The front of a Medigap policy must clearly identify it as “Medicare Supplement
Medigap
Medigap refers to various private health insurance plans sold to supplement Medicare in the United States. Medigap insurance provides coverage for many of the co-pays and some of the co-insurance related to Medicare-covered hospital, skilled nursing facility, home health care, ambulance, durable medical equipment, and doctor charges. Medigap's name is derived from the notion that it exists to …
Full Answer
How do I know if my plan is a Medicare supplement?
When you receive the printed copy of your plan, it must clearly state that it is Medicare Supplement insurance on the title page. In most cases, you pay your monthly Medigap premium directly to your private insurance provider. You do not pay this premium together with your Original Medicare Part B premium.
Should I buy a Medicare supplement policy?
If you are concerned about your out of pocket expenses that are not covered by Original Medicare, you may want to consider purchasing a Medicare Supplement policy to help cover some of your costs.
What is Medicare supplement insurance and how does it work?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
How are Medicare supplement insurance rates set?
There are three methods that a company can use to set rates for their Medicare Supplement policies: • Community-rated: With this pricing policy, every member, regardless of age, pays the same price. Hence, the name “Community.” • Issue-age-rated: Your age is used for pricing, and is locked in on your policy start date.

How long does an insured have to examine a Medicare Supplement policy?
Medigap free-look period You have 30 days to decide if you want to keep the new Medigap policy. This is called your "free look period." The 30-day free look period starts when you get your new Medigap policy.
How are Medicare Supplement plans regulated?
The California Department of Insurance (CDI) regulates Medicare Supplement policies underwritten by licensed insurance companies. The CDI assists consumers in resolving complaints and disputes concerning premium rates, claims handling, and many other problems with agents or companies.
Do Medicare Supplement plans automatically update when Medicare changes?
Once you find the best plan, you will likely want to be able to keep it. Fortunately, you will be able to stay with your plan as long as you like in most cases. This is called “guarantee renewable.” Medicare Supplement insurance plans renew automatically when you make your premium payment.
Can I be denied a Medicare Supplement plan?
For the most part, Medicare Supplement policies are guaranteed renewal. This means as long as you pay the monthly premium, you cannot be denied coverage once you enroll in a plan, regardless of any health conditions that may arise.
Who is the largest Medicare Supplement provider?
UnitedHealthCareAARP/United Health Group has the largest number of Medicare Supplement customers in the country, covering 43 million people in all 50 states and most U.S. territories. AARP licenses its name to insurer UnitedHealthCare, which helps make these policies so popular.
What states allow you to change Medicare Supplement plans without underwriting?
In some states, there are rules that allow you to change Medicare supplement plans without underwriting. This includes California, Washington, Oregon, Missouri and a couple others. Call us for details on when you can change your plan in that state to take advantage of the “no underwriting” rules.
Can I change my Medicare Supplement plan at any time?
As a Medicare beneficiary, you can change supplements at any time. As a result, there's no guarantee an application will be accepted if switched outside the designated Open Enrollment Period. An application may be “medically underwritten”.
Can you change Medicare Supplement plans every year?
You can either change to a standardized Medicare Supplement insurance plan with the same or fewer basic benefits than your current plan, or buy any Medicare Supplement Plan A, B, C*, F*, K, or L. You've had your current Medicare Supplement insurance plan for less than six months.
Can I switch from Medicare Advantage to Medicare Supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
Do pre-existing conditions apply to Medicare Supplement plans?
Summary: A Medicare Supplement insurance plan may not deny coverage because of a pre-existing condition. However, a Medicare Supplement plan may deny you coverage for being under 65. A health problem you had diagnosed or treated before enrolling in a Medicare Supplement plan is a pre-existing condition.
Do Medicare Supplement plans have a waiting period?
What is the Medicare Supplement Waiting Period? For up to six months after your Medicare Supplement plan begins, your new plan can choose not to cover its portion of payments for preexisting conditions that were treated or diagnosed within six months of the start of the policy.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
How are Medicare Supplement plans paid for?
You pay your Medicare Supplement Insurance (Medigap) premium as directed by the insurance company that sold you the plan. Medicare Supplement insurance plans are sold by private insurance companies and may help you pay for out-of-pocket costs for services covered under Original Medicare (Part A and Part B).
Which of the following is true about Medicare supplemental insurance plans?
Which of the following is true about Medicare Supplement Insurance Plans? They are regulated by the Centers for Medicare & Medicaid Services (CMS). Plan benefit amounts automatically update when Medicare changes cost sharing amounts, such as deductibles, coinsurance and copayments.
