How would the Ryan Medicare plan pay for health insurance?
Nov 26, 2016 · Ryan has been working on his plan to change Medicare for many years. A version of his "premium support" plan was included in several budget proposals he put forth when he was chairman of the House...
Would Paul Ryan's health care plan privatize Medicare?
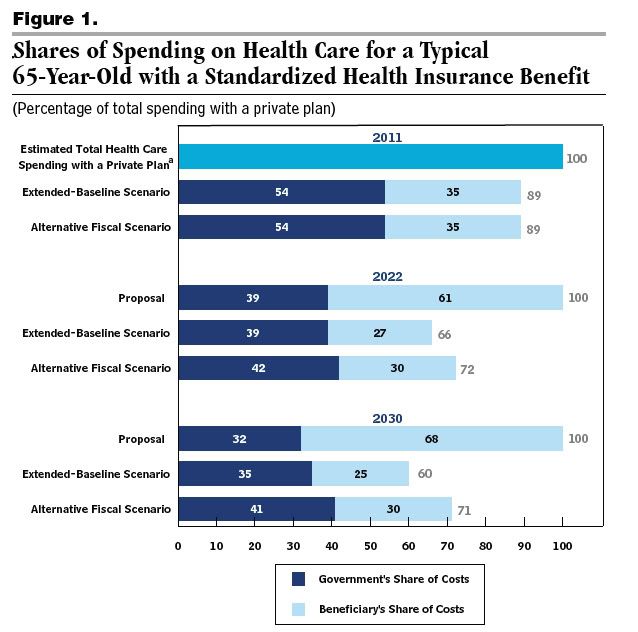
Aug 14, 2012 · The Ryan plan puts a limit on the government's Medicare spending at the rate of U.S. economic growth plus 0.5 percent. So if the economy grew at 3 percent, the maximum increase in the government’s...
What is the irony of Paul Ryan's Medicare plan?
The goal of Medicare in 1965 was to provide seniors with access to federally subsidized, low-cost healthcare. Ryan’s goal appears to be to save the government money at the expense of consumers. If Republicans Privatize Medicare. Privatization of Medicare would put an end to the government paying for healthcare for those enrolled in the program. Instead, Medicare …
Should Medicare be part of Trump's plan to replace Affordable Care Act?
Medicare eligibility age: Ryan would gradually increase the eligibility age for Medicare from 65 to nearly 67 starting in 2020. That would require those 65 to 67 to purchase commercial insurance....

What factors affect Medicare?
What are two major problems with respect to the future of Medicare?
How does Medicare affect healthcare?
Who benefits most from Medicare?
What are the disadvantages of Medicare?
- Restrictive plans can limit covered services and medical providers.
- May have higher copays, deductibles and other out-of-pocket costs.
- Beneficiaries required to pay the Part B deductible.
- Costs of health care are not always apparent up front.
- Type of plan availability varies by region.
What is the long run financial problem for Medicare?
What is the economic impact of Medicare?
Does Medicare cover all health care expenses?
Why do doctors not like Medicare Advantage plans?
What is the maximum income to qualify for Medicare?
What are the 4 types of Medicare?
- Part A provides inpatient/hospital coverage.
- Part B provides outpatient/medical coverage.
- Part C offers an alternate way to receive your Medicare benefits (see below for more information).
- Part D provides prescription drug coverage.
Is Blue Cross Blue Shield Medicare?
What would happen if Medicare was privatized?
Instead, Medicare recipients would purchase an insurance policy with their own money or with their cash benefits.
What is Medicare deregulation?
Medicare deregulation is the process of getting rid of burdensome regulations that prohibit the program from finding less expensive ways to provide coverage. For deregulation to work, however, Medicare has to be a free market, meaning it has to be privatized.
What did reform supporters say about Medicare?
Reform supporters countered that although the program was critical to millions of Medicare-eligible Americans, it could not continue without dramatic restructuring. In the end, the Affordable Care Act ...
How did the ACA reduce Medicare costs?
Cost savings through Medicare Advantage. The ACA gradually reduced costs by restructuring payments to Medicare Advantage, based on the fact that the government was spending more money per enrollee for Medicare Advantage than for Original Medicare. But implementing the cuts has been a bit of an uphill battle.
Will Medicare Advantage plan increase in 2021?
For 2021, Medicare Advantage plans will see an increase in their reimbursement rates, as was the case in 2020, 2019, 2018, and 2017.
Why did Medicare enrollment drop?
When the ACA was enacted, there were expectations that Medicare Advantage enrollment would drop because the payment cuts would trigger benefit reductions and premium increases that would drive enrollees away from Medicare Advantage plans.
