lower reimbursements.
Who is responsible for coding?
In many private practices, the physician alone is responsible for selecting codes, based on the documentation, and this is done in the EMR, at the time the note is complete. In some academic practices or health care systems, and in groups that are employed by hospitals, all services are coded by a coder.
What CPT codes are not covered by Medicare?
Certain services are never considered for payment by Medicare. These include preventive examinations represented by CPT codes 99381-99397. Medicare only covers three immunizations (influenza, pneumonia, and hepatitis B) as prophylactic physician services.
How does Medicare reimbursement work for providers?
Traditional Medicare reimbursements Instead, the law states that providers must send the claim directly to Medicare. Medicare then reimburses the medical costs directly to the service provider. Usually, the insured person will not have to pay the bill for medical services upfront and then file for reimbursement.
Do doctors lose money on Medicare patients?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
What are Medicare reimbursement requirements?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
What are three consequences that can happen from inaccurate medical coding or billing?
Inaccurate medical coding will cause your reimbursements to get delayed, denied, or only partially paid. Build up a cache of delayed reimbursements and you'll have mounds of paperwork, stress, and lost revenue for your emergency medicine practice to deal with.
What are some consequences of incorrect coding?
Coding Errors May Lead to Fraud and Abuse Fines Practices and providers who have a history of coding mistakes may face fines and or federal penalties for fraud or abuse. The False Claims Act (FCA) is the enforcement tool used for false claims.
What department is responsible for ensuring compliance with billing and coding policies?
Be aware of changes to billing and coding standards and alerts and guidance from the Centers for Medicare & Medicaid Services (CMS), the Department of Health and Human Services Office of Inspector General, and private payers.
What is Medicare Part A?
Part A Medicare covers inpatient services provided in a hospital, as well as follow-up care in a skilled nursing facility (SNF). It also covers hospice care, home health care, and inpatient care in a religious non-medical healthcare institution. Medicare Part A holds patients responsible for a deductible, an out-of-pocket expense by patients, before benefits are paid directly by Medicare. This deductible is applicable for each benefit period, loosely defined as the course of treatment for a single medical condition. After the deductible is met, Part A covers all services for the first 60 days, after which the patient is responsible for a set co-payment for each additional day. Inpatient stays longer than 90 days incur higher co-payments. and coverage for inpatient care longer than 90 days is limited on a lifetime basis.
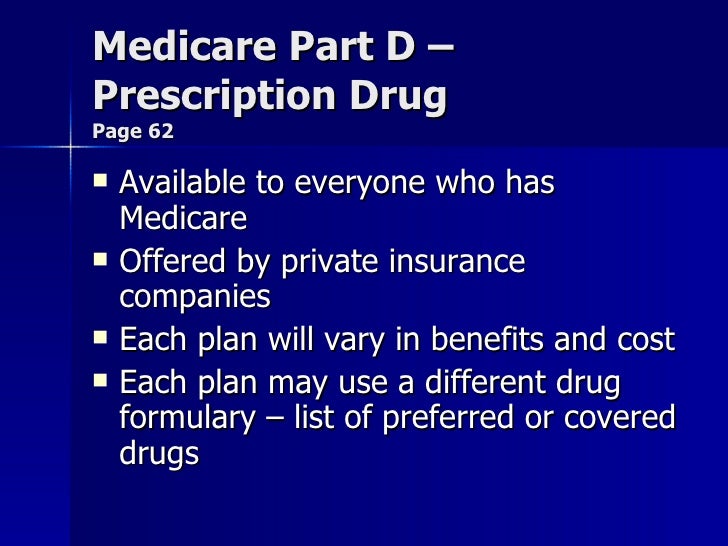
Does Medicare Part D cover prescription drugs?
Prescription drug coverage has been offered by Medicare Part D since 2006. CMS contracts with commercial third-party companies to provide prescription drug coverage, but there is no set standard of benefits as is the case with Parts A, B, or C. Part D contractors assemble formularies of covered drugs and can organized them by tiers. Tier I drugs may have no copay, while Tier III drugs impose a higher patient financial obligation than Tier II medications. Medical coding and billing for the Medicare Part D program is the profession of billers who work for pharmacies that serve outpatients.
What information does Medicare use for billing?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes. We can get almost all of this information from the superbill, which comes from the medical coder.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
Is it necessary to pay close attention to coding accuracy?
Paying close attention to coding accuracy is necessary — actually, imperative. Is it a pain? Is it expensive? Yes, but the longer a coding mistake is left undetected, the more effort it takes to correct. And ignoring new requirements under MACRA and other value-based reimbursement models can mean missed payments. Taking the time at the outset to evaluate and realign coding processes and staff will result in fewer denials and quicker, more accurate reimbursements — and, ultimately, a high-performing revenue cycle.
Can a wellness visit be miscoded?
A routine wellness visit that requires no copay could be miscoded as a problem-driven office visit , resulting in added fees for the patient and undue frustration.

What Are Medical Codes?
- Medical codes represent a whole host of information about your health: Diagnoses, treatment, medications, medical devices and more. Essentially, these codes translate complex information in your medical record into easily digestible data that payers and others can use to determine cost…
What Are Some Types of Medical Codes?
- Although there are various types of medical codes, the two main ones are diagnosis codes and procedure codes. For diagnoses, providers report ICD-10-CM diagnosis codes. ICD stands for the International Classification of Diseases. This disease classification is published and updated by the World Health Organization. The “10” refers to the version/edition of codes being used. The U…
How Can I Use Medical Codes?
- You can use medical codes to better understand your diagnoses and the services your doctor provides, to double-check your bills, to understand coverage, or to find the most affordable care. For example, if you see a medical code for a procedure you didn’t have, you can dispute the bill so you aren’t liable for payment. If you know the HCPCS code for a procedure you’re going to have, …