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because private insurance companies make it difficult for them to get paid for their services.
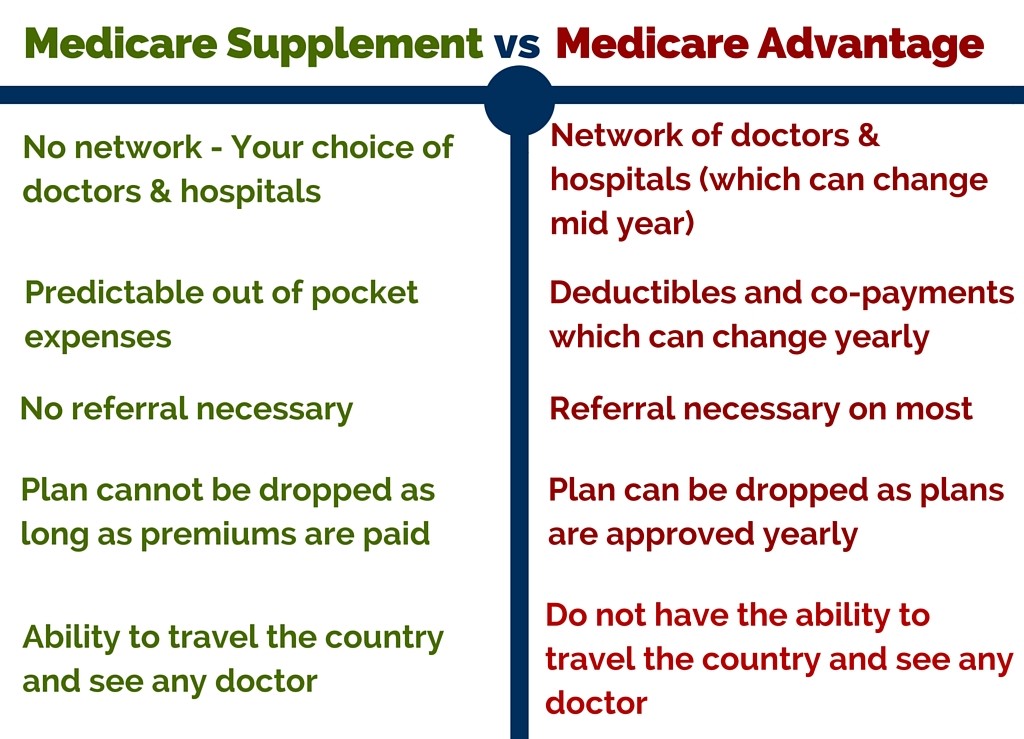
What is the difference between a Medicare Advantage plan and a Medicare Supplement plan?
Medicare Advantage and Medicare Supplement are different types of Medicare coverage. You cannot have both at the same time. Medicare Advantage bundles Part A and B often with Part D and other types of coverage. Medicare Supplement is additional coverage you can buy if you have Original Medicare Part A and B.
What happens if you buy a Medigap policy?
If you have Original Medicare and you buy a Medigap policy, here's what happens: Medicare will pay its share of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges.
What is a Medigap policy?
Those plans are ways to get Medicare benefits, while a Medigap policy only supplements your Original Medicare benefits. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage.
What is Medicare Advantage?
Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources.
How many people does a Medigap policy cover?
for your Medigap policy. You pay this monthly premium in addition to the monthly Part B premium that you pay to Medicare. A Medigap policy only covers one person. If you and your spouse both want Medigap coverage, you'll each have to buy separate policies.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). and is sold by private companies.
Does Medicare cover prescription drugs?
Some Medigap policies sold in the past cover prescription drugs. But, Medigap policies sold after January 1, 2006 aren't allowed to include prescription drug coverage. If you want prescription drug coverage, you can join a Medicare Prescription Drug Plan (Part D). If you buy Medigap and a Medicare drug plan from the same company, you may need to make 2 separate premium payments. Contact the company to find out how to pay your premiums.
Does Medigap cover everything?
Medigap policies don't cover everything. Medigap policies generally don't cover. long-term care. Services that include medical and non-medical care provided to people who are unable to perform basic activities of daily living, like dressing or bathing.
Does Medicare pay for retirees?
Read 5 things you need to know about how retiree insurance works with Medicare. If you're retired, have Medicare and have group health plan coverage from a former employer, generally Medicare pays first. Your retiree coverage pays second.
Does Medicare Supplement Insurance cover health care?
