- Directly from Medicare through electronic claims processing. This is done online.
- Directly from your provider, if he/she accepts Medicare assignment. This is done online, by fax or through the mail.
- From you. If neither Medicare nor the provider submits the claim, you will need to file the claim yourself. ...
What if Medicare denies my claim?
- Your bill will be sent directly to Medicare.
- The appeal must be filed within 120 days of receiving the Medicare Summary Notice (MSN) that shows that your claim was denied.
- If you disagree with a Medicare coverage decision in the MSN, you can appeal the decision.
What to do if Medicare denies your medical claim?
You can also take other actions to help you accomplish this:
- Reread your plan rules to ensure you are properly following them.
- Gather as much support as you can from providers or other key medical personnel to back up your claim.
- Fill out each form as carefully and exactly as possible. If necessary, ask another person to help you with your claim.
Does Medicare deny claims?
On rare occasion, Medicare may deny claims for a variety of reasons. When this happens, you will receive a Medicare denial letter to notify you that a claim was denied. There are four main types of denial letters, which differ depending on why your claim was denied.
How to get your health insurance claim processed?
- Stay organized. Keep every scrap of paper that relates to your case and have everything at your fingertips whenever you contact the insurance company. ...
- Collect names and numbers. Each time you call an insurance company representative, immediately ask for the persons name and extension. ...
- Ask for a specific timeline. ...
- Go up the food chain. ...

What are the steps in the Medicare claims process?
However, if they are unable to or simply refuse, you will need to file your own Medicare claim.Complete a Patient's Request For Medical Payment Form. ... Obtain an itemized bill for your medical treatment. ... Add supporting documents to your claim. ... 4. Mail completed form and supporting documents to Medicare.
Who processes Medicare Part A claims?
MACs are multi-state, regional contractors responsible for administering both Medicare Part A and Medicare Part B claims. MACs perform many activities including: Process Medicare FFS claims.
How long does it take for Medicare to pay claims?
For clean claims that are submitted electronically, they are generally paid within 14 calendar days by Medicare. The processing time for clean paper claims is a bit longer, usually around 30 days.
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
How do doctors bill Medicare?
If you're on Medicare, your doctors will usually bill Medicare for any care you obtain. Medicare will then pay its rate directly to your doctor. Your doctor will only charge you for any copay, deductible, or coinsurance you owe.
How do providers check Medicare claim status?
Providers can enter data via the Interactive Voice Response (IVR) telephone systems operated by the MACs. Providers can submit claim status inquiries via the Medicare Administrative Contractors' provider Internet-based portals. Some providers can enter claim status queries via direct data entry screens.
How long does Medicare take to approve?
between 30-60 daysMedicare applications generally take between 30-60 days to obtain approval.
How are Medicare claims processed?
If you have Medigap, your Medigap Plan may receive claims in one of 3 ways: Directly from Medicare through electronic claims processing. Directly from your provider, through the Internet, fax, or regular mail. This is allowed only if your provider accepts Medicare assignments.
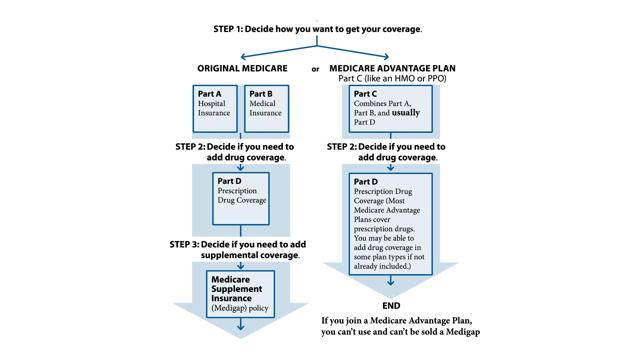
What are the four Medicare services?
In this post we will consider four Medicare Services: Original Medicare (Part A and B), the Medicare Advantage Plan (MA), the Part D Prescription Drug Plan, and Medicare Supplement (Medigap) Plan. Keep in mind that these are not exclusive and several options may coexist (e.g., Original Medicare, Part D, and Medigap).
