How Does Medicare Work?
- The basics. Established in 1965, Medicare is a federal health insurance program that provides benefits to seniors and those with disabilities and certain illnesses.
- Medicare eligibility. You or your spouse worked enough years to be eligible for Social Security or Railroad Retirement benefits.
- Enrolling in Medicare. Some people are enrolled in Medicare automatically, while others need to sign up. ...
Full Answer
What is the Medicare process and how does it work?
Services covered by Medicare must be medically necessary. Medicare also covers many preventive services, like shots and screenings. If you go to a doctor or other health care provider that accepts the Medicare-approved amount , your share of costs may be less. If you get a service that Medicare doesn’t cover, you pay the full cost.
How can you tell if someone has Medicare?
Medicare is the federal health insurance program for: People who are 65 or older Certain younger people with disabilities People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
What are the pros and cons of Medicare?
What else do I need to know about Original Medicare? You generally pay a set amount for your health care ( deductible [glossary] ) before Medicare pays its share. Then, Medicare pays its share, and you pay your share ( coinsurance / copayment ) for covered services and supplies. There's no yearly limit for what you pay out-of-pocket.
How do I get Started with Medicare?
In general, a group health plan that's sponsored jointly by 2 or more employers. , then Medicare pays first, and the group health plan pays second. If the employer has less than 20 employees, the group health plan pays first, and Medicare pays second if both of these conditions apply:

How does Medicare work in simple terms?
Do you have to pay for Medicare?
Do you automatically get Medicare with Social Security?
Does Medicare make everything free?
Who qualifies for free Medicare Part A?
Can I get Medicare Part B for free?
How long before you turn 65 do you apply for Medicare?
It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month.
How much does Medicare cost at age 62?
He can still receive Medicare Part A, but he will have to pay a monthly premium for it. In 2020, the Medicare Part A premium can be as high as $458 per month.Feb 15, 2022
Does Medicare start on birthdays?
How much does Medicare take out of Social Security?
Does Medicare cover ICU costs?
Why do doctors not like Medicare Advantage plans?
What is Medicare for?
Medicare is the federal health insurance program for: 1 People who are 65 or older 2 Certain younger people with disabilities 3 People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
Do you pay Medicare premiums if you are working?
You usually don't pay a monthly premium for Part A if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A."
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. at the start of each year, and you usually pay 20% of the cost of the Medicare-approved service, called coinsurance.
Does Medicare cover all of the costs of health care?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like copayments, coinsurance, and deductibles.
Does Medicare Advantage cover vision?
Most plans offer extra benefits that Original Medicare doesn’t cover — like vision, hearing, dental, and more. Medicare Advantage Plans have yearly contracts with Medicare and must follow Medicare’s coverage rules. The plan must notify you about any changes before the start of the next enrollment year.
Does Medicare cover prescription drugs?
Medicare drug coverage helps pay for prescription drugs you need. To get Medicare drug coverage, you must join a Medicare-approved plan that offers drug coverage (this includes Medicare drug plans and Medicare Advantage Plans with drug coverage).
What is the standard Part B premium for 2020?
The standard Part B premium amount in 2020 is $144.60. If your modified adjusted gross income as reported on your IRS tax return from 2 years ago is above a certain amount, you'll pay the standard premium amount and an Income Related Monthly Adjustment Amount (IRMAA). IRMAA is an extra charge added to your premium.
What do I need to know about Medicare?
What else do I need to know about Original Medicare? 1 You generally pay a set amount for your health care (#N#deductible#N#The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.#N#) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (#N#coinsurance#N#An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).#N#/#N#copayment#N#An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.#N#) for covered services and supplies. There's no yearly limit for what you pay out-of-pocket. 2 You usually pay a monthly premium for Part B. 3 You generally don't need to file Medicare claims. The law requires providers and suppliers to file your claims for the covered services and supplies you get. Providers include doctors, hospitals, skilled nursing facilities, and home health agencies.
Does Medicare cover health care?
The type of health care you need and how often you need it. Whether you choose to get services or supplies Medicare doesn't cover. If you do, you pay all the costs unless you have other insurance that covers it. Whether you have other health insurance that works with Medicare.
What are the factors that affect Medicare?
