What are the different types of Medicare benefits?
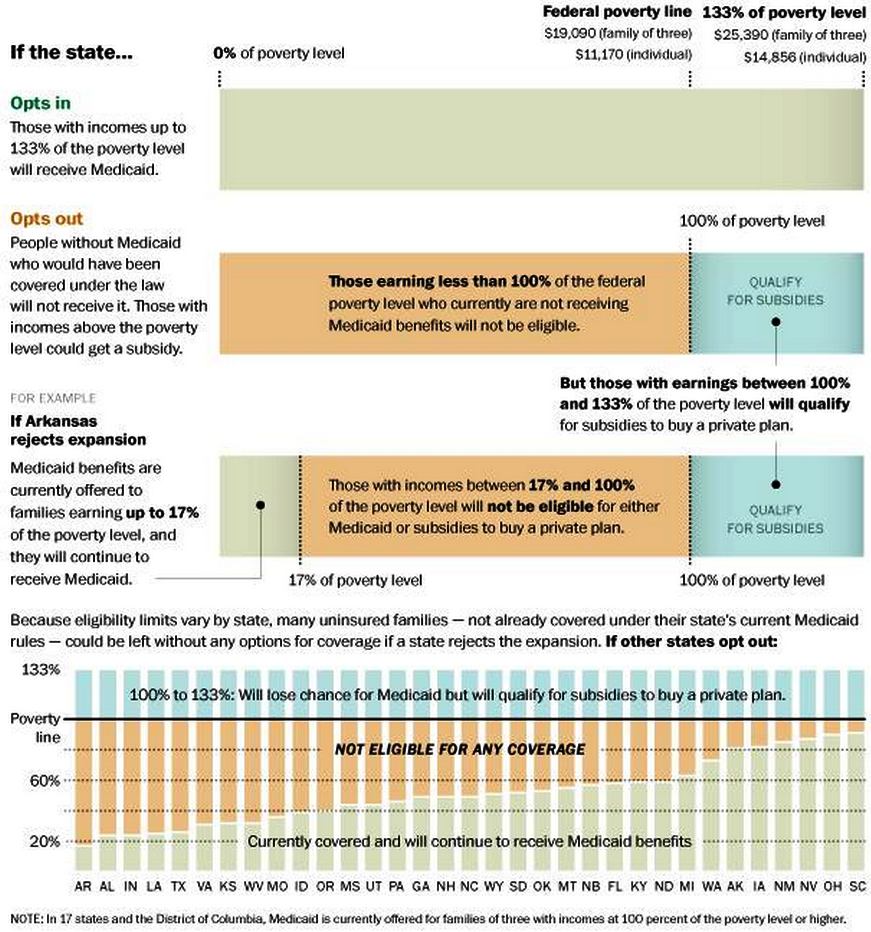
“Dual eligible beneficiaries” generally describes beneficiaries eligible for both Medicare and . Medicaid. The term includes beneficiaries enrolled in Medicare Part A, Part B, or both and . receiving full Medicaid benefits or assistance with Medicare premiums or cost sharing through one . of these Medicare Savings Program (MSP) eligibility ...
What is part a of Medicare?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. Medicare Part B (Medical Insurance) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Medicare Part D (prescription drug coverage)
What is coinsurance for Medicare?
Medicare Advantage (also known as Part C) Original Medicare includes Part A and Part B. You can join a separate Medicare drug plan to get Medicare drug coverage (Part D). You can use any doctor or hospital that takes Medicare, anywhere in the U.S. To help pay your out-of-pocket costs in Original Medicare (like your 20%.
What is a Medicare Advantage health plan (Mah)?
• How Medicare works with other types of coverage • Who should pay your bills first ... printed. Changes may occur after printing. Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. ... • For active-duty military enrolled in Medicare, TRICARE pays first for ...
How is the Medicare benchmarks calculated?
Benchmarks are calculated using the spending of all Traditional FFS Medicare beneficiaries. This includes those individuals that are enrolled only in Part A or only in Part B. Yet benefits in Medicare Advantage must cover benefits under both Part A and Part B.
What is Medicare 60 day rule?
A benefit period begins the day you are admitted to a hospital as an inpatient, or to a SNF, and ends the day you have been out of the hospital or SNF for 60 days in a row. After you meet your deductible, Original Medicare pays in full for days 1 to 60 that you are in a hospital.
How does Medicare measure the end of year benefit period?
A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins.
Do Medicare Advantage plans follow LCD?
Medicare Advantage plans are required to follow all Medicare laws and coverage policies, including LCDs (Local Coverage Decisions - coverage policies set by Medicare Fee-for-Service Contractors in your geographic area), when determining coverage for a particular service.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
Does Medicare have a lifetime limit?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What is a benefit period under Medicare Part A?
In Medicare Part A, which is hospital insurance, a benefit period begins the day you go into a hospital or skilled nursing facility and ends when you have been out for 60 days in a row. If you go back into the hospital after 60 days, then a new benefit period starts, and the deductible happens again.
What is the current Medicare Part B deductible?
Medicare Part B Premium and Deductible The standard monthly premium for Medicare Part B enrollees will be $170.10 for 2022, an increase of $21.60 from $148.50 in 2021. The annual deductible for all Medicare Part B beneficiaries is $233 in 2022, an increase of $30 from the annual deductible of $203 in 2021.Nov 12, 2021
Do Medicare benefits reset every year?
Does Medicare Run on a Calendar Year? Yes, Medicare's deductible resets every calendar year on January 1st. There's a possibility your Part A and/or Part B deductible will increase each year. The government determines if Medicare deductibles will either rise or stay the same annually.
