How do Medicare Advantage Plans work? When you join a Medicare Advantage Plan, Medicare pays a fixed amount for your coverage each month to the company offering your Medicare Advantage Plan. Companies that offer Medicare Advantage plans must follow rules set by Medicare. However, each Medicare Advantage Plan can charge different out-of-pocket costs and
Full Answer
What do you need to know about Medicare Advantage?
When you decide to switch to a new Medicare Advantage Plan or make changes to your coverage, you can do so by: Accessing Medicare's website at Medicare.gov. Contacting Medicare directly at 1-800-MEDICARE (1-800-633-4227) Contact your local SHIP (State ...
How do I know if I have Medicare Advantage?
- Review your Medicare plan coverage options. It’s a good idea to review your Medicare coverage every year to make sure the benefits of your Medicare plan remain aligned with your ...
- Make changes to your Medicare plan coverage during the right time of year. ...
- Find out what Medicare plan may fit your needs. ...
What are the advantages of Medicare Advantage?
WASHINGTON – A recent letter signed by 346 members of the U.S. House of Representatives makes the case for a “stable” Medicare Advantage program. In the letter to CMS, lawmakers urge the agency to “provide a stable rate and policy environment that ...
What companies offer Medicare Advantage plans?
What Companies Offer Medicare Advantage Plans Currently
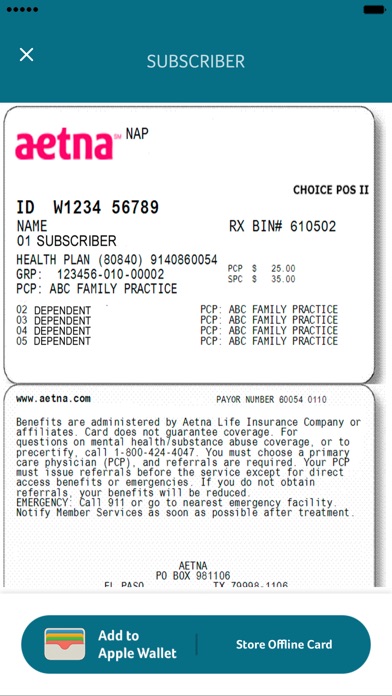
- Aetna Medicare Advantage Plans. ...
- Benefits of Aetna Medicare Advantage Plans. ...
- Blue Cross and Blue Shield Medicare Advantage Plans. ...
- Benefits of Blue Medicare Advantage Plans. ...
- Cigna Medicare Advantage Plans. ...
- Benefits of Cigna Medicare Advantage Plans. ...
- Humana Medicare Advantage Plans. ...
- Benefits of Humana Medicare Advantage Plans. ...

Can I have Medicare and Medicare Advantage at the same time?
If you join a Medicare Advantage Plan, you'll still have Medicare but you'll get most of your Part A and Part B coverage from your Medicare Advantage Plan, not Original Medicare. You must use the card from your Medicare Advantage Plan to get your Medicare- covered services.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Do Medicare Advantage Plans pay 100 %?
Medicare Advantage plans must limit how much their members pay out-of-pocket for covered Medicare expenses. Medicare set the maximum but some plans voluntarily establish lower limits. After reaching the limit, Medicare Advantage plans pay 100% of eligible expenses.
What is not covered by Medicare Advantage Plans?
Most Medicare Advantage Plans offer coverage for things Original Medicare doesn't cover, like fitness programs (like gym memberships or discounts) and some vision, hearing, and dental services. Plans can also choose to cover even more benefits.
Can you switch back to Medicare from Medicare Advantage?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
Does Medicare Advantage cover surgery?
Medicare Part B and Medicare Advantage plans generally cover physician services, including surgeons and anesthesiologists who participate in the inpatient surgery but who are not employees of the hospital.
Do I need Medicare Part D if I have an advantage plan?
Nearly 90% of Medicare Advantage plans include Medicare Part D, but you can also purchase Part D separately if you have an Advantage plan that does not include it. About a third of Medicare beneficiaries had Medicare Advantage plans in 2019.
What is the maximum out-of-pocket expense with Medicare?
Out-of-pocket limit. In 2021, the Medicare Advantage out-of-pocket limit is set at $7,550. This means plans can set limits below this amount but cannot ask you to pay more than that out of pocket.
What is the biggest difference between Medicare and Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
Why do Medicare Advantage plans have no premium?