Factors that affect Original Medicare out-of-pocket costs 1 Whether you have Part A and/or Part B. Most people have both. 2 Whether your doctor, other health care provider, or supplier accepts assignment. 3 The type of health care you need and how often you need it. 4 Whether you choose to get services or supplies Medicare doesn't cover. If you do, you pay all the costs unless you have other insurance that covers it. 5 Whether you have other health insurance that works with Medicare. 6 Whether you have Medicaid or get state help paying your Medicare costs. 7 Whether you have a Medicare Supplement Insurance (Medigap) policy. 8 Whether you and your doctor or other health care provider sign a private contract.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. ) before Medicare pays its share. Then, Medicare pays its share, and you pay your share (. coinsurance.
What is a referral in health care?
referral. A written order from your primary care doctor for you to see a specialist or get certain medical services. In many Health Maintenance Organizations (HMOs), you need to get a referral before you can get medical care from anyone except your primary care doctor.
What is a coinsurance percentage?
Coinsurance is usually a percentage (for example, 20%). An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage.
What is a copayment?
copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is a health care provider?
Tell your doctor and other. health care provider. A person or organization that's licensed to give health care. Doctors, nurses, and hospitals are examples of health care providers. about any changes in your insurance or coverage when you get care.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
How many employees does a multi-employer plan have?
At least one or more of the other employers has 20 or more employees.
What are the requirements for Medicare?
Certain individuals under 65 are eligible for Medicare as well -- namely: 1 Anyone who's permanently disabled and has received disability benefits for at least two years. 2 Those with end-stage renal disease (ESRD). 3 Those with ALS (Lou Gehrig's disease).
What is Medicare Advantage?
Established in 1965, Medicare is a federal health insurance program that provides benefits to seniors and those with disabilities and certain illnesses. Medicare has several parts. Part A covers hospitals, nursing facilities, and home health services. Part B covers preventative services like doctor visits, diagnostic tests, and medical equipment. Part D covers prescription drugs, and Part C, also known as Medicare Advantage, offers its own additional benefits. While Part A is typically free, Parts B, C, and D come with premiums.
How old do you have to be to qualify for Medicare?
Medicare eligibility. If you're a U.S. citizen or have been a permanent legal resident for at least five years, your Medicare eligibility starts at age 65 provided you meet these requirements: You or your spouse worked enough years to be eligible for Social Security or Railroad Retirement benefits.
Who is eligible for Medicare?
Certain individuals under 65 are eligible for Medicare as well -- namely: Anyone who's permanently disabled and has received disability benefits for at least two years. Those with end-stage renal disease (ESRD). Those with ALS (Lou Gehrig's disease).
What happens if you miss your enrollment period?
If you fall into the latter category and fail to sign up during your initial enrollment period, you may be hit with a penalty. If you miss your initial enrollment period, you'll be able to sign up during the general enrollment period, which runs from Jan. 1 to March 31 each year.
Who is Maurie Backman?
Maurie Backman is a personal finance writer who's passionate about educating others. Her goal is to make financial topics interesting (because they often aren't) and she believes that a healthy dose of sarcasm never hurt anyone. In her somewhat limited spare time, she enjoys playing in nature, watching hockey, and curling up with a good book.
What happens if you join Medicare Advantage?
