How do I find out if my doctor accepts Medicare assignment?
11-characters in length. Made up only of numbers and uppercase letters (no special characters); if you use lowercase letters, our system will convert them to uppercase letters. The MBI doesn’t use the letters S, L, O, I, B, and Z to avoid confusion between some letters and numbers (e.g., between “0” and “O”). Learn about and use our ...
What is a Medicare assignment?
Jul 16, 2021 · Medicare assignment is a fee schedule agreement between Medicare and a doctor. Accepting assignment means your doctor agrees to the payment terms of Medicare. Doctors …
How many characters are there in a Medicare number?
Jan 12, 2022 · Generally, a provider or supplier will be assigned to the Medicare Administrative Contractor (MAC) that covers the state where the provider or supplier is located. The Center for …
How do I Find my Medicare group number?
Apr 26, 2022 · Original Medicare is not a group policy, therefore there is no “group” in which to belong. Instead, you will see an 11-digit alphanumeric on your card which is used to identify …
How is a Medicare number determined?
How is a Medicare number formatted?
Are Medicare numbers unique?
What does Medicare number mean?
What is the new Medicare ID format?
When did Medicare ID numbers change?
Do Medicare numbers change every year?
Can your Medicare number change?
Why would a Medicare MBI number change?
How do I find my Medicare number on my Social Security?
What does C1 mean after a Social Security number?
| Code | Identification |
|---|---|
| C1-C9 | Child – Includes minor, student or disabled child |
| D | Aged Widow, age 60 or over |
| D1 | Aged widower, age 60 or over |
| D2 | Aged widow (2nd claimant) |
What does it mean to accept Medicare assignment?
Accepting assignment means your doctor agrees to the payment terms of Medicare. Doctors who accept Medicare are either a participating doctor, non-participating doctor, or they opt-out. When it comes to Medicare’s network, it’s defined in one of three ways. Participating Provider: Providers that accept Medicare Assignment agree to accept ...
What does "non-participating provider" mean?
Participating Provider: Providers that accept Medicare Assignment agree to accept what Medicare establishes per procedure, or visit, as payment in full. Non-Participating Provider: Providers in this category do accept Medicare, but do not accept the amount Medicare says a procedure or visit should cost. These providers reserve the right ...
What is assignment of benefits?
The assignment of benefits is when the insured authorizes Medicare to reimburse the provider directly. In return, the provider agrees to accept the Medicare charge as the full charge for services. Non-participating providers can accept assignments on an individual claims basis. On item 27 of the CMS-1500 claim form non participating doctors need ...
Can a doctor opt out of Medicare?
When it comes to Medicare assignments, doctors can choose to opt-out or not participate. Doctors that accept Medicare will accept Medigap coverage. Not all doctors that accept Medicare will accept a Medicare Advantage plan.
What is Medicare Advantage Plan?
Unlike a Medicare Supplement, a Medicare Advantage Plan replaces your Original Medicare. Your health coverage is the insurance company and you don’t have the freedom to simply go to any doctor. Advantage plans are subject to plan networks and rules for services.
What is a private contract with Medicare?
A Medicare private contract is for doctors that opt-out of Medicare payment terms. Once you sign a contract, it means that you accept the full amount on your own, and Medicare can’t reimburse you. Signing such a contract is giving up your right to use Medicare for your health purposes.
Does Medigap cover excess charges?
Not all Medigap plans will cover excess charges, but some do. Give us a call to see what Medigap plans in your area will cover excess charges. If you prefer, fill out our online rate form, and one of our Medicare agents will call you with your rates.
Provider Nomination and the Geographic Assignment Rule
Section 911 (b) of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), Public Law 108-173, repealed the provider nomination provisions formerly found in Section 1816 of the Title XVIII of the Social Security Act and replaced it with the Geographic Assignment Rule.
Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) Rule
Each DMEPOS supplier submits claims to the DME MAC contracted by CMS to administer DMEPOS claims for the geographic locale in which the beneficiary resides permanently. Learn more about the current DME MAC jurisdictions and view the corresponding map at Who are the MACs.
Specialty Providers and Demonstrations Rule
Specialty providers and providers involved with certain demonstrations will submit claims to a specific MAC designated by CMS. Learn more about a specific A/B MAC or DME MAC and view the corresponding maps at Who are the MACs.
Railroad Retirement Beneficiaries Entitled to Medicare Rule
Physicians and other suppliers (except for DMEPOS suppliers) will continue to enroll with and bill the contractor designated by the Railroad Retirement Board for Part B services furnished to their beneficiaries.
