When you have both Medicare and employer coverage, the size of your employer will determine how your Medicare benefits will coordinate with your employer coverage. If you become eligible for Medicare at age 65 while working for an employer with 20 or more employees, your group plan will be primary, and Medicare will be secondary.
Full Answer
When can I Change my Medicare plan?
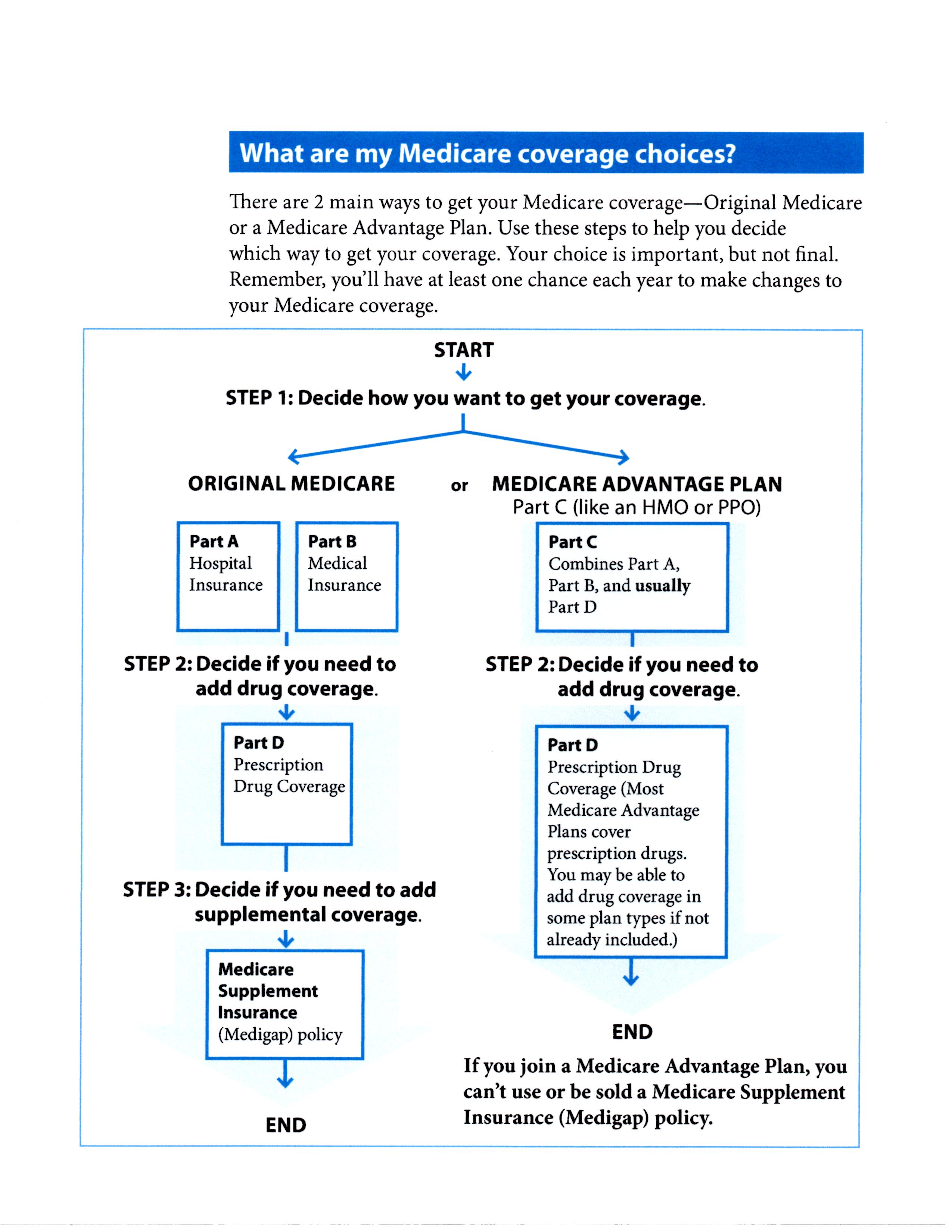
There are many plan changes that Medicare beneficiaries might want to make from one year to the next. For most of them, the applicable open enrollment period is October 15 to December 7, with changes effective on January 1. During that timeframe, you can: Switch from Original Medicare to Medicare Advantage, or vice versa.