If you join a Medicare Advantage Plan, you still have. Medicare. Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD) .
What is Medicare Advantage Plan?
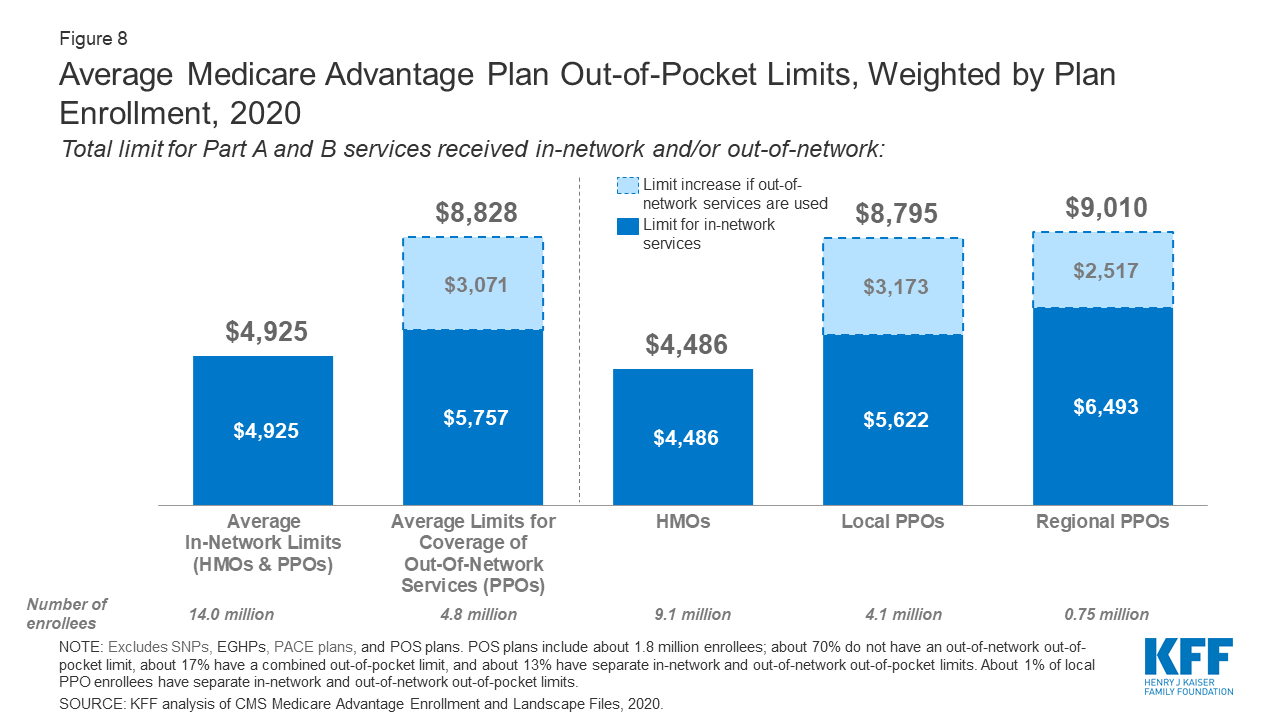
Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are an “all in one” alternative to Original Medicare. They are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, you still have. Medicare.
Does Medicare cover dental?
Covered services in Medicare Advantage Plans. Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits. For example, some plans may offer coverage for services like ...
Does Medicare Advantage cover vision?
Most Medicare Advantage Plans offer coverage for things Original Medicare doesn’t cover, like some vision, hearing, dental, and fitness programs (like gym memberships or discounts). Plans can also choose to cover even more benefits.
What happens if you don't get a referral?
If you don't get a referral first, the plan may not pay for the services. to see a specialist. If you have to go to doctors, facilities, or suppliers that belong to the plan for non-emergency or non-urgent care. These rules can change each year.
What is Medicare Supplement?
Medicare supplement insurance policies help fill in the gaps left by Original Medicare health care insurance. For many people, Medicare Supplement, also known as Medigap, insurance helps them economically by paying some of the out-of-pocket costs associated with Original Medicare.
Does Medicare Supplement pay for coinsurance?
Most supplement plans pay for Medicare copayments, coinsurance, and deductibles. But the coverage may vary according to the plan you choose. Medicare Supplement plans work together with Original Medicare. First, Medicare pays for a percentage, usually 80 percent, of the Medicare-approved cost of your health care service.
How old do you have to be to qualify for medicare?
To be eligible for Medicare, you must be at least 65 years old, a citizen of the United States or permanent legal resident for at least five consecutive years. Also, you, or your spouse, must have worked and paid federal taxes for at least ten years (or 40 quarters).
Does Medicare Supplement cover prescriptions?
They only cover one person per plan. If you want coverage for your spouse, you must purchase a separate plan. These plans also do not include prescription drug coverage.
Does Medicare cover long term care?
Most plans do not cover long-term care, vision, dental, hearing care, or private nursing care. All Medicare Supplement insurance coverage comes with a monthly premium which you pay directly to your provider. How much you pay depends on which plan you have.
Who manages Medicare?
The Centers for Medicare & Medicaid Services (CMS) manages the national Medicare program. Governing the enrollment process is a joint effort between CMS and the Social Security Administration (SSA). When you apply for Medicare benefits, the SSA is the entity that processes your application.
What is Social Security Statement?
The “Your Social Security Statement,” which is a personalized report the SSA updates annually for U.S. workers, informs individuals if they have enough credits to qualify for Medicare when turning 65. These credits reflect income earned with the potential to accrue four credits per year.
What is Lou Gehrig's disease?
Are younger than 65 and have certain permanent disabilities. Have ALS (amyotrophic lateral sclerosis), which is commonly referred to as Lou Gehrig’s disease. If you do not fall into one of the above scenarios, an application is required.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
Does Medicare pay conditional payments?
In any situation where a primary payer does not pay the portion of the claim associated with that coverage, Medicare may make a conditional payment to cover the portion of a claim owed by the primary payer. Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment.
What is secondary payer?
A secondary payer assumes coverage of whatever amount remains after the primary payer has satisfied its portion of the benefit, up to any limit established by the policies of the secondary payer coverage terms.