
The impact could be as simple as a reduction in documentation burden, which was the impetus behind new E/M coding practices in the new Medicare Physician Fee Schedule rule, or even revenue losses, which according to Evans, are frequently only seen by clinicians and their administrators after a lack of compliance has impacted their pocketbooks.
How does inaccurate medical coding affect reimbursement?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes. We can get almost all of this information from the superbill, which comes from the medical coder.
What are the most common mistakes medical coders make?
· They obtain claims from medical billing officials after a Medicare recipient has received care at a participating facility. This process generally takes around 30 days. The claims contain a series of relevant billing codes that are standardized across Medicare insurance providers. The process is the same as is used for private insurers.
How does Medicare billing work for providers?
Medicare Coding Guide Due to the Affordable Care Act (ACA), when physicians order certain evidence-based preventive services for patients, the insurance company may cover the cost of the service, with the patient having no cost-sharing responsibility (zero-dollar).
What is a medical biller or medical coder?
· Medicare also reliably follows the National Correct Coding Initiative (NCCI) edits, and it recognizes modifiers and the payments that link to them. Medicare, for the most part, lets providers know upfront what to expect.
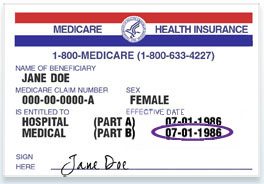
What are Medicare Parts A and B and how do they affect coding?
Part A provides inpatient/hospital coverage. Part B provides outpatient/medical coverage. Part C offers an alternate way to receive your Medicare benefits (see below for more information). Part D provides prescription drug coverage.
What are three consequences that can happen from inaccurate medical coding or billing?
Inaccurate medical coding will cause your reimbursements to get delayed, denied, or only partially paid. Build up a cache of delayed reimbursements and you'll have mounds of paperwork, stress, and lost revenue for your emergency medicine practice to deal with.
What are the cons of being a medical coder?
TOP CONS OF BEING A MEDICAL BILLER AND CODERYou must have a high school diploma or GED to be eligible for training programs. ... You must complete an accredited training program. ... You will need to get certified. ... You will have to renew your certification. ... You will have to learn a ton of new codes.More items...
What are some challenges to medical billing and coding?
4.03: Common Problems in Medical CodingNot Coding the Highest Level. ... Bad Documentation/Missing Documentation. ... Not Having Access to the Provider. ... Failing to Use Current/Updated Code Sets. ... Under- and Overcoding. ... Unbundling. ... Be Diligent. ... Communicate Often.More items...
Who is legally responsible of ensuring coding accuracy?
The medical provider or the coder? Legally, when a physician, physician assistant (PA) or nurse practitioner (NP) enroll in a Medicare, Medicaid or commercial insurance, the practitioner signs an agreement attesting that accurate claims will be submitted.
What are the two most common claim submission errors?
Common Errors when Submitting Claims:Wrong demographic information. It is a very common and basic issue that happens while submitting claims. ... Incorrect Provider Information on Claims. Incorrect provider information like address, NPI, etc. ... Wrong CPT Codes. ... Claim not filed on time.
Is Medical Coding a good career 2021?
The medical billing and coding career is a stable career and is growing quickly. It's becoming one of the most sought-after jobs in the healthcare industry due to the number of benefits it has.
Do medical coders have to talk on the phone?
Medical coders and billers work behind the scenes in office cubicles for healthcare organizations. Most of their day is spent sitting at a desk, typing on the computer, and speaking on the phone.
Are medical coders happy?
As it turns out, medical billing & coding technicians rate their career happiness 2.7 out of 5 stars which puts them in the bottom 14% of careers.
Is medical billing and coding going away?
As a result, technology advancements take jobs. There are thousands of articles on how artificial intelligence(AI) and robots will soon replace millions of jobs. I imagine you've seen some of these headlines too.
What is the future for medical coders?
The field of medical coding is growing at a much faster rate than average, with the employment of medical coders projected to grow 15 percent by 2024. The demand for skilled medical coders can only be seen to be increasing as they are key to the smooth functioning of the revenue cycle in the healthcare sector.
What aspects of coding and billing do you find most challenging?