How many Medicare Advantage enrollees are there in 2019?
However, those concerns have turned out to be unfounded. In 2019, there were 22 million Medicare Advantage enrollees, and enrollment in Advantage plans had been steadily growing since 2004.; Medicare Advantage now accounts for well over a third of all Medicare beneficiaries.
How many Medicare Advantage plans will be available in 2021?
For 2021, there are 21 Medicare Advantage and/or Part D plans with five stars. CMS noted that more than three-quarters of all Medicare beneficiaries enrolled in Medicare Advantage plans with integrated Part D prescription coverage would be in plans with at least four stars as of 2021.
When was Medicare Part D created?
When Medicare Part D was created in 2003, part of the legislation specifically forbid the government from negotiating drug prices with manufacturers, and that has continued to be the case. There has been considerable debate about changing this rule, but it has met with continued pushback from the pharmaceutical lobby.
When did McCain vote against the Affordable Care Act?
The dramatic vote cast by Sen. John McCain (R-Ariz.) against the Health Care Freedom Act on July 28, 2017 , which sealed the bill’s defeat, seemed to put an end to the efforts of congressional Republicans and the Trump administration to repeal and replace the Affordable Care Act (ACA).
When was the Tax Cuts and Jobs Act passed?
On Dec. 20, 2017 , H.R.1, the Tax Cuts and Jobs Act (TCJA), gained passage in the Senate and the House largely along party lines, and two days later, President Trump signed the bill into law.
What is the TCJA?
The TCJA is the biggest tax reform legislation in three decades for the United States and was unquestionably the most significant legislative accomplishment of the Trump administration in 2017.
Why did the Federation of American Hospitals oppose the TCJA?
Nonetheless, the Federation of American Hospitals, the trade association for investor-owned hospitals in the United States, opposed the TCJA primarily because of concerns about the potential adverse financial impact on hospitals of the repeal of the individual mandate, the more significant of the two provisions of the TCJA affecting health care.
Will the TCJA increase the number of uninsured Americans?
Thus, the actual extent to which the TCJA will increase the number of uninsured Americans is unclear. Of course, any rise in the number of uninsured Americans would contribute to increased uncompensated care (charity care and bad debt) for hospitals and health systems.
How much will the TCJA increase the federal debt?
According to the Joint Committee on Taxation, the TCJA will increase the federal debt by $1.0 trillion from 2018 to 2027, after taking into account increased federal revenues resulting from added economic growth. d The projected increase to the nation’s debt will put pressure on Congress to rein in federal expenditures, in turn shining a spotlight on the need to curb healthcare spending. Toward the end of 2017, Speaker of the House Paul Ryan (R-Wisc.) said, “Frankly, it’s the healthcare entitlements that are the big drivers of our debt, so we spend more time on the healthcare entitlements—because that’s really where the problem lies, fiscally speaking.” e
Why is it so hard to repeal the ACA?
Congressional Republicans found it more difficult than expected to repeal and replace the ACA primarily because of opposition to a pullback of the Medicaid expansion.
1. General Extension of Medicare Payment for Telehealth Services
Under the CARES Act, Congress gave CMS authority to waive certain limitations on Medicare coverage and payment for telehealth services furnished to Medicare beneficiaries, clearing the way for Medicare beneficiaries to receive care in their homes.
2. Telemedicine Controlled Substance Prescribing
The Ryan Haight Online Pharmacy Consumer Protection Act of 2008 (Ryan Haight Act) largely prohibits healthcare providers from prescribing controlled substances via telehealth without having previously performed an in-person medical evaluation of the patient.
3. Extension for FQHCs and RHCs
Prior to the pandemic, FQHCs and RHCs were limited to serving as an originating site (the location of the patient) for telehealth services.
4. Extension for CAHs
In March 2020, through its “ Hospitals without Walls ” program, CMS began allowing hospitals to provide services outside their hospital buildings for the duration of the public health emergency.
5. Restrictions for Certain DME and Lab Tests
The proposed legislation would require that the ordering clinician conduct an in-person exam of the patient no earlier than 12 months prior to ordering certain high-cost lab tests and high-cost DME products via telehealth.
6. Requirement to Submit NPI Number for Telehealth Billing
In order to bill Medicare directly, practitioners must register for a national provider identifier (NPI). Under certain conditions, Medicare pays for services that are billed by physicians but performed by non-physician staff acting under the supervision of the physician.
7. Study on COVID-19 Related Telehealth Changes under Medicare & Medicaid
The legislation would require HHS to study the impact of the pandemic telehealth flexibilities and deliver a report to Congress no later than 18 months after the end of the public health emergency.