How long does it take for Medicare to process a claim?
It takes Medicare approximately 30 days to process each claim. Medicare pays Medicare Part A claims directly to the provider (such as inpatient hospital care). You are responsible for any deductibles, copayments, and services not covered by the plan.
What happens if a provider does not accept an assignment?
If the provider does not accept the assignment, he is required to submit a claim to Medicare, and the payment will be sent to you.
How often do you get an EOB?
The same is true for Part D: the paperwork is processed internally. You will get an EOB every month showing how much you and your plan have paid for your prescriptions.
How to contact Liberty Medicare?
For help finding the best Medicare or Individual Health Plan for you, please contact Liberty Medicare or call us at 877-657-7477.
Can you file an EOB with Medicare?
This is allowed only if your provider accepts Medicare assignments. On very rare occasions, when neither Medicare nor your provider files the claim, you will need to file the claim yourself. You are supposed to get an EOB from your Medigap plan with the details of your services and the amount paid.
How long does it take for Medicare to pay?
Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn't filed within this time limit, Medicare can't pay its share. For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020.
How to file a medical claim?
Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1 The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2 The itemized bill from your doctor, supplier, or other health care provider 3 A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare 4 Any supporting documents related to your claim
What to call if you don't file a Medicare claim?
If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227) . TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got. If it's close to the end of the time limit and your doctor or supplier still hasn't filed the claim, you should file the claim.
What is an itemized bill?
The itemized bill from your doctor, supplier, or other health care provider. A letter explaining in detail your reason for submitting the claim, like your provider or supplier isn’t able to file the claim, your provider or supplier refuses to file the claim, and/or your provider or supplier isn’t enrolled in Medicare.
What happens after you pay a deductible?
After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). , the law requires doctors and suppliers to file Medicare. claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered.
When do you have to file Medicare claim for 2020?
For example, if you see your doctor on March 22, 2019, your doctor must file the Medicare claim for that visit no later than March 22, 2020. Check the "Medicare Summary Notice" (MSN) you get in the mail every 3 months, or log into your secure Medicare account to make sure claims are being filed in a timely way.
What is the form called for medical payment?
Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is 10.4 in Medicare?
10.4 - Claims Submitted for Items or Services Furnished to Medicare Beneficiaries in State or Local Custody Under a Penal Authority
What is 30.3.7 billing?
30.3.7 - Billing for Diagnostic Tests (Other Than Clinical Diagnostic
What is Medicare 40.3?
40.3 - Readmission to Medicare Program After Involuntary Termination
What is 30.2 assignment?
30.2 - Assignment of Provider’s Right to Payment
What is a 50.1.1 form?
50.1.1 - Billing Form as Request for Payment
What is CAH 30.1.1?
30.1.1 - Payment for Inpatient Services Furnished by a CAH
What is 140.1.7?
140.1.7 - Change of Ownership or Leasing
What is the purpose of 140.1.3?
140.1.3 - Verification Process Used to Determine if the Inpatient Rehabilitation Facility Met the Classification Criteria
What is 100.5 review?
100.5 - Review of Hospital Admissions of Patients Who Have Elected Hospice Care
What is 100.3 in education?
100.3 - Resident and Interns Not Under Approved Teaching Programs
What is 90.4.2 billing?
90.4.2 - Billing for Liver Transplant and Acquisition Services
What is 70.1 in medical billing?
70.1 - Providers Using All-Inclusive Rates for Inpatient Part A Charges
Who is responsible for the portion of the costs above what Medicare would usually cover?
A person would be responsible for the portion of the costs above what Medicare would usually cover, as well as any applicable out-of-pocket expenses.
How much does Medicare reimburse for out of network services?
Medicare allows out-of-network healthcare providers to charge up to 15% more than the approved amount for their services. Medicare calls this the limiting charge.
