Within this type of reimbursement arrangement, providers take on a portion of the risk for delivering care to their patients. For example, if a patient’s healthcare costs exceed the capitation payment, the provider is usually responsible for the remaining costs.
Full Answer
What are the major reimbursement methods used in healthcare?
Mar 23, 2020 · However, for alternative procedures, the provider can bill up to 15 percent more than the Medicare approved amount, and the bill is sent directly to the patient who will seek reimbursement from Medicare. Medicare will also only reimburse up to 95 percent of the approved amount for these procedures. Some providers may completely opt out of Medicare, …
Are you eligible for a Medicare reimbursement?
May 14, 2020 · A: Medicare reimbursement refers to the payments that hospitals and physicians receive in return for services rendered to Medicare beneficiaries. The reimbursement rates for these services are set by Medicare, and are typically less than the amount billed or the amount that a private insurance company would pay. Based on the degree to which they accept …
What to know about medical reimbursement plans?
Jul 13, 2021 · How does Medicare reimbursement work? The Centers for Medicare and Medicaid (CMS) sets reimbursement rates for all medical services and equipment covered under Medicare. When a provider accepts...
How does Medicare reimburse hospitals?
Mar 23, 2020 · If a provider is a non-participating provider, it means that they have not signed a contract with Medicare to accept the insurance company’s prices for all procedures, but they do for accept assignment for some. This is mainly due to the fact that Medicare reimbursement amounts are often lower than those received from private insurance companies.
How does Medicare affect reimbursement for healthcare services?
How does Medicare reimburse health care providers?
Does Medicare pay doctors less?
Summarizing, we do find corroborative evidence (admittedly based on physician self-reports) that both Medicare and Medicaid pay significantly less (e.g., 30-50 percent) than the physician's usual fee for office and inpatient visits as well as for surgical and diagnostic procedures.
What factors affect Medicare reimbursement?
How do reimbursements work in healthcare?
Is Medicare reimbursement taxable income?
Why do doctors not like Medicare?
Do Medicare patients get treated differently?
Which of the following expenses would be paid by Medicare Part B?
Why is reimbursement important to a healthcare organization?
What are Medicare reimbursements?
Does Medicare reimbursement increase with inflation?
What is Medicare reimbursement?
A: Medicare reimbursement refers to the payments that hospitals and physicians receive in return for services rendered to Medicare beneficiaries. The reimbursement rates for these services are set by Medicare, and are typically less than the amount billed or the amount that a private insurance company would pay.
Does Medicare pay for the entire bill?
If a Medicare beneficiary receives services from one of these doctors, the patient must pay the entire bill; Medicare will not reimburse the doctor or the patient for any portion of the bill, and the provider can set whatever fees they choose.
What is Medicare participating provider?
Physicians who agree to fully accept the rates set by Medicare are referred to as participating providers. They accept Medicare’s reimbursements for all Medicare-covered services, for all Medicare patients, and bill Medicare directly for covered services. Most eligible providers are in this category. A Kaiser Family Foundation analysis found that ...
Can a doctor opt out of Medicare?
A small number of doctors (less than 1 percent of eligible physicians) opt out of Medicare entirely, meaning that they do not accept Medicare reimbursement as payment-in-full for any services, for any Medicare patients. If a Medicare beneficiary receives services from one of these doctors, the patient must pay the entire bill;
What happens if a non-participating provider doesn't accept assignment?
If you receive treatment from a non-participating provider who doesn’t accept assignment for the treatment you receive, you may have to pay the bill up front and seek reimbursement from Medicare for the portion they’ll pay. In this case, the provider is paid 95 percent of the fee schedule amount, and can only bill you up to 15 percent more than ...
What happens if you don't accept assignment for treatment?
If you receive treatment from a non-participating provider who doesn’t accept assignment for the treatment you receive, you may have to pay the bill up front and seek reimbursement from Medicare for the portion they’ll pay.
What is Medicare reimbursement?
The Centers for Medicare and Medicaid (CMS) sets reimbursement rates for all medical services and equipment covered under Medicare. When a provider accepts assignment, they agree to accept Medicare-established fees. Providers cannot bill you for the difference between their normal rate and Medicare set fees.
Can you bill Medicare for a difference?
Providers cannot bill you for the difference between their normal rate and Medicare set fees. The majority of Medicare payments are sent to providers of for Part A and Part B services. Keep in mind, you are still responsible for paying any copayments, coinsurance, and deductibles you owe as part of your plan.
Do providers have to file a claim for Medicare?
They agree to accept CMS set rates for covered services. Providers will bill Medicare directly, and you don’t have to file a claim for reimbursement.
