Can I have dual coverage with Medicare?
Medicare and Private Insurance: Can You Have Both? It's possible to have both Medicare and private insurance. You may have both if you're covered under an employer-provided plan, COBRA, or TRICARE.
How do you determine which insurance is primary and which is secondary?
The insurance that pays first is called the primary payer. The primary payer pays up to the limits of its coverage. The insurance that pays second is called the secondary payer. The secondary payer only pays if there are costs the primary insurer didn't cover.Dec 1, 2021
Does Medicare automatically forward claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.Aug 19, 2013
Is Medicare separate from insurance?
Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance).
Is it better to have Medicare as primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Is baby automatically added to insurance?
When your baby is born, they are automatically added to your health insurance plan for the first 30 days of life*. Once your baby is born, you have two options to insure your child: add your baby to your current health insurance plan or change plans.Jun 6, 2017
Why do insurance companies ask if you have other insurance?
The carriers need to know about other coverage so they can coordinate benefits. If your wife were covered by two health insurance policies, her own policy would be her primary insurance provider and your health insurance plan would be secondary coverage.Apr 29, 2015
How does Medicare process secondary claims?
The primary insurer must process the claim in accordance with the coverage provisions of its contract. If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits.Feb 10, 2021
Will secondary insurance pay if Medicare denies?
If your primary insurance denies coverage, secondary insurance may or may not pay some part of the cost, depending on the insurance. If you do not have primary insurance, your secondary insurance may make little or no payment for your health care costs.
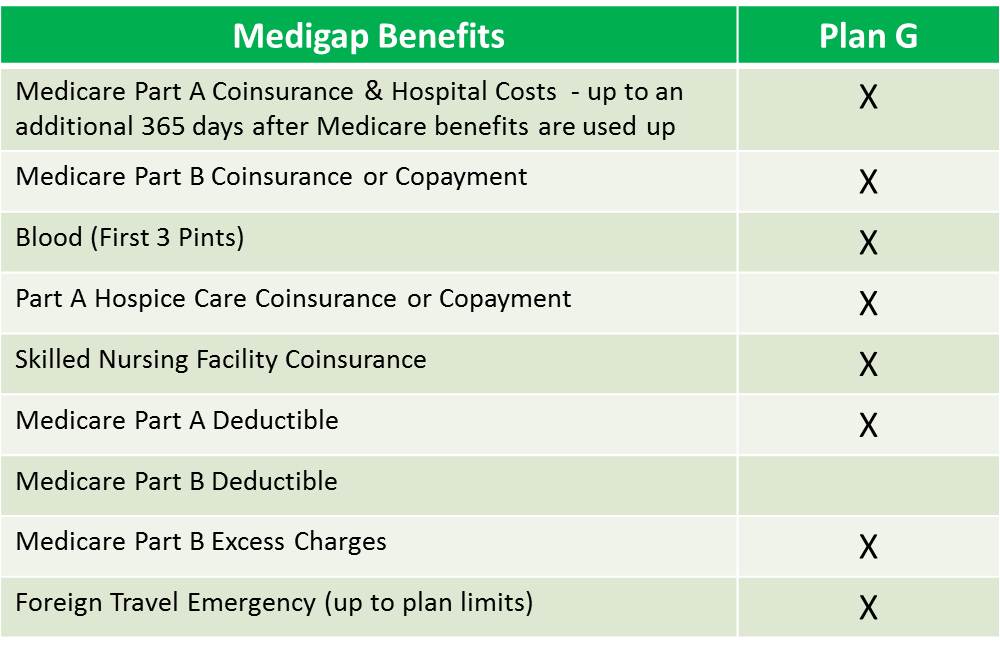
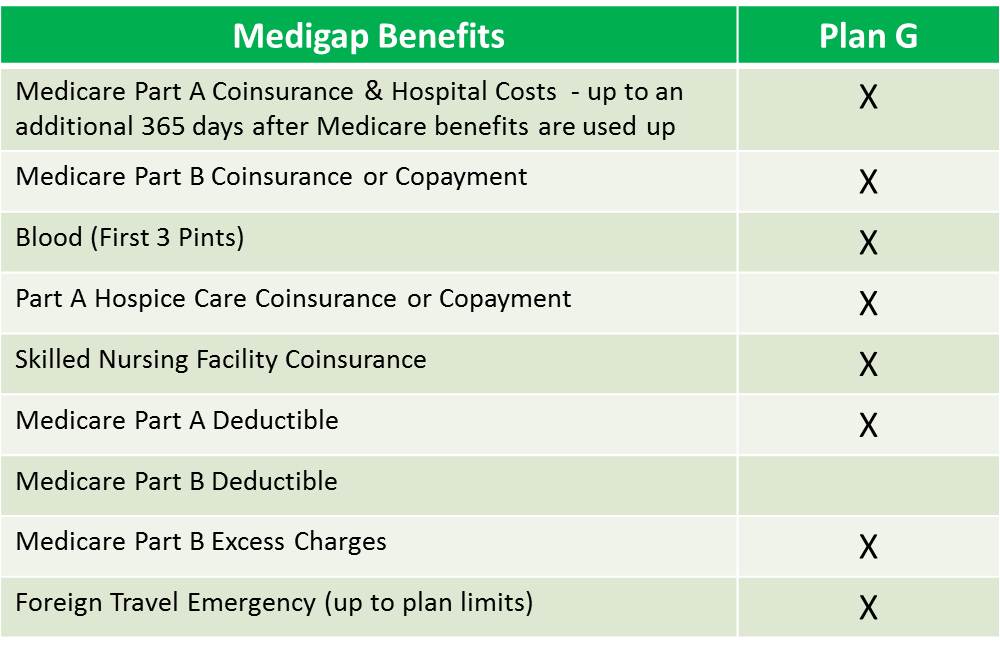
What are the negatives of a Medicare Advantage plan?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan; if you decide to switch to Medigap, there often are lifetime penalties.