How long does a non-participating provider have to pay for a healthcare bill?
The individual will pay the full cost of the services to the healthcare provider directly. The provider has 1 year to submit a bill for their services to a Medicare Administrative Contractor on behalf of the individual.
What is Medicare certified provider?
A Medicare-certified provider: Providers can accept assignments from Medicare and submit claims to the government for payment of their services. If an individual chooses a participating provider, they must pay a 20% coinsurance.
What is a non-participating provider?
A non-participating provider: These providers have not signed an agreement with Medicare to accept assignments, but they can choose to accept individual patients. They can choose to charge more than the Medicare reimbursement amount for a particular service.
What is a copayment for Medicare?
Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
Which states require a healthcare provider to file a claim for reimbursement?
The states of Massachusetts, Minnesota, and Wisconsin standardize their plans differently. If an individual has traditional Medicare and a Medigap plan, the law requires that a healthcare provider files claims for their services. An individual should not need to file a claim for reimbursement.
What happens if a provider does not accept Medicare?
Keep in mind that if a provider does not participate in Medicare's network or accepts assignment, a claims form may need to be submitted. If you paid up front, Medicare typically would reimburse you accordingly. A non-assignment provider might request the excess amount up front (up to 15% higher than what Medicare allows). These providers may file a claim on your behalf to Medicare in these situations. Ideally, use providers that accept assignment as the claims processing is extremely streamlined and your out-of-pocket expenses should be much lower depending on the Medigap plan that you have. Some Medicare supplement plans such as the F plan, cover excess and this is a big reason to consider the F plan.
How does accepting assignment affect Medicare?
First, it affects the rates that the provider will charge for a given diagnostic code since accepting assignment also means accepting Medicare's schedule of reimbursements ( or up to 15% higher if a provider chooses). The other big impact is on the claims side.
What does it mean when a provider accepts an assignment?
The term for this is that a provider accepts "assignment" which essentially means that the provider is in Medicare's network. This has two major impacts.
Does Medigap pay for things that Medicare does not?
This is a very important concept to understand. Many people think that Medigap plans will offer "additional" benefits to traditional Medicare, meaning, it will pay for things that Medicare will not pay for. We have to be careful here.
Does Medicare supplement work with Medigap?
First, it's important to understand how Medicare itself deals with providers and secondly, how Medigap supplements coordinate with Medicare itself. The first point depends on the status of the particular provider (doctor or hospital) in question. If the provider participates with Medicare, the claims process can be pretty smooth and coordinated.
Is Medicare a scary thing?
It's scary enough to go through a major health scare but the billing and claims side can be downright terrifying even if you have Medicare and a Medicare supplement. There can be many pages of detail with codes and descriptions that are foreign to most of us. Let's take a look at how Medicare supplement claims are processed in conjunction with Medicare itself so that we go into the paperwork tornado with a safety rope.
Does Medicare Supplement Plan pay for a procedure?
We have to be careful here. For a given medical procedure, if Medicare deems that it is not covered, the Medicare supplement plan will also not pay. The supplement looks to Medicare to determine what is eligible and then pays accordingly.
When Do I Need to File A Claim?
How Do I File A Claim?
- Fill out the claim form, called the Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB). You can also fill out the CMS-1490S claim form in Spanish.
What Do I Submit with The Claim?
- Follow the instructions for the type of claim you're filing (listed above under "How do I file a claim?"). Generally, you’ll need to submit these items: 1. The completed claim form (Patient Request for Medical Payment form (CMS-1490S) [PDF, 52KB]) 2. The itemized bill from your doctor, supplier, or other health care provider 3. A letter explaining in detail your reason for subm…
Where Do I Send The Claim?
- The address for where to send your claim can be found in 2 places: 1. On the second page of the instructions for the type of claim you’re filing (listed above under "How do I file a claim?"). 2. On your "Medicare Summary Notice" (MSN). You can also log into your Medicare accountto sign up to get your MSNs electronically and view or download them anytime. You need to fill out an "Author…