Getting credentialed (or on insurance panels) involves retrieving and filling out a series of applications with insurance companies (which takes upward of 10 hours per panel), submitting the applications to insurance companies, ensuring each has received your application, and then doing a lot of follow up to track the progress of each application.
Full Answer
How to credential for Medicare?
± Eligibility for Participation in Medicare (Excluded and Opt -Out) - Quality of Care Issues, Grievances etc.(usually at recredentialing) In addition, credentialing must include a Completed Application and the use of Current Documents ( The information used in the review must be no more than 6 months old on the date of determination.)
How much does medical credentialing cost?
Nov 23, 2021 · What Is Medicare Credentialing. Medicare providers serve Medicare beneficiaries and are paid for their services by Medicare instead of by the individuals. Medicare approves a variety of individual practitioners, agencies and facilities to provide high-quality care to Medicare recipients. Medicare credentialing standards vary depending on the type of services you are …
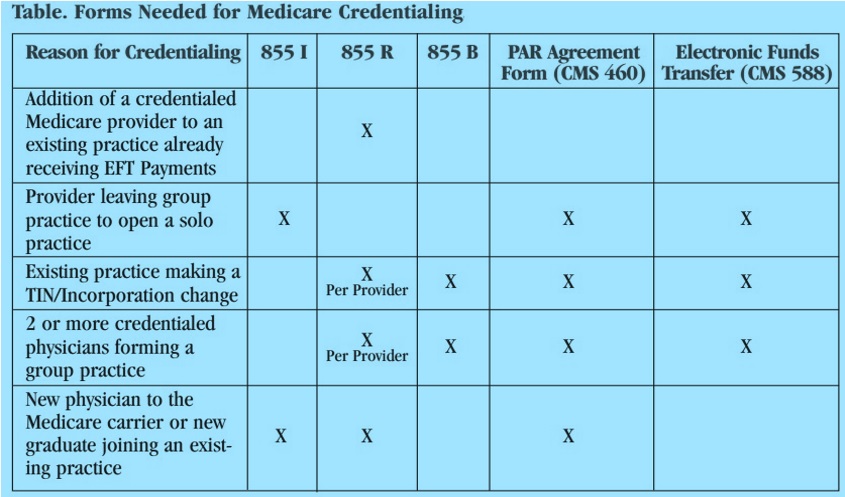
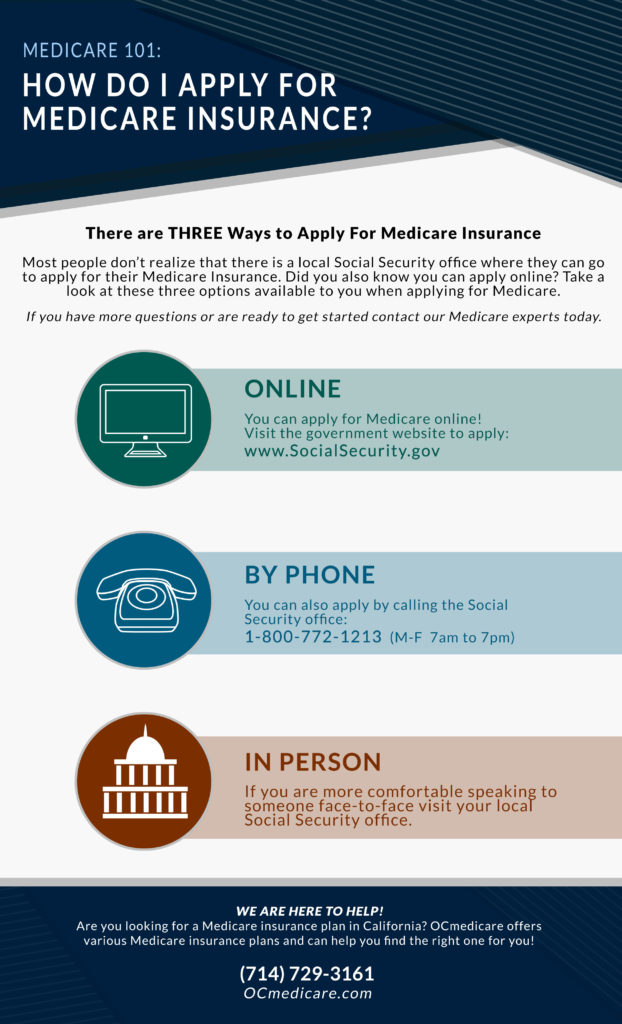
What documents do I need to apply for Medicare?
