Medicare Supplement plans work together with Original Medicare. First, Medicare pays for a percentage, usually 80 percent, of the Medicare-approved cost of your health care service. After this is paid, your supplement policy pays your portion of the remaining cost.
Full Answer
What are the top 5 Medicare supplement plans?
- Plan G
- Plan N
- Plan A
- Plan F
- High Deductible Plan F
How do I pick a Medicare supplement plan?
“Medicare supplements may be bought through an agent or from the carrier directly,” says Corujo. Since there’s no annual open enrollment period, you may join at any time. To buy a Medigap policy, it’s best to enroll during your Medigap Open Enrollment period, which lasts six months.
How does Medicare work with my current employer insurance?
- You will always have the choice of keeping your employer health insurance when you are eligible for Medicare if you work for a large company
- Depending on the size of your company, Medicare may be your primary or secondary insurance
- Medicare also works with COBRA, TRICARE, VA benefits, and HRAs
How much does Medicare supplement pay?
You pay coinsurance or copayment amounts in most cases. Under Part B, the coinsurance amount is usually 20% of the Medicare-approved amount. You may get some services at no cost. For example, if the Medicare-approved amount for a doctor visit is $85, your coinsurance would be around $17, if you’ve already paid your Part B deductible.

What does Medicare Supplement plan a cover?
Medicare Supplement insurance Plan A covers 100% of four things: Medicare Part A coinsurance payments for inpatient hospital care up to an additional 365 days after Medicare benefits are used up. Medicare Part B copayment or coinsurance expenses. The first 3 pints of blood used in a medical procedure.
What is the difference between Medicare and a supplemental plan?
Original Medicare pays for much, but not all, of the cost for covered health care services and supplies. A Medicare Supplement Insurance (Medigap) policy can help pay some of the remaining health care costs, like: Copayments. Coinsurance.
Do Medicare supplements pay for Part A deductible?
Most Medicare Supplement insurance plans cover the Part A deductible at least 50%. All Medicare Supplement plans also cover your Part A coinsurance and hospital costs 100% for an additional 365 days after your Medicare benefits are used up.
Is there a Medicare Supplement that covers everything?
Medicare Supplement insurance Plan F offers more coverage than any other Medicare Supplement insurance plan. It usually covers everything that Plan G covers as well as: The Medicare Part B deductible at 100% (the Part B deductible is $203 in 2021).
What are the advantages and disadvantages of Medicare Supplement plans?
Medicare Advantage offers many benefits to original Medicare, including convenient coverage, multiple plan options, and long-term savings. There are some disadvantages as well, including provider limitations, additional costs, and lack of coverage while traveling.
Can I switch from Medicare Advantage to Medicare Supplement?
Once you've left your Medicare Advantage plan and enrolled in Original Medicare, you are generally eligible to apply for a Medicare Supplement insurance plan. Note, however, that in most cases, when you switch from Medicare Advantage to Original Medicare, you lose your “guaranteed-issue” rights for Medigap.
How much does Social Security deduct for Medicare?
If your 2020 income was $91,000 to $408,999, your premium will be $544.30. With an income of $409,000 or more, you'll need to pay $578.30....Medicare Part B.Income on Individual Tax ReturnIncome on Joint Tax ReturnMonthly Premium$114,001 to $142,000$228,001 to $284,000$340.205 more rows•Feb 24, 2022
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
Why do I need Medicare Part C?
Medicare Part C provides more coverage for everyday healthcare including prescription drug coverage with some plans when combined with Part D. A Medicare Advantage prescription drug (MAPD) plan is when a Part C and Part D plan are combined. Medicare Part D only covers prescription drugs.
Does Medicare pay 100 percent of hospital bills?
According to the Centers for Medicare and Medicaid Services (CMS), more than 60 million people are covered by Medicare. Although Medicare covers most medically necessary inpatient and outpatient health expenses, Medicare reimbursement sometimes does not pay 100% of your medical costs.
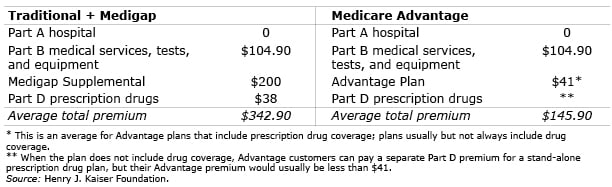
How much is Medicare Supplement monthly?
In 2020, the average premium for Medicare supplemental insurance, or Medigap, was approximately $150 per month or $1,800 per year, according to Senior Market Sales, a full-service insurance organization.
What are the top 3 most popular Medicare Supplement plans in 2021?
Three Popular Medicare Supplement PlansBlue Cross Blue Shield. According to Blue Cross Blue Shield (BCBS), Plans F and N are available in most areas. ... AARP United Healthcare. The United Healthcare Medicare Supplement plan is also very popular. ... Humana.
How many Medicare Supplement Plans are there?