Medicare Advantage plans are provided by private insurance companies. These companies are in business to make a profit. To offer $0 premium plans, they must make up their costs in other ways. They do this through the deductibles, copays and coinsurance.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
How long does Medicare last?
This time is known as the beginning of your Initial Enrollment Period, and it lasts for seven months.
What is original Medicare?
Original Medicare. Original Medicare is the federal program that provides your Part A and Part B coverage. Medicare Part A is responsible for covering inpatient health expenses. These could be incurred during hospital stays, inpatient procedures, stays in skilled nursing facilities, or in hospice care.
What is covered by Part B?
Part B, on the other hand, covers outpatient expenses. This coverage includes visits to your primary care physician and other specialists, outpatient procedures or testing, durable medical equipment, or any care that is used to prevent sickness or injury.
What happens if you don't apply for Medicare?
When you apply for Medicare, there are a few options to consider when selecting the plan that meets your needs.
Does Medicare Part A have a premium?
If you or your spouse has worked for at least 10 years while paying taxes, Medicare Part A is not associated with any premium payments. Part B does carry a premium payment, which is determined based on your monthly adjusted income. Medicare Part C is also known as Medicare Advantage.
Is Medicare Advantage still sponsored?
These plans are still sponsored by Medicare, but they are provided through private insurers, so they may offer additional benefits in addition to Part A and Part B coverage. Medicare Advantage plans differ from one another, so the specific costs can vary based on the benefits your plan includes .
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Why is Medicare Advantage so popular?
Medicare Advantage is a popular health insurance option because it works like private health insurance for Medicare beneficiaries. In fact, according to the Centers for Medicare & Medicaid Services, more than 60 million Americans enrolled in Medicare in 2019. Of these Medicare enrollees, more than 37 percent were enrolled in a Medicare Advantage ...
How long does it take to sign up for Medicare?
Initial enrollment period. This is a 7-month window around your 65th birthday when you can sign up for Medicare. It begins 3 months before your birth month, includes the month of your birthday, and then extends 3 months after your birthday. During this time, you can enroll for all parts of Medicare without a penalty.
Does Medicare Advantage have coinsurance?
Most Medicare Advantage plans charge a copayment or coinsurance amount for services rendered. These services could include a doctor’s office visit, specialist’s office visit, or even a prescription drug refill. Specific coinsurance and copayment amounts are set by the plan you’re enrolled in.
Does Medicare Advantage cover hospital services?
This includes any hospital services covered under Medicare Part A and any medical services covered under Medicare Part B. Some Medicare Advantage plans also cover additional healthcare needs, including: However, this coverage varies by plan, and each Medicare Advantage plan can choose what additional coverage to offer.
When is the open enrollment period for Medicare?
Open enrollment period (October 15–December 7). During this time, you can switch from original Medicare (parts A and B) to Part C (Medicare Advantage), or from Part C back to original Medicare. You can also switch Part C plans or add, remove, or change a Part D plan. General enrollment period (January 1–March 31).
Does Medicare Advantage cover prescription drugs?
Most Medicare Advantage plans include this coverage, which helps pay for the cost of your medications. Only certain types of prescription drugs are required to be covered under Part D, however — so you’ll want to make sure to check for coverage of your medications before enrolling in an Advantage plan.
Can you charge separate deductibles for Medicare Advantage?
In addition, Advantage plans can charge separate drug and health plan deductibles. Individual healthcare needs play a huge role in how much you may end up paying out of pocket for your Medicare Advantage plan. For example, your plan costs can be affected by: how often you seek services.
Where does Medicare Advantage money come from?
The money that the government pays to Medicare Advantage providers for capitation comes from two U.S. Treasury funds.
What is Medicare Advantage Reimbursement?
Understanding Medicare Advantage Reimbursement. The amount the insurance company receives from the government for you as a beneficiary is dependent upon your individual circumstances. As a beneficiary of a Medicare Advantage plan, if your monthly health care costs are less than what your insurance carrier receives as your capitation amount, ...
What is the second fund in Medicare?
The second fund is the Supplementary Medical Insurance Trust which pays for what is covered in Part B, Part D, and more. As a beneficiary enrolled in a Medicare Advantage plan, you will also be responsible for some of the costs of your healthcare.
How old do you have to be to get Medicare Advantage?