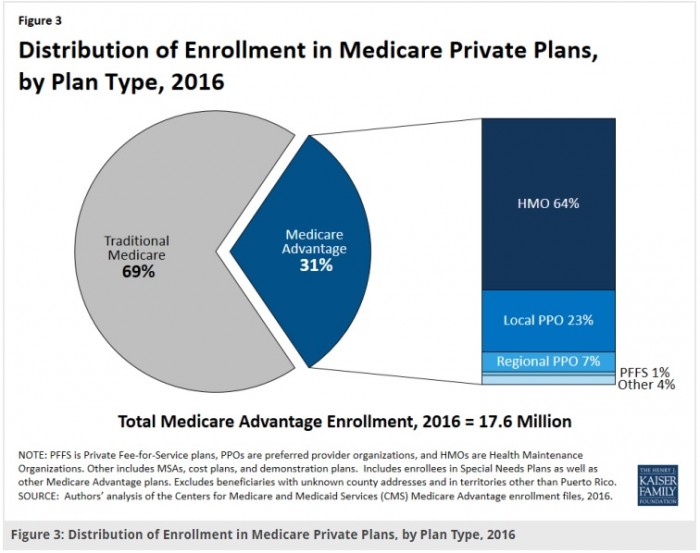
Is Medicare Advantage a private plan?
Most companies will file claims for services. Since Medicare Advantage is a private plan, you never file for reimbursement from Medicare ...
Can you file a claim with Medicare Advantage?
Most companies will file claims for services. Since Medicare Advantage is a private plan, you never file for reimbursement from Medicare for any outstanding amount. You will file a claim with the private insurance company to reimburse you if you have been billed directly for covered expenses.
What is Medicare Part D?
Medicare Part D or prescription drug coverage is provided through private insurance plans. Each plan has its own set of rules on what drugs are covered. These rules or lists are called a formulary and what you pay is based on a tier system (generic, brand, specialty medications, etc.).
How much does Medicare pay?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
Does Medicare reimburse doctors?
Medicare Reimbursement for Physicians. Doctor visits fall under Part B. You may have to seek reimbursement if your doctor does not bill Medicare. When making doctors’ appointments, always ask if the doctor accepts Medicare assignment; this helps you avoid having to seek reimbursement.
Do you have to ask for reimbursement from Medicare?
If you are in a Medicare Advantage plan, you will never have to ask for reimbursement from Medicare. Medicare pays Advantage companies to handle the claims. In some cases, you may need to ask the company to reimburse you. If you see a doctor in your plan’s network, your doctor will handle the claims process.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do doctors have to file claims for Medicare?
If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms. However, certain doctors don’t bill Medicare directly. If you want Medicare to pay for your care, you’ll need to send a form to request reimbursement.
Does Medicare cover nursing home care?
Your doctors will usually bill Medicare, which covers most Part A services at 100% after you’ve met your deductible.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Why has CMS experimented with payment methods?
The CMS has experimented with payment methods in an attempt to increase cost-effectiveness. Medicare has offered shared cost-savings incentives to reward quality care to both primary care providers and preventative services.
What is the goal of the Affordable Care Act?
Decreasing health care expenditures has been one of the main objectives of the Affordable Care Act. To achieve this goal, the Centers for Medicare and Medicaid Services (CMS) has been tasked with experimenting with provider reimbursement methods in an attempt to increase quality, while decreasing costs. The purpose of this research was ...
Can physicians negotiate reimbursement rates?
Physicians can negotiate their healthcare reimbursement rates under commercial contracts; however, they’re locked into geographically-adjusted payments from Medicare. Hospitals are paid based on diagnosis-related groups (DRG) that represent fixed amounts for each hospital stay.
How are hospitals paid?
Hospitals are paid based on diagnosis-related groups (DRG) that represent fixed amounts for each hospital stay. When a hospital treats a patient and spends less than the DRG payment, it makes a profit. When the hospital spends more than the DRG payment treating the patient, it loses money.
Do independent physicians accept insurance?
Some providers—mostly independent physicians—avoid the complex maze of healthcare reimbursement altogether by simply choosing not to accept insurance. Instead, they bill patients directly and avoid the administrative burden of submitting claims and appealing denials. Still, many providers can’t afford to do this.
What does it mean to be on multiple insurance panels?
Participating on multiple insurance panels means providers have access to a wider pool of potential patients, many of whom benefit from low-cost healthcare coverage under the Affordable Care Act. More potential patients = more potential healthcare reimbursement. When billing insurance, consider the following five steps that providers must take ...
What is EHR in healthcare?
Providers log into the electronic health record (EHR) and document important details regarding a patient’s history and presenting problem. They also document information about the exam and their thought process in terms of establishing a diagnosis and treatment plan. All of this information goes directly into the patient’s medical record where it’s stored securely and becomes the foundation for the medical necessity of the services provided.
What happens if documentation doesn't support services billed?
If documentation doesn’t support the services billed, providers may need to repay the healthcare reimbursement they received. Each of these steps takes time and resources, two of the most limited commodities in today’s provider settings.
What is EHR document?
Document the details necessary for payment. Providers log into the electronic health record (EHR) and document important details regarding a patient’s history and presenting problem. They also document information about the exam and their thought process in terms of establishing a diagnosis and treatment plan.