To that end, here are eight simple rules for creating a Medicare POC—so you can provide treatment to patients who need you and get paid: 1. Provide all the details. As we explain in this guide, plans of care must—at minimum—include: “Medical diagnosis “Long-term functional goals “Type of services or interventions
Full Answer
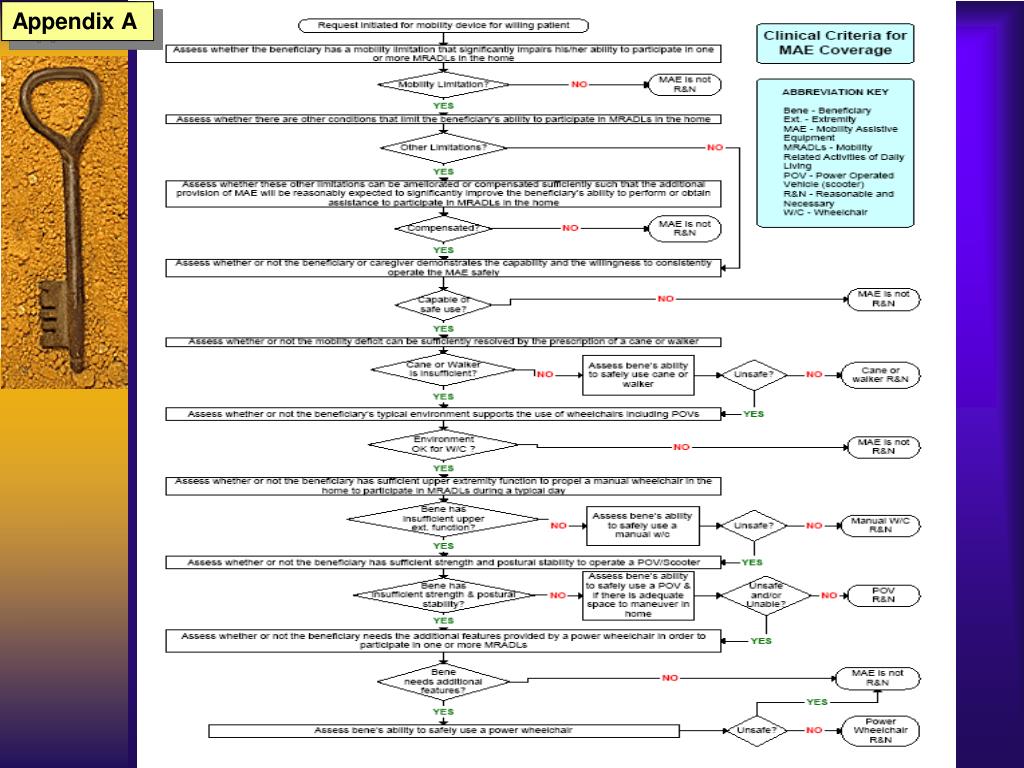
What is the Medicare Coverage Determination process?
Medicare Coverage Determination Process. Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or injury (and within the scope of a Medicare benefit category).
When are therapy services covered by Medicare?
The Centers for Medicare and Medicaid Services (CMS) states that therapy services shall be payable when the medical record and the information on the claim form consistently and accurately report covered therapy services.
What are the rules for creating a Medicare POC?
To that end, here are eight simple rules for creating a Medicare POC—so you can provide treatment to patients who need you and get paid: 1. Provide all the details. As we explain here, plans of care must—at minimum—include:
Why does Medicare want to coordinate care with my doctor?
Medicare wants to be sure that all doctors have the resources and information they need to coordinate your care. Coordinated care helps prevent: Getting the same service more than once (when getting the services again isn't needed)

What do Medicare regulations do?
Medicare Regulations means that certain government-sponsored insurance program under Title XVIII, P.L. 89-97, of the Social Security Act, which, among other things, provides for a health insurance system for eligible elderly and disabled individuals, as set forth at Section 1395, et seq.
How does Medicare determine medical necessity?
Insurance companies provide coverage for care, items and services that they deem to be “medically necessary.” Medicare defines medical necessity as “health-care services or supplies needed to diagnose or treat an illness or injury, condition, disease, or its symptoms and that meet accepted standards of medicine.”
How does the CMS regulate healthcare?
The CMS oversees programs including Medicare, Medicaid, the Children's Health Insurance Program (CHIP), and the state and federal health insurance marketplaces. CMS collects and analyzes data, produces research reports, and works to eliminate instances of fraud and abuse within the healthcare system.
What are the four components of Medicare medical necessity?
What are the 4 parts of Medicare?Medicare Part A – hospital coverage.Medicare Part B – medical coverage.Medicare Part C – Medicare Advantage.Medicare Part D – prescription drug coverage.
Who decides medically necessary?
How is “medical necessity” determined? A doctor's attestation that a service is medically necessary is an important consideration. Your doctor or other provider may be asked to provide a “Letter of Medical Necessity” to your health plan as part of a “certification” or “utilization review” process.