Read about Medigap (Medicare Supplement Insurance), which helps pay some of the health care costs that Original Medicare doesn't cover.
What is a medicaid supplement?
Medigap (Medicare Supplement Health Insurance) A Medigap policy is health insurance sold by private insurance companies to fill the “gaps” in Original Medicare Plan coverage. Medigap policies help pay some of the health care costs that the Original Medicare Plan doesn't cover.
What is the difference between Medigap and Medicare?
Generally, the only difference between Medigap policies sold by different insurance companies is the cost. You and your spouse must buy separate Medigap policies.Your Medigap policy won't cover any health care costs for your spouse. Some Medigap policies also cover other extra benefits that aren't covered by Medicare.
Can insurance companies sell standardized insurance?
Insurance companies can only sell you a “standardized” Medigap policy. Medigap policies must follow Federal and state laws. These laws protect you. The front of a Medigap policy must clearly identify it as “Medicare Supplement Insurance.”
Do you have to pay for Medigap?
Generally, when you buy a Medigap policy you must have Medicare Part A and Part B. You will have to pay the monthly Medicare Part B premium. In addition, you will have to pay a premium to the Medigap insurance company. As long as you pay your premium, your Medigap policy is guaranteed renewable.
Can I sell my Medicare insurance to someone under 65?
The bulletin below sets forth circumstances under which the Secretary has determined that issuers may sell individual market health insurance policies to certain Medicare beneficiaries under age 65 who lose state high risk pool coverage. As this bulletin explains, for sales to these individuals, HHS will not enforce the anti-duplication provisions of section 1882 (d) (3) (A) of the Social Security Act (the Act) from January 10, 2014 to December 31, 2015. Accompanying the bulletin are Frequently Asked Questions.
When is the best time to buy Medicare Supplement?
The best time to purchase a Medicare Supplement is during your Medicare Supplement Open Enrollment Period, which starts the first six months that you are enrolled in Medicare Part B and are 65 or older. During this period, you have the right to join any Medicare Supplement plan, regardless of pre-existing conditions or disabilities.
How does age affect Medicare premiums?
However, if you purchase a Medicare Supplement when you are first eligible, usually at the age of 65, you’ll pay less than if you had waited until you were 75.
What happens after open enrollment?
After your Open Enrollment Period is over, insurance companies may require medical underwriting (looking into your medical history to determine if they will accept you), deny you coverage, or charge you more for your premiums. Generally, you will have the most options available and the lowest costs if you join a Medicare Supplement plan when you are first eligible.
What is community rated Medicare?
There are three methods that a company can use to set rates for their Medicare Supplement policies: • Community-rated: With this pricing policy, every member, regardless of age, pays the same price. Hence, the name “Community.”. • Issue-age-rated: Your age is used for pricing, and is locked in on your policy start date.
Why do insurance companies charge more for quarterly payments?
Some companies will charge more for quarterly, semi-annual, and annual payments, because they prefer that you pay monthly. Furthermore, it is easier and more cost-effective for insurance companies to process payments paid electronically, rather than by check or credit card.
Do women get lower Medicare?
Some insurance companies offer lower rates on Medicare Supplement plans for women. According to research, women typically live longer, which means they pay more for their coverage over their lifetime. Women also tend to enjoy better health and thus claim less.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
What is a Medicare Supplement policy?
A Medicare Supplement policy, also known as Medigap, helps pays for some coinsurance, copayments, and deductibles that are not included in your Original ...
How many people can you cover with Medicare Supplement?
If you are not sure where to send your Medigap premium payment, contact your insurance provider for clarification. Remember that one Medicare supplement insurance plan covers only one person. If you want coverage for your spouse as well, you must get a separate policy.
How much is the Medigap premium for 2019?
This is an increase of $9.10 from the amount of $135.50 in 2019. Together with your Part B premium, you must pay a monthly premium to your private insurance provider for your Medigap policy. Prices vary from company to company and location plays a large role in the amount.
How old do you have to be to get Medicare Supplement?
In order to be eligible to purchase any Medicare Supplement policy, you must first be 65 years of age and enrolled in Original Medicare Part A (hospital insurance) and Part B (medical insurance). You are responsible for paying your monthly Medicare Part B premium even if you have supplemental insurance that covers other out of pocket expenses. ...
Do you pay Medicare Supplement insurance with Medicare Part B?
You do not pay this premium together with your Original Medicare Part B premium. If you are not sure where ...
Can you sell a standardized Medicare plan?