Use this guide if any of the following apply: You’re a health care provider who wants to bill Medicare for your services and also have the ability to order and certify.; You don’t want to bill Medicare for your services, but you do want enroll in Medicare solely to order and certify.; You wish to provide services to beneficiaries but do not want to bill Medicare for your services.
How to get credentialed with Medicaid?
Nov 10, 2020 · Medical credentialing is a professional process that helps to establish and maintain effective standards throughout the medical community. Its central goal is to promote patient confidence and ensure the highest quality of care.
What does it mean to be credentialed with Medicare?
Credentialing is the process of approving a physician, agency or other medical provider as part of the Medicare supply chain.Apr 1, 2020
Does Medicare backdate credentialing?
Answer: The short answer is Yes, but there are some specifics that you need to be aware of. Retroactively billing Medicare is critical for most organizations as providers often start without having a Medicare number.
How long does it take to get CMS approval?
CMS is presently averaging between four and six months to provide a response. Failure to provide CMS with all the necessary information and documentation at the time of submission can result in a “development request” from CMS which can delay the approval process further.
What does it mean to be credentialed by insurance companies?
Credentialing is a process that the insurance companies use to verify your education, training, and professional experience and to ensure that you meet their internal requirements for serving as an in-network provider on their panel.
Will Medicare retro pay?
A Medicare program to help people with limited income and resources pay Medicare prescription drug program costs, like premiums, deductibles, and coinsurance. with an effective date in the past (retroactive). You'll be automatically enrolled in a Medicare drug plan unless you decline coverage or join a plan yourself.
How long does it take to get Medicare Part B after?
Most Medicare provider number applications are taking up to 12 calendar days to process from the date we get your application. Some applications may take longer if they need to be assessed by the Department of Health. We assess your application to see if you're eligible to access Medicare benefits.Dec 10, 2021
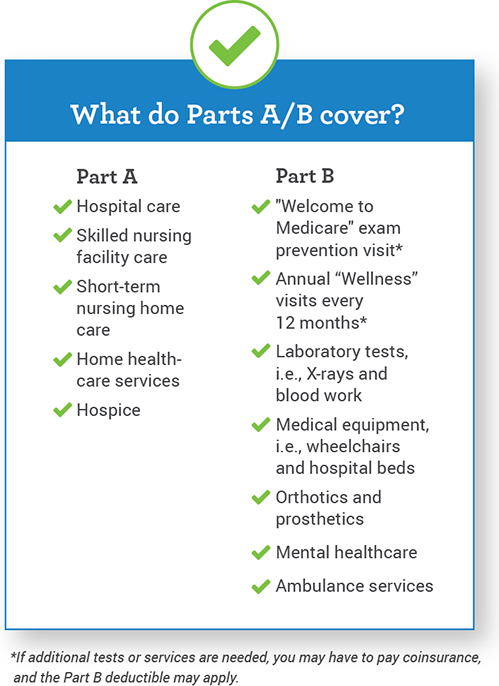
What triggers payment of Medicare Part A benefits?
If you're under 65, you get premium-free Part A if: You have Social Security or Railroad Retirement Board disability benefits for 24 months. You have End-Stage Renal Disease (ESRD) or Amyotrophic Lateral Sclerosis (ALS) and meet certain requirements.
Does Medicare cover experimental drugs?