How Does Medicare Advantage Reimbursement Work? In the United States, you are eligible to enroll in a Medicare Advantage plan if you are either 65 years of age or older, are under 65 with certain disabilities.
Does Medicare Advantage cover dental?
Medicare Advantage plans must provide the same coverage as Parts A and B, but many offer additional benefits, such as vision and dental care, hearing exams, wellness programs, and Part D, prescription drug coverage.
Is Medicare Part C required?
Having a Medicare Part C plan is not a requirement for Medicare coverage, it is strictly an option many beneficiaries choose. If you decide to enroll in a Medicare Advantage plan, you are still enrolled in Medicare and have the same rights and protection that all Medicare beneficiaries have.
What is Medicare Advantage?
Medicare Advantage takes the place of original Medicare add-ons, such as Part D and Medigap. Instead of having multiple insurance plans to cover medical costs, a Medicare Advantage plan offers all your coverage in one place.
How much is Medicare 2021?
You’ll have certain set costs associated with your coverage under parts A and B. Here are some of the costs associated with original Medicare in 2021: Cost. Original Medicare amount. Part A monthly premium. $0, $259, or $471 (depending on how long you’ve worked) Part A deductible. $1,484 each benefit period.
Is Medicare a government or private insurance?
Original Medicare is a government-run option and not sold by private insurance companies. Medicare Advantage is managed and sold by private insurance companies. These companies set the prices, but Medicare regulates the coverage options. Original Medicare and Medicare Advantage are two insurance options for people age 65 and older living in ...
Does Medicare Advantage save money?
For some people, Medicare Advantage plans can help save money on long-term medical costs, while others prefer to pay for only what they need with Medicare add-ons. Below you’ll find an estimated cost comparison for some of the fees associated with Medicare Advantage in 2021: Cost. Medicare. Advantage amount.
Does Medicare cover dental and vision?
Medical services. If you’re someone who rarely visits the doctor, Medicare and Medicare add-ons may cover most of your needs. However, if you’re someone who wants coverage for yearly dental, vision, or hearing exams, many Medicare Advantage plans offer this type of coverage.
Does Medicare cover all your needs?
For example, Medicare may not cover all your needs, but a Medicare Advantage Special Needs Plan could help with long-term costs.
Do you pay Medicare premiums monthly?
If you have Medicare, you’ll pay a monthly premium for Part A (if you don’t qualify for premium-free Part A) and Part B, yearly deductibles for parts A and B, and other costs if you buy add-on coverage.
What is Medicare Advantage?
You buy Medicare Advantage plans from private health insurance companies that contract with the government. They work with Original Medicare coverage. Part D covers prescription drugs. Many Medicare Advantage plans combine Parts A, B and D in one plan. And each Medicare plan only covers one person.
Why are Medicare Advantage plans so popular?
Medicare Advantage plans are popular because of their convenience. Most plans combine medical and prescription coverage on one card. Some offer dental and vision coverage, too. And you're able to predict your out-of-pocket costs better than you can with Original Medicare.
How much does Medicare pay for coinsurance?
When you have Original Medicare, you pay 20 percent of the cost, or 20 percent coinsurance, for most medical services covered under Part B. Medicare Advantage plans use copays more than coinsurance. Which means you pay a fixed cost. You might have a $15 copay for doctor office visits, for example.
What is Medicare Part D coverage?
Medicare Part D prescription coverage has something called the coverage gap , or donut hole. The coverage gap is a stage in which you pay much more out of pocket for your prescription drugs. It's not based on a time period.
What is the difference between Medicare Supplement and Medicare Advantage?
Medicare supplement, or Medigap, plans are another option. In a way, Medicare Advantage replaces Original Medicare and connects all the pieces together on one plan. Supplement plans don't replace Original Medicare. It's more like an extra you can add on top of Original Medicare.
Does Medicare have a cap?
That means once you spend a certain amount of money on health care each year, your plan pays 100 percent of the cost of services it covers. Original Medicare doesn't have this cap. So if you get really sick, you'll end up paying a lot.
Do Medicare supplement plans come with dental?
And supplement plans don't come with the extra benefits you often get with Medicare Advantage, like dental and vision coverage. The triangles to the right show how supplement plans sit on top of Medicare Parts A, B and D. You can get complete coverage, but you still have to coordinate all those pieces on your own.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What happens when there is more than one payer?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) to pay. In some rare cases, there may also be a third payer.