Here are more ways that Medicare and Medicaid can work together:
- Medicaid can provide premium assistance, where you will automatically be enrolled in a Medicare Savings Program (MSP). ...
- Medicaid can provide cost-sharing assistance depending on your income. ...
- Medicaid can provide prescription drug assistance for d ually eligible beneficiaries, where they are automatically enrolled in the Extra Help program
Full Answer
How to combine Medicare and Medicaid to save money?
You should have the following information ready when you apply:
- Full legal name, Date of Birth, Social Security Number, Citizenship or Immigration Status for you and anyone in your household who is applying for health care coverage.
- Most recent federal tax filing information (if available).
- Job and income information for members of your household for the month prior or the current month. ...
What are the pros and cons of Medicare and Medicaid?
Pros And Cons Of Medicaid In America. 862 Words 4 Pages. In the United States, Medicare is the program supports people over age 65 with medical care. It also provides support for persons with certain disabilities and people of all ages who have kidney failure. ... Medicare and Medicaid are two government funded health insurance options for ...
How does Medicare and group health insurance work together?
Some people who continue to work past 65 may also have group health plan benefits through their employer. Because of this, it’s possible to have both Medicare and a group health plan after age 65. For these individuals, Medicare and employer insurance can work together to ensure that healthcare needs and costs are covered.
Who really pays for Medicaid?
Who Really Pays For Health Care Might Surprise You
- Before Obamacare we had a free-market health-care system. Government has been part of the business of medicine at least since the 1940s, when Washington began appropriating billions to build private ...
- I fully paid for Medicare through taxes deducted from my salary. ...
- Premiums from my paycheck fund my company health plan. Probably not entirely. ...

When can a patient have both Medicare and Medicaid?
Some Americans qualify for both Medicare and Medicaid, and when this happens, it usually means they don't have any out-of-pocket healthcare costs. Beneficiaries with Medicare and Medicaid are known as dual eligibles – and account for about 20 percent of Medicare beneficiaries (about 12.3 million people).
What plan provides both Medicare and Medicaid coverage?
UnitedHealthcare Connected® for One Care (Medicare-Medicaid Plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
When the patient is covered by both Medicare and Medicaid what would be the order of reimbursement?
gov . Medicare pays first, and Medicaid pays second . If the employer has 20 or more employees, then the group health plan pays first, and Medicare pays second .
What is the lowest income to qualify for Medicaid?
Federal Poverty Level thresholds to qualify for Medicaid The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.
What are the disadvantages of Medicaid?
Disadvantages of Medicaid They will have a decreased financial ability to opt for elective treatments, and they may not be able to pay for top brand drugs or other medical aids. Another financial concern is that medical practices cannot charge a fee when Medicaid patients miss appointments.
What is not covered by Medicaid?
Medicaid is not required to provide coverage for private nursing or for caregiving services provided by a household member. Things like bandages, adult diapers and other disposables are also not usually covered, and neither is cosmetic surgery or other elective procedures.
When a patient is covered through Medicare and Medicaid which coverage is primary?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors' visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Does Medicaid pay Medicare premiums?
Medicaid pays Part A (if any) and Part B premiums. Medicaid is liable for Medicare deductibles, coinsurance, and copayments for Medicare-covered items and services. Even if Medicaid doesn't fully cover these charges, the QMB isn't liable for them.
Do doctors treat Medicare patients differently?
Many doctors try to help out patients who can't afford to pay the full amount for an office visit or the copay for a pricey medication. Now along comes a study suggesting that physicians in one Texas community treat patients differently, depending on whether they are on Medicare or have private insurance.
How do I qualify for dual Medicare and Medicaid?
Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. To be considered dually eligible, persons must be enrolled in Medicare Part A (hospital insurance), and / or Medicare Part B (medical insurance).
What is considered low income for a single person in 2021?
2021 POVERTY GUIDELINES FOR THE 48 CONTIGUOUS STATES AND THE DISTRICT OF COLUMBIAPersons in family/householdPoverty guideline1$12,8802$17,4203$21,9604$26,5005 more rows
What is the medical income limit for 2021?
A single adult can earn up to $17,775 in 2021 and still qualify for Medi-Cal. A single adult with one dependent can earn up to $46,338 annually and the child will still be eligible for Medi-Cal.
What’s the Difference Between Medicaid and Medicare?
Medicaid is an assistance program. For anyone that qualifies, Medicaid enrollment is open the entire year. Most Medicaid enrollees lack access to a...
Can You Have Medicare and Medicaid?
The short answer is yes. If you receive coverage from both Medicaid and Medicare, you’re a “dually eligible beneficiary.” If you are dual eligible,...