These plans cover more than just out-of-pocket costs from Medicare and may provide additional benefits for some people. Currently, 10 Medicare supplement plans are available. These are:
What does "no" mean in Medicare Supplement?
“Yes” under a plan letter means that it covers 100% of the benefit. “No” under a plan letter means that it does not cover that benefit.
What is Medicare Part A and B?
Medicare parts A and B, which would serve as the primary payer, administer their coverage first . Afterward, Medigap coverage takes over to fund the out-of-pocket costs of treatment and any other agreed costs, such as treatment received outside the United States on some Medigap plans.
What is Medicare Advantage Plan?
People use Medicare Advantage plans as an alternative to Medicare parts A and B. Private companies sell and administer them, just as they do Medicare supplement plans. They provide bundled plans that may cover more than separate Medicare plans, such as dental or vision care.
What is the difference between coinsurance and deductible?
Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%.
What is a copayment for Medicare?
Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs. This article explains how Medicare supplement plans work, how to find one, and how to work out which plan is best.
Does Medicare cover all of the costs?
A person can choose to enroll in Medicare parts A and B. However, these may not cover all healthcare costs. People with Medicare will still have to pay different deductibles and coinsurances based on the type of care they receive. Medicare supplement plans can help a person reduce out-of-pocket costs on Medicare parts A and B. ...
What are Medicare Supplement Plans?
Medicare Supplement plans, also known as Medigap, are supplement insurance plans that work with Original Medicare Part A and Part B.
Who Regulates Medicare Supplement Plans?
Although Medicare Supplements (Medigap) plans are sold by private insurance companies, the federal government (CMS) regulates each plan’s design in terms of coverages offered.
How Does Medicare Supplement Plans Work?
While there are 10 Medigap plans to choose from in all but three states, each plan, although different from the next, works in the same manner. Medicare would pay its share and then the Medicare Supplement Plan would pay its share.
Which Medicare Supplement Plans Provide the Best Coverage?
Having multiple Medigap plans to choose from enables the policy shopper to select a plan that will best meet their individual needs and their individual budget. It’s also important to keep in mind that the Medigap Plan you select will have a monthly premium charge over and above your Medicare Part B premium.
What are High-Deductible Medicare Supplement Plans?
There are two high-deductible Medicare Supplement Plans available. High deductible Plan F and Plan G both have a regular version and a “high-deductible” version. Since the policyholder is agreeing to accept more out-of-pocket expenses for their annual healthcare expenses, the insurance company offers the plan at a lower monthly premium.
How does Original Medicare work?
Original Medicare covers most, but not all of the costs for approved health care services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them.
How does Medicare Advantage work?
Medicare Advantage bundles your Part A, Part B, and usually Part D coverage into one plan. Plans may offer some extra benefits that Original Medicare doesn’t cover — like vision, hearing, and dental services.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
What is a group health plan?
If the. group health plan. In general, a health plan offered by an employer or employee organization that provides health coverage to employees and their families.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
When does Medicare pay for COBRA?
When you’re eligible for or entitled to Medicare due to End-Stage Renal Disease (ESRD), during a coordination period of up to 30 months, COBRA pays first. Medicare pays second, to the extent COBRA coverage overlaps the first 30 months of Medicare eligibility or entitlement based on ESRD.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What are the benefits of Medicare Supplement?
These are the benefits that may be available with a Medicare Supplement plan: 1 Coverage for Part A hospital coinsurance costs for up to 365 days once Part A’s coverage is used up. 2 Part B copayments and coinsurance amounts. 3 Coverage for the first three pints of blood if required during treatment. 4 Hospice care share-of-cost obligations with Part A. 5 Coinsurance related to a stay in a skilled nursing facility. 6 Coverage for the deductibles for Part A or Part B. 7 Excess charges not covered by Part B. 8 Medical emergencies while traveling in a foreign country.
How long does Medicare Supplement cover hospital coinsurance?
These are the benefits that may be available with a Medicare Supplement plan: Coverage for Part A hospital coinsurance costs for up to 365 days once Part A’s coverage is used up. Part B copayments and coinsurance amounts. Coverage for the first three pints of blood if required during treatment.
How long does Medigap coverage last?
This waiting period may last for up to 6 months.
How long does a special enrollment period last?
A special enrollment period begins 60 days before a loss of coverage is expected to occur and can last up to 63 days after it happens.
How long does it take to enroll in Medigap?
The initial enrollment period for a Medigap plan begins the month a recipient turns 65 and is enrolled in Part B. Recipients have a 6-month period to purchase any Medigap plan available in their state.
What is Medicare Part A?
Medicare Part A covers some costs associated with inpatient hospital treatment, a skilled nursing facility, or hospice. Medicare Part B covers some costs associated with medically necessary outpatient services ...
Which states have supplemental Medicare plans?
Some states, such as Massachusetts, Minnesota and Wisconsin, may label and regulate their supplemental plans differently. Nationally, Medicare laws can also change and that can have an impact on which Medigap plans are still valid and which may be phased out.