What is the biggest disadvantage of Medicare Advantage?
The primary advantage is the monthly premium, which is generally lower than Medigap plans. The top disadvantages are that you must use provider networks and the copays can nickel and dime you to death.Dec 12, 2021
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
How does Medicare work?
Here's how Medicare payments work if your employer covers you: 1 If you work for a company with fewer than 20 employees, Medicare is usually considered primary and your employer is secondary. 2 If you work for a larger company, your employer is primary and Medicare is secondary. 3 If Medicare is the secondary payer, it will reimburse based on what the employer paid, what is allowed in Medicare and what the doctor or provider charged. You will then have to pay what's left over.
How does Medicare work if you work for a company?
Here's how Medicare payments work if your employer covers you: If you work for a company with fewer than 20 employees, Medicare is usually considered primary and your employer is secondary. If you work for a larger company, your employer is primary and Medicare is secondary.
What happens if you don't sign up for Part B?
If you don't sign up for Part B, you will lose TRICARE coverage. TRICARE FOR LIFE (TFL) is what TRICARE-eligible individuals have if they carry Medicare Part A and B. TFL benefits include covering Medicare's deductible and coinsurance. The exception is if you need medical attention while overseas, then TFL is primary.
What is Cobra insurance?
COBRA. COBRA lets you keep your employer group health insurance plan for a limited time after your employment ends. This continuation coverage is meant to protect you from losing your health insurance immediately after you lose a job. If you're on Medicare, Medicare pays first and COBRA is secondary.
What is a cob policy?
It's called COB, which protects insurance companies from making duplicate payments or even reimbursing for more than the healthcare services cost. Insurance providers work together to coordinate benefits and they use COB policies ...
How to decide if you have dual health insurance?
When deciding whether to have dual health insurance plans, you should run the numbers to see whether paying for two plans would be more than offset by having two insurance plans paying for medical care. If you have further questions about Medicare and COB, call Medicare at 855-798-2627.
Does Medicare cover VA?
Medicare doesn't cover services within the VA. Unlike the other scenarios on this page, there is no primary or secondary payer when it comes to VA vs. Medicare. Having both coverage gives veterans the option to get care from either VA or civilian doctors depending on the situation.
Why does Medicare send medical bills?
Since Medicare generally pays its share, medical provider s may send bills to Medicare if they don’t get compensated within a reasonable amount of time . In this case, Medicare might make a “conditional payment” to protect you from being stuck paying hefty medical bills when a claim is taking a long time.
Where does the other health plan come from?
The other health plan could come from a job, a union, a private company, or a government organization. Here’s how Medicare coordination of benefits works.
What is the difference between primary and secondary payer?
Payer: Your health insurance coverage – for example, Medicare or an employer plan. Primary payer: The health insurance that pays first, up to its limits. Secondary payer: The secondary health insurance pays then pays what the primary payer doesn’t cover, up to the secondary payer’s limits. The secondary payer might not cover all costs ...
What percentage of Medicare Part B deductible is paid?
Let’s say you have an outpatient medical bill for $1,000, and Medicare Part B is the primary payer. If you have paid your Part B deductible, it could pay 80 percent, or $800. The secondary payer may pay the other $200 if it covers the service and you’ve paid your secondary plan’s annual deductible. Like the primary payer, ...
Does Medicare pay first for a small company?
Group health insurance: You might have health insurance from an employer or a spouse’s employer. If it’s a small company with fewer than 20 employers, Medicare will usually pay first. If you have benefits from a larger employer, the employer plan typically pays first. Still, you can ask the company’s benefits department to make sure.
Can you get medicaid after Medicare?
Still, you can ask the company’s benefits department to make sure. Medicaid: Many people who have Medicare also qualify for Medicaid. In most cases, Medicaid pays after Medicare and any other health insurance you may have. Veterans’ benefits: If you have Veterans Benefits Administration (VBA) benefits, you may need to choose whether ...
Does Medicare pay for VBA?