What is Covered?
Your state determines Medicaid services. Original Medicare coverage includes Part A (hospital) and Part B (medical). It is important to know that y...
What are my Costs with dual eligibility?
Dual eligibility can limit individual costs for beneficiaries. For those with Medicare, state Medicaid programs will pay for many cost-sharing and...
Can I change plans if I’m dual eligible?
Yes. If you have Medicare and full Medicaid coverage, you can change plans once per calendar quarter for the first three quarters. The new plan wil...
Where do I apply for Medicaid?
You can apply through your state health department’s website, over the phone or even by mail.
What is the history of Medicaid, and how is it tied to Medicare?
Medicaid and Medicare share a birthday, both born on July 30, 1965, when President Lyndon B. Johnson signed legislation creating a pair of programs...
What is integrated care?
When care is provided to Medicare-Medicaid beneficiaries through an “integrated” care model, the beneficiary can get the full array of Medicaid and Medicare benefits through a single delivery system. This approach can improve care coordination and quality, and reduce administrative burdens. One such model is the Program for All-Inclusive Care ...
Can Medicare beneficiaries get help with out of pocket medical expenses?
Medicare beneficiaries who have limited income and resources may get help paying for their Medicare premiums and out-of-pocket medical expenses from Medicaid.
How does Medicare and Medicaid work together?
Medicare and Medicaid work together to cover costs, including long-term services. If you do not have full Medicaid benefits, Medicare Savings Programs (MSP) may help cover some of those costs: Qualified Medicare Beneficiary (QMB) Program. Specified Low-Income Medicare Beneficiary (SLMB) program.
What is Medicare Part A?
Dual-eligible beneficiaries can have: Medicare Part A. Medicare Part A, also called "hospital insurance, " covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare. Medicare Part B.
What is partial coverage?
Partial coverage may include Medicaid coverage for expenses like Medicare premiums. A premium is a fee you pay to your insurance company for health plan coverage. This is usually a monthly cost. A deductible is an amount you pay out of pocket before your insurance company covers its portion of your medical bills.
What are the benefits of Medicare Part A?
Dual-eligible beneficiaries can have: 1 Medicare Part A#N#Medicare Part A, also called "hospital insurance," covers the care you receive while admitted to the hospital, skilled nursing facility, or other inpatient services. Medicare Part A is part of Original Medicare. 2 Medicare Part B#N#Medicare Part B is the portion of Medicare that covers your medical expenses. Sometimes called "medical insurance," Part B helps pay for the Medicare-approved services you receive. 3 Both Part A and Part B 4 Full Medicaid benefits 5 State Medicare Savings Programs
How long does it take to get medicaid after a disability?
An individual under 65 receiving Social Security Disability Insurance can have Medicaid and later enroll in Medicare after 24 months of receiving Social Security Disability benefits, or upon reaching the age of 65.
What is dual eligibility for medicaid?
Medicaid is a state-based health insurance program for individuals that qualify. Unlike Medicare, Medicaid does not have age restrictions for members. , you are dual-eligible. Dual-eligibility allows beneficiaries to combine Medicare and Medicaid benefits to expand coverage ...
What is full coverage Medicare?
. Full coverage consists of the same benefits as partial coverage and may include services not covered by Medicare like long-term care.
Does Medicaid cover cost sharing?
If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays.
Does Medicare cover medicaid?
If you qualify for a Medicaid program, it may help pay for costs and services that Medicare does not cover.
Is medicaid the primary or secondary insurance?
Medicaid can provide secondary insurance: For services covered by Medicare and Medicaid (such as doctors’ visits, hospital care, home care, and skilled nursing facility care), Medicare is the primary payer. Medicaid is the payer of last resort, meaning it always pays last.
Does Medicaid offer care coordination?