Even though plans may have a different premium cost, private insurance providers are required to follow federal and state laws and can only sell a standardized plan that provides the same benefits as anywhere else in the country . These laws are meant to protect all beneficiaries no matter where you purchase your Medigap plan. When you receive the printed copy of your plan, it must clearly state that it is Medicare Supplement insurance on the title page.
Does Medigap cover prescription drugs?
It is also important to note that Medigap policies do not include coverage for prescription drugs. You must enroll in a separate Medicare Prescription Drug Plan (Part D). Medicare Part D plans are also sold by private insurance providers that are approved by Medicare.
What happens if a provider does not accept Medicare?
Keep in mind that if a provider does not participate in Medicare's network or accepts assignment, a claims form may need to be submitted. If you paid up front, Medicare typically would reimburse you accordingly. A non-assignment provider might request the excess amount up front (up to 15% higher than what Medicare allows). These providers may file a claim on your behalf to Medicare in these situations. Ideally, use providers that accept assignment as the claims processing is extremely streamlined and your out-of-pocket expenses should be much lower depending on the Medigap plan that you have. Some Medicare supplement plans such as the F plan, cover excess and this is a big reason to consider the F plan.
How does accepting assignment affect Medicare?
First, it affects the rates that the provider will charge for a given diagnostic code since accepting assignment also means accepting Medicare's schedule of reimbursements ( or up to 15% higher if a provider chooses). The other big impact is on the claims side.
What does it mean when a provider accepts an assignment?
The term for this is that a provider accepts "assignment" which essentially means that the provider is in Medicare's network. This has two major impacts.
Does Medicare supplement work with Medigap?
First, it's important to understand how Medicare itself deals with providers and secondly, how Medigap supplements coordinate with Medicare itself. The first point depends on the status of the particular provider (doctor or hospital) in question. If the provider participates with Medicare, the claims process can be pretty smooth and coordinated.
Is Medicare a scary thing?
It's scary enough to go through a major health scare but the billing and claims side can be downright terrifying even if you have Medicare and a Medicare supplement. There can be many pages of detail with codes and descriptions that are foreign to most of us. Let's take a look at how Medicare supplement claims are processed in conjunction with Medicare itself so that we go into the paperwork tornado with a safety rope.
Does Medicare Supplement Plan pay for a procedure?
We have to be careful here. For a given medical procedure, if Medicare deems that it is not covered, the Medicare supplement plan will also not pay. The supplement looks to Medicare to determine what is eligible and then pays accordingly.
Does Medicare pay part of a covered benefit?
Medicare will pay part of a covered benefit and the supplement will pay all or part of the remaining claim. You will then get an Explanation of Benefits or an EOB showing what the total amount was, what Medicare and supplement paid, and your responsibility if any for that particular claim.
What is Medicare Supplement Insurance?
Medicare Supplement Insurance (also called Medigap) is an optional type of insurance that can be used in combination with Original Medicare (Parts A and B). A Medicare Supplement Insurance plan helps pay for out-of-pocket expenses that are associated with Original Medicare, such as deductibles, coinsurance and copayments, as well as other costs.
How old do you have to be to get Medicare Supplement?
In order to be eligible for a Medicare Supplement Insurance plan, you must meet each of the following requirements: You must be at least 65 years old or live in a state that allows Medigap coverage for people under 65 who have end-stage renal disease or a qualifying disability*.
How many types of Medigap are there?
Each of the 10 types of Medigap plans are standardized across the country in terms of coverage. In other words, a plan type sold by a company in one area of the country must offer the exact same combination of benefits as the same plan type sold by a different company in another part of the country.
When is the best time to enroll in Medigap?
The best time to enroll in Medigap is during your Medigap open enrollment period . This is a six-month period that begins the month that you are enrolled in Medicare Part B and are at least 65 years old (or qualify because of a disability or end-stage renal disease).
How to shop for insurance?
Because the prices and availability of plans can differ from one insurance company to another, the best way to shop for a plan is to compare offerings from multiple insurance companies in your area. The best way to do this is to have an agent provide you with a range of plan options and price quotes once you are age-eligible .
How can plan prices differ?
Plan prices can differ based on location. For example, the price of a plan in New York may be quite different than the cost of the very same plan sold in California, even though they offer the exact same basic benefits.
Does Medicare Supplement Insurance accept Medicare?
Any physician or facility that accepts Medicare also accepts Medicare Supplement Insurance. So as long as your provider accepts Medicare, your Medigap plan will also be accepted.