What changes will Medicare enrollees see in 2021?
A: There are several changes for Medicare enrollees in 2021. Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7. (Here’s our overview of everything you need to know about the annual enrollment period.)
How do I change the address on my Medicare card?
How do I change my address with Medicare? To change your official address with Medicare, you have to contact Social Security. Follow these steps to update your information in your my Social Security account. Call 1-800-772-1213. TTY users can call 1-800-325-0778.
Can I re-enroll in Medicare after I've dropped my employer-sponsored health plan?
There are rules for re-enrolling in Medicare after you’ve dropped it for an employer-sponsored health plan. You’ll have an 8-month Special Enrollment Period in which to re-enroll in Medicare Part A and Part B.
Do you get your Medicare taken away if you start working?
Medicare and Medicaid Employment Supports - Ticket to Work - Social Security. Many people believe that they will automatically lose their Medicare or Medicaid as soon as they start working. But that's a myth.
Can you have Medicare and employer insurance at the same time?
Can I have Medicare and employer coverage at the same time? Yes, you can have both Medicare and employer-provided health insurance. In most cases, you will become eligible for Medicare coverage when you turn 65, even if you are still working and enrolled in your employer's health plan.
Is it a good idea to get Medicare if you're still working at 65?
If you have health insurance through a company with fewer than 20 employees, you should sign up for Medicare at 65 regardless of whether you stay on the employer plan. If you do choose to remain on it, Medicare is your primary insurance.
Will going back to work affect my Medicare?
If you're going back to work and can get employer health coverage that is considered acceptable as primary coverage, you are allowed to drop Medicare and re-enroll again without penalties. If you drop Medicare and don't have creditable employer coverage, you'll face penalties when getting Medicare back.
How does working affect Medicare?
It depends on how you get your health insurance now and the number of employees that are in the company where you (or your spouse) work. Generally, if you have job-based health insurance through your (or your spouse's) current job, you don't have to sign up for Medicare while you (or your spouse) are still working.
Is Medicare primary or secondary to employer coverage?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
Do I automatically get Medicare when I turn 65?
You automatically get Medicare when you turn 65 Part A covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What do I need to do before I turn 65?
Turning 65 Soon? Here's a Quick Retirement ChecklistPrepare for Medicare. ... Consider Additional Health Insurance. ... Review Your Social Security Benefits Plan. ... Plan Ahead for Long-Term Care Costs. ... Review Your Retirement Accounts and Investments. ... Update Your Estate Planning Documents.
What happens if you don't enroll in Medicare Part A at 65?
The Part A penalty is 10% added to your monthly premium. You generally pay this extra amount for twice the number of years that you were eligible for Part A but not enrolled. For example, suppose that: You were eligible for Medicare in 2020, but you didn't sign up until 2022.
Can I lose Medicare?
Summary: In most cases, you won't lose your Medicare eligibility. But if you move out of the country, or if you qualify for Medicare by disability or health problem, you could lose your Medicare eligibility.
Can Medicare Part B be suspended?
You can disenroll from Part B and stop paying premiums for it in this situation, regardless of whether it was you or your spouse who landed this new job. In other words, you're allowed to delay Part B without penalty if you have health insurance from current employment and the employer plan is primary to Medicare.
Can Medicare Part B be Cancelled?
You can voluntarily terminate your Medicare Part B (medical insurance). It is a serious decision. You must submit Form CMS-1763 (PDF, Download Adobe Reader) to the Social Security Administration (SSA). Visit or call the SSA (1-800-772-1213) to get this form.
What is the Medicare small employer exception?
