
How does Medicare pay for Medigap?
Medicare doesn't pay any of the costs for you to get a Medigap policy. You have to pay the premiums for a Medigap policy. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered. information directly from Medicare. Then, they pay the doctor directly.
How do I compare Medigap rates?
Call your State Health Insurance Assistance Program (SHIP). Ask if they have a "Medigap rate comparison shopping guide" for your state. SHIPs can give you free help choosing a policy.
How are Medigap premiums priced?
Medigap policies can be priced or "rated" in 3 ways: Generally the same monthly premium is charged to everyone who has the Medigap policy, regardless of age. Your premium isn’t based on your age. Premiums may go up because of inflation and other factors, but not because of your age. Mr. Smith is 65.
What is the difference between Medigap and Medicare Advantage?
If you have a Medigap policy and join a A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, with a few exclusions, for example, certain aspects of clinical trials which are covered by Original Medicare even though you’re still in the plan.
What is considered the best Medigap plan?
Best overall Medicare Supplement plan pre-2020: Plan F 1, 2020, Plan F is the best Medigap plan. Plans will cover all the items that you would usually need to pay for out of pocket, including deductibles and coinsurance.
How are Medigap policies rated?
Attained age-rated Medigap pricing always calculates your premium based on your current age (the age you have “attained”), no matter how long you have had your policy. This means that when you first buy your policy, your premium will be based on your current age, with older people paying more.
Why is my Medicare Supplement premium so high?
CMS officials gave three reasons for the historically high premium increase: Rising prices to deliver health care to Medicare enrollees and increased use of the health care system. Some of the higher health care spending is being attributed to COVID-19 care.
Who has the best Medigap?
BCBS tied for the top score on the American Customer Satisfaction Index for health insurers. BCBS companies offer Medigap policies in all 50 states and Washington, D.C.
What is the most popular Medigap plan for 2021?
Plans F and GMedigap Plans F and G are the most popular Medicare Supplement plans in 2021. Learn more about other popular plans like Plan N and compare your Medigap plan options.
Is plan F better than plan G?
Medigap Plan G is currently outselling most other Medigap plans because it offers the same broad coverage as Plan F except for the Part B deductible, which is $233 in 2022. The only difference when you compare Medicare Supplements Plan F and Plan G is that deductible. Otherwise, they function just the same.
Do Medigap premiums increase with age?
Generally the same monthly premium is charged to everyone who has the Medigap policy, regardless of age. Your premium isn't based on your age. Premiums may go up because of inflation and other factors, but not because of your age.
What is the monthly premium for Plan G?
How much does Medicare Plan G cost? Medicare Plan G costs between $120 and $364 per month in 2022 for a 65-year-old. You'll see a range of prices for Medicare supplement policies because each insurance company uses a different pricing method for plans.
Does Medigap have an out-of-pocket maximum?
Do Medigap Plans have an Out-of-Pocket Maximum? Medigap plans don't have a maximum out-of-pocket because they don't need one. The coverage is so good you'll never spend $5,000 a year on medical bills.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
How do I choose a Medigap company?
How to Sign Up for Medigap PlansEnroll in Medicare Part A and Part B. ... Find which insurance companies in your state are licensed to sell Medigap plans by visiting Medicare.gov.Compare costs between companies. ... Select a Medigap plan that works best for you and purchase your policy.
How Much Is Medigap per month?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
What states have Medigap policies?
In Massachusetts, Minnesota, and Wisconsin, Medigap policies are standardized in a different way. Each insurance company decides which Medigap policies it wants to sell, although state laws might affect which ones they offer. Insurance companies that sell Medigap policies:
How much is Medicare deductible for 2020?
With this option, you must pay for Medicare-covered costs (coinsurance, copayments, and deductibles) up to the deductible amount of $2,340 in 2020 ($2,370 in 2021) before your policy pays anything. (Plans C and F aren't available to people who were newly eligible for Medicare on or after January 1, 2020.)
What is coinsurance in Medicare?
Coinsurance is usually a percentage (for example, 20%). The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. (unless the Medigap policy also pays the deductible).