What are the guidelines for medical necessity?
"Medically Necessary" or "Medical Necessity" means health care services that a physician, exercising prudent clinical judgment, would provide to a patient. The service must be: For the purpose of evaluating, diagnosing, or treating an illness, injury, disease, or its symptoms.
What does CMS guidelines stand for?
Centers for Medicare & Medicaid ServicesThe Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
Who enforces CMS regulations?
CMS is charged on behalf of HHS with enforcing compliance with adopted Administrative Simplification requirements. Enforcement activities include: Educating health care providers, health plans, clearinghouses, and other affected groups, such as software vendors. Solving complaints.
Why is CMS important to healthcare organizations?
With expenditures of approximately $650 billion in 2006 and with more than 90 million beneficiaries, CMS plays a key role in the overall direction of the healthcare system. It is CMS's mission to ensure effective, up-to-date healthcare coverage and to promote quality care for its beneficiaries.
Which CMS publications provide medical necessity guidelines?
ResourcesCMS Internet Only Manual (IOM), Publication 100-08, Medicare Program Integrity Manual, Chapter 13, Local Coverage Determinations.American Medical Association (AMA) Current Procedural Terminology (CPT) Manual.Healthcare Common Procedure Coding System (HCPCS) Manual.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
What is not medically necessary?
“Not medically necessary” means that they don't want to pay for it. People, please. Acme Insurance didn't do a ton of research to find out if you. needed this treatment or not.
What is Medicare coverage?
Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or injury (and within the scope of a Medicare benefit category).
When did the NCD change?
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 amended several portions of the NCD development process with an effective date of January 1, 2004.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
Why are guidelines important?
Guidelines help doctors understand the best ways to diagnose, treat and even prevent diseases and conditions. Guideline recommendations are based on the strongest available scientific evidence. The creation of a guideline is a rigorous process because careful scientific study is at the heart of every guideline.
What is the challenge of creating guidelines?
One challenge of creating guidelines is that treatments are based on averages: what will help the most patients with the fewest side effects. Thus, health care providers need risk assessment tools and clinical judgment as to how a recommendation applies to each patient.
What is the AHA guidelines?
Since then, the organization has created guidelines covering a wide variety of topics related to heart disease and stroke. The AHA has created numerous guidelines with the American College of Cardiology. The two first worked together on 1984 guidelines about pacemakers – at the request of the federal government.
What is the Medicare requirement for therapy?
In general, Medicare requires that therapy services are of appropriate type, frequency, intensity, and duration for the individual needs of the patient. Documentation should: Establish the variables that influence the patient's condition, especially those factors that influence the clinician's decision to provide more services than are typical ...
What is the purpose of treatment notes?
Treatment Notes. The purpose of the treatment note is not to document medical necessity, but to create a record of all encounters and skilled intervention. Documentation is required for every treatment day, every therapy service, and must include the following information:
What is an evaluation in a plan of care?
Evaluation. The initial evaluation, or the plan of care including an evaluation, should document the necessity for a course of therapy through objective findings. Documentation of the evaluation should list the conditions and complexities and, where it is not obvious, describe the impact of the conditions and complexities on ...
When is therapy service payable?
The Centers for Medicare and Medicaid Services (CMS) states that therapy services shall be payable when the medical record and the information on the claim form consistently and accurately report covered therapy services. Documentation should also include objective measures of the patient's improvement as a means to justify therapy services ...
How often do you need to complete a progress report?
A clinician must complete a progress report at least once every 10 treatment days or at least once during each certification interval, whichever is less. The beginning of the first reporting period is the first day of the episode of treatment regardless of whether the service provided on that day is an evaluation, re-evaluation, or treatment.
What is the difference between the amount and frequency of therapy?
Type, amount, duration, and frequency of therapy services. The amount of treatment refers to the number of times in a day the type of treatment will be provided. The frequency refers to the number of times in a week the type of treatment is provided. The duration is the number of weeks, or the number of treatment sessions.
What is the long term treatment goal?
Long term treatment goals should be developed for the entire episode of care and not only for the services provided under a plan for one interval of care . The plan of care shall contain, at minimum, the following information: Type, amount, duration, and frequency of therapy services.
What is the necessity of physical therapy?
The necessity for treatment is established by the physical therapist at the first evaluation. The patient’s treatment diagnosis and health challenges associated with it, such as weakness, pain or balance deficits, must be deemed appropriate for physical therapy care. There must also be achievable goals that the patient can meet within ...
Does Medicare cover physical therapy?
Medicare provides medical coverage under multiple parts, but for physical therapy these services are covered under Medicare Part A and Medicare Part B. Medicare Part A coverage applies to physical therapy provided as an inpatient, such as in the hospital or a rehabilitation facility, but also when the patient is homebound.
What should an MA organization do before contracting with CMS?
Before an MA organization contracts with an entity to perform functions that are otherwise the responsibility of the MA organization under its contract with CMS, the MA organization should develop, implement, and maintain policies and procedures for assessing contracting provider groups' administrative and fiscal capacity to manage financial risk prior to delegating MA-related risk to these groups. Suggested policies and procedures include:
How long do you have to give CMS notice?