Routine costs associated with Medicare approved Clinical Trials is Medicare's financial responsibility. Experimental and investigational procedures, items and medications are not covered.Aug 17, 2021
What is a Category B device?
Category B (Non-experimental/investigational) device refers to a device for which the incremental risk is the primary risk in question (that is, initial questions of safety and effectiveness of that device type have been resolved), or it is known that the device type can be safe and effective because, for example, ...Jan 5, 2015
What are the steps that the process of credentialing usually consist of?
6 Key Steps In Provider CredentialingThe Importance of Credentialing.#1 Identify the Required Documents.#2 Prioritize Insurers.#3 Check for Accurate Information.#4 Completing the CAQH.#5 Wait for Verification.#6 Following Up.#7 Recertification.More items...
What is credentialing process?
Credentialing is the process of checking that healthcare providers have the required licenses, certificates, and other titles in good standing to do their job. A hospital will first check a provider's credentials to make sure they can work in the facility.Feb 15, 2019
What does getting credentialed mean?
Credentialing is the process of establishing the qualifications of licensed medical professionals and assessing their background and legitimacy.
What is the purpose of medical credentialing?
This regulation is designed to ensure that all patients receive only the highest quality of care from practitioners who are truly qualified to provide it.
How long does it take to get a medical credential?
In some cases, where a minimal amount of background information needs to be gathered, the process might only take 7 to 10 days. Though in the case of a specialist, or an application that was filled out incorrectly, the medical credentialing process might take several weeks to several months.
What are the different types of healthcare organizations?
Also known as NCQA it is an independent, nonprofit organization that specifically evaluates and directly reports on the quality of healthcare organizations before issuing them credentials. This includes: 1 Preferred Provider Organization 2 Managed Behavioral Healthcare Organizations 3 New Health Plans 4 Doctor Organizations 5 Managed Care Plans 6 Credentials Verification Organizations 7 Disease Management Programs
What is TJC accreditation?
More commonly known as TJC they are an accrediting organization that serves to maintain the highest standards and best practices of the United States healthcare industry. Hospitals and clinics will voluntarily submit themselves for TJC accrediting surveys at three-year intervals.
What is CMS in healthcare?
The CMS is an agency of the Federal Government under the United States Department of Health and Human Services umbrella. It has a wide range of responsibilities, including oversight of quality standards in long-term care facilities as well as clinical laboratories.
What is primary source verification?
Primary source verification plays an essential role in preventing any type of fraud in the medical credentialing process. They work directly with the Board of Medicine to confirm all medical licenses and adhere to strict standards for certified healthcare facilities.
Can a medical practitioner bill insurance?
Once a medical practitioner has been credentialed and their information has been provided to the institution for approved hiring, they can enter into a contract with an insurance company. This allows them to bill and is reimbursed as an in-network provider . This is especially important for small practices that sometimes need to handle their own medical billing or those who outsource to a third-party medical billing service.
What is credentialing software?
However, credentialing software tools can help reduce errors, eliminate redundancy, and speed up the credentialing process. They can also help organizations ensure providers remain compliant, ...
What is the most important step in the credentialing process?
A crucial step in the credentialing process that can’t be overlooked is a background check — even if the applicant’s CV looks impeccable. The three most frequently used data banks for background check s on healthcare providers are:
Why are automated alerts important?
For example, automated alerts can notify the medical staff coordinator or HR director that a license needs to be renewed by a certain date.
Do providers need to go through privileging?
In addition to credentialing, a provider may also need to go through privileging and payer enrollment. The differences between these processes can be confusing, and sometimes it’s assumed that once one of the three steps has been met, the physician is ready to practice at your facility. Credentialing and privileging are the two processes that most often get confused. At their most basic level, the three processes are:
What is credentialing in healthcare?
Credentialing in the healthcare industry sometimes goes by other terms, including the following: Insurance Credentialing: Also known informally as “getting on insurance panels,” this term refers to a health insurance company verifying a physician’s credentials.
What is provider credentialing?