If an employer, having fewer than 20 full and/or part-time employees, sponsors or contributes to a single-employer Group Health Plan (GHP), the Medicare Secondary Payer (MSP) rules applicable to individuals entitled to Medicare on the basis of age do not apply to such individuals.
What are Medicare Secondary Payer rules?
Generally the Medicare Secondary Payer rules prohibit employers with 20 or more employees from in any way incentivizing an active employee age 65 or older to elect Medicare instead of the group health plan, which includes offering a financial incentive.
Does Medicare Secondary cover primary deductible?
“Medicare pays secondary to other insurance (including paying in the deductible) in situations where the other insurance is primary to Medicare.
Is Medicare Part A free?
Most people don't pay a monthly premium for Part A (sometimes called "premium-free Part A"). If you buy Part A, you'll pay up to $499 each month in 2022. If you paid Medicare taxes for less than 30 quarters, the standard Part A premium is $499.
When to switch to original Medicare?
Switch to Original Medicare during the first year on the Medicare Advantage plan (trial period). Switch to Original Medicare during the annual Medicare Advantage open enrollment period (January 1 to March 31).
How to leave Medicare Advantage?
To protect Medicare beneficiaries, lawmakers provided escape hatches for Medicare Advantage enrollees who decide – for whatever reason – that they’d rather be covered under Original Medicare . There are essentially four different avenues available to enrollees who want to leave their Medicare Advantage plan: 1 Make changes during general open enrollment (October 15 to December 7, with changes effective January 1). 2 Switch to Original Medicare during the first year on the Medicare Advantage plan (trial period). 3 Switch to Original Medicare during the annual Medicare Advantage open enrollment period (January 1 to March 31). Note that Medicare Advantage enrollees also have the option to switch to a different Medicare Advantage plan during this time. 4 Switch to Original Medicare (or a different Medicare Advantage plan, depending on the situation) if a special enrollment period becomes available.
How long is the disenrollment period for Medicare?
The disenrollment period, created by the Affordable Care Act, was only a month and a half long. It allowed Medicare Advantage enrollees to switch to Original Medicare and a Part D plan, but did not allow them to switch to a different Medicare Advantage plan.
What percentage of Medicare beneficiaries are in Medicare Advantage?
Medicare Advantage (Medicare Part C) has become increasingly popular over the last decade. Thirty-four percent of all Medicare beneficiaries were in Medicare Advantage plans as of 2019, up from just 13 percent in 2005. And by late 2019, nearly 38 percent of Medicare beneficiaries had private coverage, nearly all of whom had Medicare Advantage ( Medicare Cost plans are another form of private Medicare coverage, but very few people are enrolled in those plans). But that doesn’t mean everyone is happy with Medicare Advantage, or that it’s the right option for all Medicare beneficiaries who enroll in it.
How long is the Medicare trial period?
This applies to people who enrolled in Medicare Advantage as soon as they turned 65 , and also to people who switched from Original Medicare to Medicare Advantage – but only if it’s their first time being on a Medicare Advantage plan.
How many stars does Medicare have?
Medicare utilizes a star rating system for Medicare Advantage and Part D Prescription Drug Plans. Each Medicare contract is assigned a rating of one to five stars, with the best contracts receiving five stars.
When is the open enrollment window for Medicare Part B?
This window runs from January 1 to March 31, with coverage effective July 1.
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.
When will Medicare stop allowing C and F?
As a result of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), Medigap plans C and F (including the high-deductible Plan F) are no longer available for purchase by people who become newly-eligible for Medicare on or after January 1, 2020.
When will Medicare Part D change to Advantage?
Some of them apply to Medicare Advantage and Medicare Part D, which are the plans that beneficiaries can change during the annual fall enrollment period that runs from October 15 to December 7.
What is the maximum out of pocket limit for Medicare Advantage?
The maximum out-of-pocket limit for Medicare Advantage plans is increasing to $7,550 for 2021. Part D donut hole no longer exists, but a standard plan’s maximum deductible is increasing to $445 in 2021, and the threshold for entering the catastrophic coverage phase (where out-of-pocket spending decreases significantly) is increasing to $6,550.