Medicaid can offer care coordination: Some states require certain Medicaid beneficiaries to enroll in Medicaid private health plans, also known as Medicaid Managed Care (MMC) plans. These plans may offer optional enrollment into a Medicare Advantage Plan designed to better coordinate Medicare and Medicaid benefits.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
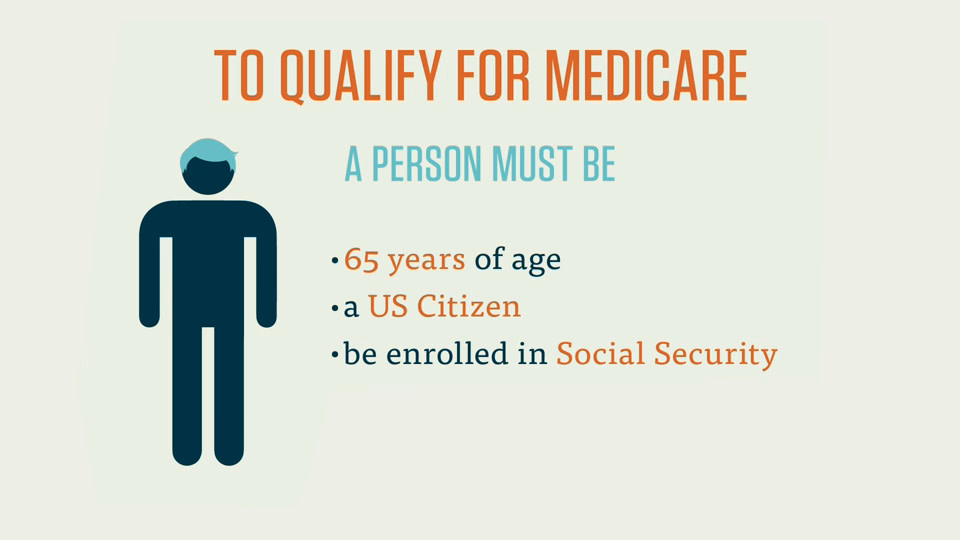
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
Does Medicaid cover nursing home care?
Medicaid also pays for nursing home care, and often limited personal care assistance in one’s home. While some states offer long-term care and supports in the home and community thorough their state Medicaid program, many states offer these supports via 1915 (c) Medicaid waivers.
Is Medicaid a federal program?
Eligibility requirements for Medicaid are not as straightforward as are the requirements for Medicare. This is because, as mentioned previously, Medicaid is a federal and state program. While the parameters of the program are federally set, each state can set their own rules within these guidelines. Even within the same state, there are a variety of pathways to Medicaid that have their own eligibility requirements.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens when there is more than one payer?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
How much does Medicare pay for each prescription?
You pay $1-3 for each prescription per month. Covers your Medicare Part A and B copayment. Provides additional Medi-Cal benefits such as medical transportation, incontinence supplies, and personal care in a nursing home.
What is the second option for Medicare?
Option 2: Medicare Advantage Plan + Medi-Cal health plan. You enroll into a Medicare Advantage managed care plan; Your Medicare Parts A, B and D benefits are assigned to the plan; While you are in the plan, you must use plan providers to obtain medical care; You pay $1-3 for each prescription per month.
What are the benefits not covered by Medicare?
Provides benefits not covered by Medicare such as –. Hearing aids. Incontinence supplies. Dental services. Vision care. Medical transportation. In Home Supportive Services care at home. Nursing home care. There are different ways to use your Medicare and Medi-Cal benefits.
What is Medi-Cal insurance?
Medi-Cal is your secondary insurance. Medi-Cal closes the gaps in Medicare coverage and provides additional benefits not covered by your Medicare.
Does Medicare Part D affect your ability to use Medicare?
You enroll into a Medicare Part D plan that only provides drug coverage you pay $1-3 for each prescription per month. Your Part D plan does not affect your ability to use your Medicare. Covers your Medicare Part A and B copayments. Provides additional Medi-Cal benefits such as medical ...
Can I get medical care outside of Medi-Cal?
You can receive medical services outside your Cal MediConnect plan only for emergency care or if you need urgent care outside your service area. The Cal MediConnect plan may provide additional benefits such as dental services that are not covered by Medi-Cal.
Do you have to enroll in a Medi-Cal plan if you have Medicare?
Your enrollment in a Medi-Cal health plan will not limit your ability to use your Medicare coverage. Your Medi-Cal health plan will only manage most of your Medi-Cal benefits.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is tricare medical?
Published by: Medicare Made Clear. TRICARE® is the health care program that serves uniformed service members, retirees and their families worldwide. Medicare is a federal health care program for U.S. citizens age 65 and older, under age 65 with certain disabilities and those who have end-stage renal disease. You may be eligible for both TRICARE and ...
Does Tricare work with Medicare?
TRICARE For Life may work with Original Medicare (Parts A & B), a Medicare Advantage plan or a Part D prescription drug plan. However, you may want to think carefully about whether you need Medicare drug coverage. TRICARE For Life includes a prescription drug benefit, so you may not need Part D.
Do you have to have Medicare Part B to get tricare?
Most people with TRICARE, who become Medicare eligible and get Medicare Part A, must also have Medicare Part B to be able to remain eligible. Part D is not required to maintain eligibility.
Is tricare for life a creditable benefit?
This allows you to sign up without paying the Part D late enrollment penalty. When you have TRICARE For Life and Medicare, you won’t receive a TRICARE wallet card.