Provider credentialing in healthcare is the process by which medical organizations verify the credentials of healthcare providers to ensure they have the required licenses, certifications, and skills to properly care for patients. The process is also called physician credentialing, medical credentialing, or doctor credentialing.
How long does it take to get a physician credentialed?
Under the most efficient circumstances, a physician can be credentialed to work at a hospital or credentialed and approved to be in-network for a health insurance company in 30 days. More often, the process takes 60 to 90 days. And on occasion — especially with insurance companies — it can take six months or more.
What is a medical sales rep?
Medical sales rep credentialing: Also known as vendor credentialing, this refers to healthcare organizations checking on and monitoring the background and training of sales reps and other vendors who may want or need access to the facilities. Credentialing is also used in non-medical contexts, including the following:
What is a CVO in healthcare?
In some cases, the healthcare facility or insurance company works with a third-party company — called a credentials verification organization (CVO) — that works with the provider to gather and verify information. Organizations often hire CVOs to allow for more efficient credentialing. 2. Check the Information.
What is a CAQH?
The Council for Affordable Quality Healthcare (CAQH) is a not-for-profit organization formed by some of the nation’s top health insurance companies . One of its online products — formerly called the Universal Provider Datasource and now known as ProView — gathers a common set of information from healthcare providers, including their professional background. Hundreds of insurance plans then use that common information as they credential providers — and relieve providers of the burden of submitting the same information to every insurance company they may want to enroll with.
Do hospitals have to be credentialed?
Healthcare organizations that don’t follow the CMS regulations are not eligible for Medicare or Medicaid reimbursement. Similarly, the Joint Commission accredits only those who follow its regulations. Most U.S. hospitals pursue the Joint Commission accreditation, which is required for Medicare and Medicaid reimbursement eligibility. States also have their own regulations.
Different Credentialing Processes for Psychologist vs Physician
Psychcare is similar to a TPA (third party administrator) or IPA (independent physician association) if you’re familiar with either of these. The psychiatrist would still need to negotiate his/her contract with a company like Psychcare but this agreement will include rates for a number of different plans.
Difference Between Commercial Insurance Contracting & Medicare Enrollment
The commercial insurer process involves credentialing (primary source verification, CAQH credentialing) and contracting which would include the contract negotiations; whereas with straight Medicaid or Medicare, they only need to be credentialed (Except where Participation vs Non Participation is concerned with Medicare).
What is medical credentialing?
For health care providers, medical credentialing is the process of getting networked with insurance companies (this is often described as “getting on insurance panels”). Medical credentialing is a popular term among health care providers these days, especially among counselors, chiropractors, and even massage therapists who, only a few years ago, ...
How to get credentialed in insurance?
1. Make a List. Research the insurance companies and find out which insurance companies you want to be credentialed with. Each company may require a different process with varying hoops you have to jump through. 2. Get Prepared, and Complete the CAQH. CAQH, the Council for Affordable Quality Healthcare, is often needed in conjunction ...
What is CAQH in insurance?
CAQH, the Council for Affordable Quality Healthcare, is often needed in conjunction with an insurance company’s application to complete one’s medical credentialing (i.e., to get on insurance panels). Major insurance companies, like BCBS and Aetna, use CAQH as a part of their application process.
How long is the CAQH application?
CAQH offers medical providers the option to complete the application online, or on paper. Don’t choose the paper option. First, the application is 50 pages long and only prints correctly in color.
What insurance companies use CAQH?
Major insurance companies, like BCBS and Aetna, use CAQH as a part of their application process. There are a few important things you need to know about your CAQH application…. You need to be invited. You can’t just go on to CAQH and upload your information; you need to be invited by an insurance company.
Is it easy to get a medical credential?
It’s no secret that the process of medical credentialing isn’t something many health care providers look forward to—in fact, it’s a process that many health care providers dread. While medical credentialing will probably never become your favorite pastime, there are a few things you can remember that will make the process easier: 1. Make a List. ...