Top 7 Challenges Medical Billing and Coding Experts Are FacingMedical Information Is Under Medical Privacy Laws. ... Getting to Know Medical Billing and Coding Systems. ... Possible Errors When Extracting Data From Medical Records. ... Technical Updates in Medical Billing and Coding. ... Medical Billing and Coding Involves Third-Parties.More items...•
What information does Medicare use for billing?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes. We can get almost all of this information from the superbill, which comes from the medical coder.
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
How much more can a provider bill than Medicare?
However, for alternative procedures, the provider can bill up to 15 percent more than the Medicare approved amount, and the bill is sent directly to the patient who will seek reimbursement from Medicare.
How long does it take for Medicare to process a claim?
They obtain claims from medical billing officials after a Medicare recipient has received care at a participating facility. This process generally takes around 30 days.
What is a CMS-1500?
Part B claims are filed using the CMS-1500 form. This is the standardized claim for that is used by healthcare providers that contract with Medicare. For providers that do not accept assignment for the specific procedure, Medicare will pay the patient directly for the reimbursement amount.
Is Medicare Part C billed directly?
Medicare Part C is also known as Medicare Advantage. These plans are offered through private insurers, so the billing is not filed directly though Medicare.
Can you opt out of Medicare?
Some providers may completely opt out of Medicare, meaning that they are not able to bill Medicare for any services. This means that the patient is responsible for paying for all costs out of pocket. In addition, there is no limit to the amount that the provider can charge for a procedure.
Is Medicare a federal or state insurance?
Medicare is a federally funded health insurance option, and since Medicare is responsible for reimbursing all participating healthcare facilities, the billing process is very particular.
Who insures resequencing of POA indicators?
The provider, a provider's billing office, third party billing agents and anyone else involved in the transmission of this data shall insure that any resequencing of diagnosis codes prior to transmission to CMS also includes a resequencing of the POA Indicators.
Does CMS pay for POA indicator?
CMS will not pay the CC/MCC DRG for those selected HACs that are coded as "1" for the POA Indicator. The “1” POA Indicator should not be applied to any codes on the HAC list. For a complete list of codes on the POA exempt list, see the Official Coding Guidelines for ICD-10-CM.
What is Medicare Part A?
Part A Medicare covers inpatient services provided in a hospital, as well as follow-up care in a skilled nursing facility (SNF). It also covers hospice care, home health care, and inpatient care in a religious non-medical healthcare institution. Medicare Part A holds patients responsible for a deductible, an out-of-pocket expense by patients, before benefits are paid directly by Medicare. This deductible is applicable for each benefit period, loosely defined as the course of treatment for a single medical condition. After the deductible is met, Part A covers all services for the first 60 days, after which the patient is responsible for a set co-payment for each additional day. Inpatient stays longer than 90 days incur higher co-payments. and coverage for inpatient care longer than 90 days is limited on a lifetime basis.
Does Medicare Part D cover prescription drugs?
Prescription drug coverage has been offered by Medicare Part D since 2006. CMS contracts with commercial third-party companies to provide prescription drug coverage, but there is no set standard of benefits as is the case with Parts A, B, or C. Part D contractors assemble formularies of covered drugs and can organized them by tiers. Tier I drugs may have no copay, while Tier III drugs impose a higher patient financial obligation than Tier II medications. Medical coding and billing for the Medicare Part D program is the profession of billers who work for pharmacies that serve outpatients.
What are the two categories of medical coding errors?
When it comes to medical coding errors, they fall into the broad categories of “fraud” and “abuse.”
What does modifier 22 mean in a medical procedure?
In such a case, appending the modifier 22 to the code used to report the removal can indicate the increased complexity of the service.
What is NCCI edit?
Failing to check National Correct Coding Initiative (NCCI) edits when reporting multiple codes. The Centers for Medicare & Medicaid Services developed the NCCI to help ensure correct coding methods were followed and avoid inappropriate payments for Medicare Part B claims. These are automated prepayment edits that are “reached by analyzing every pair of codes billed for the same patient on the same service date by the same provider to see if an edit exists in the NCCI,” the AMA’s text notes. “If there is an NCCI edit, one of the codes is denied.” NCCI edits will also typically provide a list of CPT modifiers available that may be used to override the denial. In certain cases, clear direction is stated that no modifier may be used to override the denial.
What is unbundling CPT?
Unbundling refers to using multiple CPT codes for the individual parts of the procedure, either due to misunderstanding or in an effort to increase payment. Upcoding. Example: You are a physician in a specialty, such as oncology, that often has highly complex patients.