Qualified Chains Rule
The Geographic Assignment Rule states that generally, a provider or supplier will be assigned to the MAC that covers the state where the provider or supplier is located. However, it does provide an exception for qualified chains.
Out-of-Jurisdiction Providers (OJP) Rule
An OJP is a provider that is not currently assigned to an A/B MAC in accordance with the geographic assignment rule and the qualified chain exception. For example, a hospital not part of a qualified chain located in Maine, but currently assigned to the A/B MAC in Jurisdiction F would be an OJP.
What Is a Health Insurance Group Number?
A group number is assigned to the employer or other group that sponsors an insurance plan for its employees or other individuals covered by the group plan. Each member of the group will share the same group number, but each person will have their own unique member number.
Does Private Medicare Have Group Numbers?
Original Medicare is not group coverage and therefore has no corresponding group number. But private Medicare plans may have a group number associated with the plan.
What Is a Medicare Group?
While Original Medicare is not group coverage, there are some group Medicare insurance plans available from private insurance companies.
What are the different parts of Medicare?
What the letters mean for the parts of Medicare 1 Medicare Part A is hospital insurance and provides coverage for inpatient stays at hospitals and skilled nursing care facilities, among other inpatient services. 2 Medicare Part B is medical insurance and provides coverage for outpatient doctor’s appointments and medical devices. 3 Medicare Part C, also known as Medicare Advantage, provides coverage for everything found in Part A and Part B through one plan provided by a private insurer.#N#Many Medicare Advantage plans may also cover additional benefits not covered by Part A and Part B, such as prescription drugs, dental, vision, hearing, wellness programs like SilverSneakers and more. 4 Medicare Part D provides coverage exclusively for prescription drugs.#N#You can visit MyRxPlans.com to compare Part D plans available where you live and enroll in a Medicare prescription drug plan online in as little as 10 minutes. 1
How many characters are in a Medicare card?
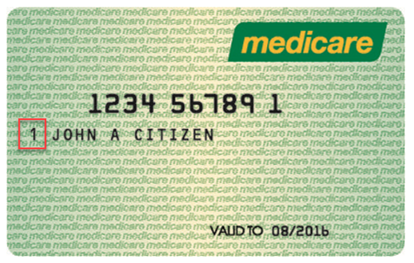
The Medicare number displayed on Medicare cards (known as an MBI, or Medicare Beneficiary Identifier) is 11 characters long: The 2nd, 5th, 8th and 9th characters are always a letter, and the 3rd and 6th characters are sometimes a letter.
What is Medicare Part B?
Medicare Part B is medical insurance and provides coverage for outpatient doctor’s appointments and medical devices. Medicare Part C, also known as Medicare Advantage, provides coverage for everything found in Part A and Part B through one plan provided by a private insurer.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance, also called Medigap, uses a letter system to identify its plans. Medicare Supplement Insurance is used in conjunction with Part A and Part B of Medicare to provide coverage for certain out-of-pocket expenses like some Medicare deductibles and coinsurance.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a multi-employer plan have?
At least one or more of the other employers has 20 or more employees.
What does assignment mean in Medicare?
Assignment means that your doctor, provider, or supplier agrees (or is required by law) to accept the Medicare-approved amount as full payment for covered services.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. and. coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
What is coinsurance in Medicare?
coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%). amount and usually wait for Medicare to pay its share before asking you to pay your share. They have to submit your.
What is the limiting charge for Medicare?
The limiting charge is 15% over Medicare's approved amount. The limiting charge only applies to certain services and doesn't apply to supplies or equipment. ". The provider can only charge you up to 15% over the amount that non-participating providers are paid.
Do you have to sign a private contract with Medicare?
You don't have to sign a private contract. You can always go to another provider who gives services through Medicare. If you sign a private contract with your doctor or other provider, these rules apply:
Can you opt out of Medicare?
Certain doctors and other health care providers who don’t want to work with the Medicare program may “opt out” of Medicare. Medicare doesn’t pay for any covered items or services you get from an opt-out doctor or other provider, except in the case of an emergency or urgent need.
Do doctors accept assignment?
Most doctors, providers, and suppliers accept assignment, but you should always check to make sure. Participating providers have signed an agreement to accept assignment for all Medicare-covered services. Here's what happens if your doctor, provider, or supplier accepts assignment: Your. out-of-pocket costs.