What is the Medicare premium for 2021?
The standard premium for Medicare Part B is $148.50/month in 2021. This is an increase of less than $4/month over the standard 2020 premium of $144.60/month. It had been projected to increase more significantly, but in October 2020, the federal government enacted a short-term spending bill that included a provision to limit ...
How much is the Medicare coinsurance for 2021?
For 2021, it’s $371 per day for the 61st through 90th day of inpatient care (up from $352 per day in 2020). The coinsurance for lifetime reserve days is $742 per day in 2021, up from $704 per day in 2020.
How many people will have Medicare Advantage in 2020?
People who enroll in Medicare Advantage pay their Part B premium and whatever the premium is for their Medicare Advantage plan, and the private insurer wraps all of the coverage into one plan.) About 24 million people had Medicare Advantage plans in 2020, and CMS projects that it will grow to 26 million in 2021.
What is the income bracket for Medicare Part B and D?
The income brackets for high-income premium adjustments for Medicare Part B and D will start at $88,000 for a single person, and the high-income surcharges for Part D and Part B will increase in 2021. Medicare Advantage enrollment is expected to continue to increase to a projected 26 million. Medicare Advantage plans are available ...
What to do if you move to a new state with Medicare?
If you are moving, no matter what type of Medicare coverage you have, you must inform the Social Security Administration of your new address. If you cannot keep your current healthcare providers, perhaps they can recommend people in your new state.
How to change my Social Security mailing address?
When you move, you should also contact the Social Security Administration to change your on-file mailing address. You can do this online at the official S.S.A. site which is www.ssa.gov, or you can phone them at 1-800-772-1213 Monday through Friday from 7:00 a.m. to 7:00 p.m.
How to enroll in Medicare Supplement Plan?
1. Enroll in a Medicare Supplement Plan through your current Medigap provider if it covers the same, or fewer benefits than your current SELECT plan. 2. Enroll in a Medigap plan offered by any provider in your new area of service. Also, if you have a Medicare Advantage plan in your current state but there are no available Part C plans in the state ...
How long does a SEP last?
If you notify your provider before you move, your SEP begins the month before you move and continues for two months after the move. If you wait until after you move to notify your provider, your SEP begins the month of notification and ends after two months have passed. If you have a Medicare Advantage plan before you move ...
What is a SEP in Medicare?
You can take advantage of a Special Enrollment Period (SEP) to make changes to a Part C or D plan. SEPs are available for Medicare recipients who experience certain life events. If you are moving outside your plan’s area of service and need a new plan, or if you are moving within the plan’s area of service and wish to include new plan options ...
Does Medicare require you to use a hospital?
Medicare does not require you to use healthcare providers or hospitals in networks, as is the case with some Medicare Advantage plans. Once you have moved, you can choose any physician, hospital, or other healthcare provider as long as they accept Medicare assignment. Using healthcare providers who accept Medicare assignment ensures ...
Do you need to change your Medicare plan when you move?
Generally speaking, if your plan requires that you use a set network for healthcare service providers, you will need to make more changes when you move . Because having continuous healthcare coverage is so important, you should have all the facts about how your Medicare benefits are affected by your move before you start packing.
What is a moon in Medicare?
Most observation patients get a Medicare form called a Medicare Outpatient Observation Notice (MOON). But that isn’t enough.
How much does an observation patient have to pay for her stay?
But an observation patient is treated under Part B rules. Thus, an observation patient may have to pay as much as 20 percent of the costs of her stay (if she has it, Medicare Supplemental (Medigap) insurance may pick this up). But the real time bomb goes off after discharge.
Does Medicare cut payments to hospitals?
In recent years, Medicare has been cutting payments to hospitals that readmit certain patients within 30 days. But if a patient is under observation, the penalties don’t apply. The Medicare Payment Advisory Commission (MedPAC), which advises Congress on Medicare issues, says this is not an issue.