Can you report an injection code without documentation?
Improper reporting of injection codes. Only report one code for the entire session during which the injections take place instead of multiple units of a code. Reporting unlisted codes without documentation. If you must use an unlisted code to properly bill for a service, you must properly document it.
Can you bill for a skin repair and excision?
Example: You bill for a lesion excision and skin repair on a single service date. But CPT coding guidelines say simple repairs are included in the excision codes, so separately coding the repair would be wrong and generate an NCCI edit. But if the repair was performed on a different site from where the lesion was removed, it is appropriate to bill for both and append a modifier to let the payer know the procedure was indeed separate from the excision.
How does coding errors affect emergency medicine?
When the government and insurance companies deny claims with medical billing and coding errors. Your EM group loses reimbursement revenue until you can correct and resubmit a clean claim.
What happens if you have inaccurate medical coding?
Inaccurate medical coding will cause your reimbursements to get delayed, denied, or only partially paid. Build up a cache of delayed reimbursements and you’ll have mounds of paperwork, stress, and lost revenue for your emergency medicine practice to deal with.
Why are emergency medical claims rejected?
Claims are most often rejected due to billing and coding errors. But once your team fixes those errors, you can resubmit a clean claim for payment again. Your emergency medicine group will notice a boost in revenue by following up on your medical denials.
What are the consequences of upcoding?
But the more serious consequences of upcoding and acts of medical abuse and fraud could have your group facing federal penalties and expensive fines.
Why is it important to continue training for your billing team?
Additionally, it’s imperative to continue training for your team since medical billing codes change all the time. This will help them stay up to date on the latest and most specific codes to use. And it will also lower your denial rate.
What happens if you code incorrectly?
Inaccurate coding leads to inaccurate reimbursement, and in some cases, legal action against your practice. The best way to avoid the consequences of medical coding and billing errors is to partner with a team of experts that specializes in emergency medicine revenue cycle management.
What are the consequences of medical coding errors?
Medical coding errors lead to higher claim denials, loss of revenue, and federal penalties, fines, and imprisonment. Learn how to protect your emergency medicine group from ED coding errors now:
How does medical coding affect revenue?
It’s simple: Medical coders translate medical record documentation into the alphanumeric language of which healthcare data consists. Quality and accuracy in medical coding doesn’t just affect the revenue cycle—although that is an important part of the claims process—it also directly affects the quality of healthcare data.
How does incomplete diagnosis affect patient care?
Incorrect and incomplete diagnosis coding can adversely affect patient care by indicating the presence of disease where it does not exist, and not revealing the presence of a disease where it does exist. This can affect the accuracy of quality measurements such as the Healthcare Effectiveness Data and Information Set.
How does quality affect reimbursement?
The quality of claims data can positively or negatively affect provider reimbursement (programs such as CMS’ Physician Quality Reporting System (PQRS) or other pay-for-performance measures), or cause incorrect hospital diagnosis-related group (DRG) payment due to improper diagnosis code sequencing . Incorrect and incomplete diagnosis coding can adversely affect patient care by indicating the presence of disease where it does not exist, and not revealing the presence of a disease where it does exist. This can affect the accuracy of quality measurements such as the Healthcare Effectiveness Data and Information Set. Ultimately, it can lead to patients not being identified for case management where they may need extra support.
What is medical claim?
Medical claims are a smorgasbord of information. They contain member and provider demographics, dates, diagnoses, procedures, medications, and much more. Much of these data are protected health information as defined by HIPAA, and law prohibits release of information that can identify a specific person.
Why are health data used in public health?
Healthcare data have been used in public health for many years—hundreds, in fact! During the Black Death in London, England in 1664-1665, weekly Bills of Mortality were posted in public places to help warn citizens about how the plague was spreading within their communities. Today, such agencies as the Centers for Disease Control and Prevention and World Health Organization continue to gather and publish information about new and emerging infectious diseases, as well as more common infections such as influenza.
What is healthcare data analysis?
Healthcare data analyses are not limited to acute and infectious disease. Many chronic diseases, such as asthma and diabetes, are carefully studied and tracked. In fact, if you have a chronic disease, you may be enrolled in a disease management program through your employer and health insurer. Look to Claims for Data Analysis.