How does CMS define a Medicare Advantage Plan?
Medicare Advantage is an “all in one” alternative to Original Medicare. These “bundled” plans include Part A, Part B, and usually Part D. Plans may have lower out-of- pocket costs than Original Medicare. In many cases, you'll need to use doctors who are in the plan's network.
Do Medicare replacements follow Medicare guidelines?
Medicare Advantage Plans Must Follow CMS Guidelines In the United States, according to federal law, Part C providers must provide their beneficiaries with all services and supplies that Original Medicare Parts A and B cover. They must also provide any additional benefits proclaimed in their Part C policy.
What is the difference between LCD and NCD for Medicare?
When a contractor or fiscal intermediary makes a ruling as to whether a service or item can be reimbursed, it is known as a local coverage determination (LCD). When CMS makes a decision in response to a direct request as to whether a service or item may be covered, it's known as a national coverage determination (NCD).Mar 26, 2016
What is Medicare for?
Medicare is the federal health insurance program for: 1 People who are 65 or older 2 Certain younger people with disabilities 3 People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
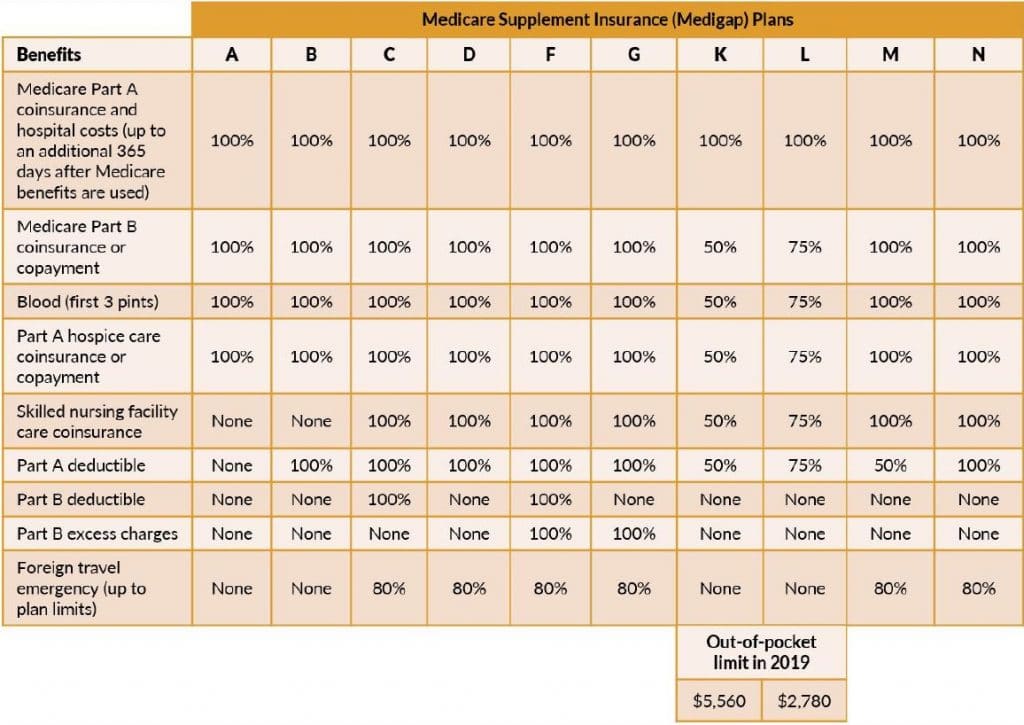
What is a medicaid supplement?
A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles. Some Medigap policies also cover services that Original Medicare doesn't cover, like medical care when you travel outside the U.S.
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What is the standard Part B premium for 2020?
The standard Part B premium amount in 2020 is $144.60. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
What is SRDP in healthcare?
The SRDP sets forth a process to enable providers of services and suppliers to self-disclose actual or potential violations of the physician self-referral statute. Additionally, Section 6409 (b) of the ACA, gives the Secretary of HHS the authority to reduce the amount due and owing for violations of Section 1877.
What is the definition of home health services?
Home health services. Outpatient prescription drugs. Inpatient and outpatient hospital services. When enacted in 1989, Section 1877 of the Social Security Act (the Act) applied only to physician referrals for clinical laboratory services.
What is the Stark Law?
1395nn), also known as the physician self-referral law and commonly referred to as the “Stark Law”: Prohibits a physician from making referrals for certain designated health services (DHS) payable by Medicare to an entity with which he or she (or an immediate family member) ...
What information does Medicare use?
A Medicare contractor may use any relevant information they deem necessary to make a prepayment or post-payment claim review determination. This includes any documentation submitted with the claim or through an additional documentation request. (See sources of Medicare requirements, listed below).
What is CMS's role in Medicare?
CMS' Center for Program Integrity (CPI) oversees Medicare medical review contractors. CPI conducts contractor oversight activities such as: 1 Providing broad direction on medical review policy 2 Reviewing and approving Medicare contractors' annual medical review strategies 3 Facilitating Medicare contractors' implementation of recently enacted Medicare legislation 4 Facilitating compliance with current regulations 5 Ensuring Medicare contractors' performance of CMS operating instructions 6 Conducting continuous monitoring and evaluation of Medicare Contractors' performance in accord with CMS program instructions as well as contractors' strategies and goals 7 Providing ongoing feedback and consultation to contractors regarding Medicare program and medical review issues
What is Medicare NCD?
National Coverage Determinations (NCDs): Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or injury (and within the scope of a Medicare benefit category).