The organization must give CMS notice at least 90 days before the intended date of termination which specifies the reasons the MA organization is requesting contract termination.
What is the MA administrative contracting requirement?
The MA administrative contracting requirements apply both to first tier contracts and to downstream contracts in the manner specified for provider contracts, as described above. At the same time, the responsibility of the MA organization is to assure that its contractor and any downstream contractors have the information necessary to know how to comply with the requirements under the MA program.
Who audits MA contracts?
DHHS, the Comptroller General, or their designees may audit, evaluate, or inspect any books, contracts, medical records, patient care documentation, and other records of the MA organization or relating to the MA organization's MA contract. DHHS, the Comptroller General, or their designees may audit, evaluate, or inspect any books, contracts, medical records, patient care documentation, and other records of the related entity, contractor, subcontractor, or its transferee that pertain to any aspect of services performed, reconciliation of benefit liabilities, and determination of amounts payable under the contract, or as the Secretary may deem necessary to enforce the MA contract.
Does CMS enter into a contract with an entity?
Unless an organization has a minimum enrollment waiver as explained below, CMS does not enter into a contract with an entity unless it meets the following minimum enrollment requirements:
How long does it take to get a certified plan of care?
You should only proceed with treatment, though, if you’re confident that you’ll be able to obtain a certified plan of care within that 30-day timeframe. Otherwise, you risk not receiving payment for your services. On that note, be sure to get a real or electronic signature—not a stamp. 5.
Is "Medicare" and "Simple" the same sentence?
Senior Writer. “Simple” and “Medicare” are rarely used in the same sentence, but that doesn’t have to be the case—especially when it comes to developing physical therapy, occupational therapy, and speech-language pathology plans of care (POCs) and adhering to certification requirements. While these treatment outlines might seem daunting at first, ...
Do you have to be a primary care physician to sign a POC?
The certifying physician does not have to be the patient’s primary care physician—and Medicare has no requirement that the patient see the certifying physician before that physician signs the POC (although the MD may have his or her own requirement to that end). That’s just one more reason to build a robust network of responsive physicians who understand the value of your services. That way, you can ensure there’s no delay on obtaining a signed POC—and thus, no delay on providing critical care to your patients.
Does Medicare allow PTs?
While Medicare does allow PT, OT, and SLP assistants to provide services to Medicare beneficiaries under certain conditions, it requires that all plans of care be established by fully licensed providers. That means only PTs, OTs, and SLPs should develop patient treatment plans.
Do you need to establish a new Medicare plan of care?
Individuals who become newly eligible for Medicare during their course of care are considered new patients under Medicare, so you’ll need to establish a new certified plan of care and count the first visit post-eligibility change as visit number one.
Do you have to recertify a POC before it expires?
As noted here, in order to continue providing care beyond the initial certification period, the therapist must have the physician recertify the plan of care before it expires. If you’re unable to obtain a recertification signature before the plan lapses, be sure to update the POC immediately and include an explanation for the delay in your documentation. (If you’re a WebPT Member, you can also use the Plan of Care report to see which POCs are pending certification and which require recertification.)
.png/315px-United_States_Export_Treemap_(2011).png)
Summary
- In general, Medicare requires that therapy services are of appropriate type, frequency, intensity, and duration for the individual needs of the patient. Documentation should: 1. Establish the variables that influence the patient's condition, especially those factors that influence the clinician's decision to provide more services than are typical f...
Evaluation
- The initial evaluation, or the plan of care including an evaluation, should document the necessity for a course of therapy through objective findings. Documentation of the evaluation should list the conditions and complexities and, where it is not obvious, describe the impact of the conditions and complexities on the prognosis and/or the plan for treatment so that it is clear to a reviewer t…
Plan of Care/Certification of The Plan of Care
- The plan of care shall be consistent with the related evaluation. The evaluation and plan may be reported in two separate documents or a single combined document. The certified plan of care ensures that the patient is under the care of a physician or NPP. Long term treatment goals should be developed for the entire episode of care and not only for the services provided under …
Progress Reports
- The progress report provides justification for the medical necessity of treatment. A clinician must complete a progress report at least once every 10 treatment days or at least once during each certification interval, whichever is less. The beginning of the first reporting period is the first day of the episode of treatment regardless of whether the service provided on that day is an evaluati…
Treatment Notes
- The purpose of the treatment note is not to document medical necessity, but to create a record of all encounters and skilled intervention. Documentation is required for every treatment day, every therapy service, and must include the following information: 1. the encounter note must record the name of the treatment, intervention of activity provided; 2. total treatment time; and 3. signature …
Discharge Note
- The Discharge Note is required and shall be a progress report written by a clinician and shall cover the reporting period from the last progress report to the date of discharge. The discharge note shall include all treatment provided since the last progress report and indicate that the therapist reviewed the notes and agrees to the discharge.