What is covered benefits?
benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. but some offer additional benefits, so you can choose which one meets your needs.
Where do you live in Medigap?
You live in Massachusetts, Minnesota, or Wisconsin. If you live in one of these 3 states, Medigap policies are standardized in a different way. You live in Massachusetts. You live in Minnesota. You live in Wisconsin.
Do insurance companies have to offer every Medigap plan?
Insurance companies that sell Medigap policies: Don't have to offer every Medigap plan. Must offer Medigap Plan A if they offer any Medigap policy. Must also offer Plan C or Plan F if they offer any plan.
Does Medicare cover Part B?
As of January 1, 2020, Medigap plans sold to new people with Medicare aren't allowed to cover the Part B deductible. Because of this, Plans C and F are not available to people new to Medicare starting on January 1, 2020.
How long does Medigap coverage last?
This waiting period may last for up to 6 months.
What is Medicare Part A?
Medicare Part A covers some costs associated with inpatient hospital treatment, a skilled nursing facility, or hospice. Medicare Part B covers some costs associated with medically necessary outpatient services ...
What are the benefits of Medicare Supplement?
These are the benefits that may be available with a Medicare Supplement plan: 1 Coverage for Part A hospital coinsurance costs for up to 365 days once Part A’s coverage is used up. 2 Part B copayments and coinsurance amounts. 3 Coverage for the first three pints of blood if required during treatment. 4 Hospice care share-of-cost obligations with Part A. 5 Coinsurance related to a stay in a skilled nursing facility. 6 Coverage for the deductibles for Part A or Part B. 7 Excess charges not covered by Part B. 8 Medical emergencies while traveling in a foreign country.
How long does Medicare Supplement cover hospital coinsurance?
These are the benefits that may be available with a Medicare Supplement plan: Coverage for Part A hospital coinsurance costs for up to 365 days once Part A’s coverage is used up. Part B copayments and coinsurance amounts. Coverage for the first three pints of blood if required during treatment.
How long does it take to enroll in Medigap?
The initial enrollment period for a Medigap plan begins the month a recipient turns 65 and is enrolled in Part B. Recipients have a 6-month period to purchase any Medigap plan available in their state.
Which states have supplemental Medicare plans?
Some states, such as Massachusetts, Minnesota and Wisconsin, may label and regulate their supplemental plans differently. Nationally, Medicare laws can also change and that can have an impact on which Medigap plans are still valid and which may be phased out.
Does Medicare Part A cover coinsurance?
Although Medicare Part A and Part B can help cover many expenses, recipients are still obligated to pay deductibles, copayments and coinsurance amounts. A Medigap plan can help alleviate the burden of some of the costs of deductibles, coinsurance, copayment, and medical care outside of the United States. There are a variety of policies that offer ...
How long does it take to change your mind on a Medicare Select policy?
. If you buy a Medicare SELECT policy, you have the right to change your mind within 12 months and switch to a standard Medigap policy.
What is Medicare claim?
claim. A request for payment that you submit to Medicare or other health insurance when you get items and services that you think are covered. information directly from Medicare. Then, they pay the doctor directly. Some Medigap insurance companies also provide this service for Part A claims.
What is Medicare assignment?
assignment. An agreement by your doctor, provider, or supplier to be paid directly by Medicare, to accept the payment amount Medicare approves for the service, and not to bill you for any more than the Medicare deductible and coinsurance. " for all Medicare patients.
Can you charge different premiums for the same insurance?
Insurance companies may charge different premiums for the same exact policy. As you shop for a policy, be sure you're comparing the same policy. For example, compare Plan A from one company with Plan A from another company. In some states, you may be able to buy another type of Medigap policy called. Medicare Select.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). .
How long do you have to keep Medicare Advantage Plan?
If you don’t drop your Medicare Advantage Plan and return to Original Medicare within 12 months of joining, generally, you must keep your Medicare Advantage Plan for the rest of the year. You can disenroll or change plans during the Open Enrollment Period or if you qualify for a Special Enrollment Period.