Medicare may help pay if you don’t get services authorized or the VBA won’t cover all services. Liability insurance: Suppose you need health care because of an auto accident. Liability insurance may pay some or all of your healthcare bills. In this case, Medicare is usually the secondary payer.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
How Does Medicare Work With Group Health & Retiree Health Insurance
So I’m just back here on again, the Medicare and You PDF online version, and they have a nice little chart here, this is actually on page 21. So if you have the physical copy, and this is the 2022 version, which just came out. Again, if you don’t have this, you can get it online.
Who Pays First, Medicare or Employee Coverage?
If you’re under 65 and have a disability, have group health plan coverage based on your or a family member’s current employment, and the employer has 100 or more employees, your group health plan pays first.
How does Medicare work with insurance carriers?
Generally, a Medicare recipient’s health care providers and health insurance carriers work together to coordinate benefits and coverage rules with Medicare. However, it’s important to understand when Medicare acts as the secondary payer if there are choices made on your part that can change how this coordination happens.
Who is responsible for making sure their primary payer reimburses Medicare?
Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment. Medicare recipients are also responsible for responding to any claims communications from Medicare in order to ensure their coordination of benefits proceeds seamlessly.
What is secondary payer?
A secondary payer assumes coverage of whatever amount remains after the primary payer has satisfied its portion of the benefit, up to any limit established by the policies of the secondary payer coverage terms.
How old do you have to be to be covered by a group health plan?
Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization that shares a plan with other employers with more than 20 employees between them.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
Is ESRD covered by COBRA?
Diagnosed with End-Stage Renal Disease (ESRD) and covered by a group health plan or COBRA plan; Medicare becomes the primary payer after a 30-day coordination period. Receiving coverage through a No-Fault or Liability Insurance plan for care related to the accident or circumstances involving that coverage claim.
Does Medicare pay conditional payments?
In any situation where a primary payer does not pay the portion of the claim associated with that coverage, Medicare may make a conditional payment to cover the portion of a claim owed by the primary payer. Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment.
What happens if you have Medicare Part D and another insurance?
If someone has Medicare Part D and another insurance policy with drug coverage, there will be a coordination of benefits between the separate policy companies to determine which policy is the primary payer and which is the secondary. The determination of payments for prescription drugs will be based on the enrollee’s personal situation.
What is Medicare Part D?
Medicare Part D is Medicare’s prescription drug coverage program. Unlike Original Medicare Parts A and B, Part D plans are optional and sold by private insurance companies that contract with the federal government. Part D was enacted in 2003 as part of the Medicare Modernization Act and became operational on January 1, 2006.
What is the spending gap for Medicare Part D?
Beginning in 2020, the spending gap is reduced to a ‘standard’ co-payment of 25%, the same as required in initial spending policies. Even with the wide range of co-payments and deductibles, Medicare Part D drug coverage has proven beneficial for policy enrollees who otherwise could not afford their life-saving medications.
Is Medicare Part D private or union?
There are dozens of variables in the available Medicare Part D plans, private drug coverage plans, employer- provided plans for those still working and those retired, and union plans for those still working and those retired. Medicare Part D enrollees can benefit from a consultation with a prescription drug plan provider ...
Is Medicare the primary payer?
When Medicare Part D is the Primary Payer: • When someone is retired and enrolled in Part D while also having another health insurance policy with drug coverage, Medicare is the primary payer. The other insurance policy is the secondary payer on any remaining amount due up to the limits of the policy. If there is still any remaining unpaid amount, ...
How long does Medicare coverage last?
This special period lasts for eight months after the first month you go without your employer’s health insurance. Many people avoid having a coverage gap by signing up for Medicare the month before your employer’s health insurance coverage ends.
What is a small group health plan?
Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage a small group health plan. If your employer’s insurance covers more than 20 employees, Medicare will pay secondary and call your work-related coverage a Group Health Plan (GHP).
Does Medicare pay second to employer?
Your health insurance through your employer will pay second and cover either some or all of the costs left over. If Medicare pays secondary to your insurance through your employer, your employer’s insurance pays first. Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance ...
Does Medicare cover health insurance?
Medicare covers any remaining costs. Depending on your employer’s size, Medicare will work with your employer’s health insurance coverage in different ways. If your company has 20 employees or less and you’re over 65, Medicare will pay primary. Since your employer has less than 20 employees, Medicare calls this employer health insurance coverage ...
Does Cobra pay for primary?
The only exception to this rule is if you have End-Stage Renal Disease and COBRA will pay primary. Your COBRA coverage typically ends once you enroll in Medicare. However, you could potentially get an extension of the COBRA if Medicare doesn’t cover everything the COBRA plan does like dental or vision insurance.
Can an employer refuse to pay Medicare?
The first problem is that your employer can legally refuse to make any health-related medical payments until Medicare pays first. If you delay coverage and your employer’s health insurance pays primary when it was supposed to be secondary and pick up any leftover costs, it could recoup payments.