Does Medigap have prescription drug coverage?
The Medigap policy can no longer have prescription drug coverage even if you had it before, but you may be able to join a. Medicare Drug Plan (Part D) Part D adds prescription drug coverage to: Original Medicare. Some Medicare Cost Plans. Some Medicare Private-Fee-for-Service Plans.
Can you get a Medigap policy back if you leave Medicare?
If you leave the Medicare Advantage Plan, you might not be able to get the same, or in some cases, any Medigap policy back unless you have a " trial right. ". If you have a Medicare Advantage Plan, it's illegal for anyone to sell you a Medigap policy unless you're switching back to. Original Medicare.
When does Medigap coverage start?
Ask for your policy to become effective when you want coverage to start. Generally, Medigap policies begin the first of the month after you apply. If, for any reason, the insurance company won't give you the effective date for the month you want, call your State Insurance Department.
How long is the open enrollment period for Medigap?
Medigap Open Enrollment Period. A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older.
How to fill out a medical application?
Tips for filling out your application 1 Fill out the application carefully and completely, including medical questions. The answers you give will determine your eligibility for open enrollment or guaranteed issue rights (also called "Medigap protections"). 2 If your insurance agent fills out the application, check to make sure it's correct. 3 Remember that the insurance company can't ask you any questions about your family history or require you to take a genetic test. 4 If you buy a Medigap policy during your#N#Medigap Open Enrollment Period#N#A one-time only, 6-month period when federal law allows you to buy any Medigap policy you want that's sold in your state. It starts in the first month that you're covered under Part B and you're age 65 or older. During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law.#N#, the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price. 5 If you provide evidence that you're entitled to a guaranteed issue right, the insurance company can't use any medical answers you give to deny you a Medigap policy or change the price.
How to pay for insurance?
How to pay for your policy. It's best to pay by check, money order, or bank draft. Make it payable to the insurance company, not the agent. If buying from an agent, get a receipt with the insurance company's name, address, and phone number for your records. Some companies may offer electronic funds transfer.
Can you be denied a Medigap policy?
During this period, you can't be denied a Medigap policy or charged more due to past or present health problems. Some states may have additional open enrollment rights under state law. , the insurance company can’t use any medical answers you give to deny you a Medigap policy or change the price.
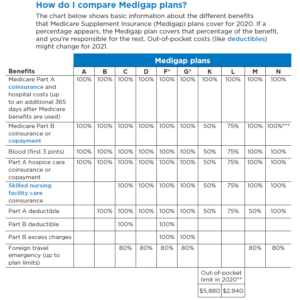
Step 1 – Decide which benefits you want, then decide which of the Medigap plans A–N meet your needs
Decide which benefits [glossary] you need and want while considering your current and future health care needs. You might not be able to switch policies later.
Step 4 – Buy the Medigap policy
Once you decide on the insurance company and the Medigap policy you want, you should apply. The insurance company must give you a clearly worded summary of your Medigap policy. Make sure you read it carefully. If you don't understand it, ask questions.
How does Medicare and Medigap work?
Medicare and Medigap work together smoothly to pay for your medical bills. It’s done automatically and usually without any input from you; that’s how Medigap policies work. That ease-of-use is a big appeal of owning a Medigap policy. Your doctors are in charge of your medical care. They know that Medicare’s rules require ...
What is the role of a Medigap insurer?
A Medigap insurer’s only role is to pay bills, bills that Medicare has already approved.
How often does Medicare send out EOB?
To help you monitor that, every three months Medicare will mail you an Explanation of Benefits (EOB) that summarizes all the bills they approved and paid on your behalf. You can also create an online Medicare account and view your bills there.
What is Medicare's rule for MRI?
They know that Medicare’s rules require that any procedure or treatment, such as surgery, a blood test or MRI, that the order is medically necessary. That means it is necessary to diagnose and treat a medical condition.
What is Medicare crossover?
After that, Medicare uses a system called “crossover” to electronically notify your Medigap insurance company that they have to pay the part of the remainder (the gaps) that your Medigap policy covers.
